Vision rehabilitation
Vision rehabilitation (often called vision rehab) is a term for a medical rehabilitation to improve vision or low vision. In other words, it is the process of restoring functional ability and improving quality of life and independence in an individual who has lost visual function through illness or injury.[1][2] Most visual rehabilitation services are focused on low vision, which is a visual impairment that cannot be fully corrected by regular eyeglasses, contact lenses, medication, or surgery. Low vision interferes with the ability to perform everyday activities.[3] Visual impairment is caused by factors including brain damage, vision loss, and others.[4] Of the vision rehabilitation techniques available, most center on neurological and physical approaches.
Background and definition
Definition of rehabilitation
Rehabilitation (literally, the act of making able again) helps patients achieve physical, social, emotional, spiritual independence and quality of life.[5] Rehabilitation does not undo or reverse the cause of damage; it seeks to promote function and independence through adaptation. Individuals can seek rehabilitation in different domains, such as motor rehabilitation after a stroke or physical rehabilitation after a car accident.[6]
Definition of low vision
Low vision is a condition where a level of vision is 20/70 or worse and it cannot be fully recovered with medical treatment, surgery, or conventional glasses.[2]
Approximately 14 million Americans suffer from low vision. The prevalence of low vision increases from 1% at age 65 to 4% at age 79, and increases dramatically to 17% after age 80. In addition, the prevalence of low vision is increasing, and depression is becoming a common issue for individuals with low vision.[7]
Low vision is different from blindness in that people with low vision have some useful sight. However, those people often have a hard time accomplishing daily tasks as their vision deteriorates (such as reading, cooking, driving, recognizing people's faces, and discerning color).[5]
| Definition | Visual activity | Visual field |
|---|---|---|
| Moderate Visual Impairment | <20/60 to 20/160 | Not considered |
| Severe Visual Impairment | ≤20/200 to 20/400 | Visual field ≤20 degrees |
| Profound Visual Impairment | <20/400 to 20/1000 | Visual field ≤10 degrees |
| Near-total Vision Loss | ≤20/1250 | |
| Total blindness | No perception of light |
Diseases that cause low vision and associated disabilities of each disease
Low vision can be caused by many diseases.[5] Though low vision mainly influences the elderly, it can appear at any stage of life. Most people develop low vision as a result of eye conditions and diseases such as macular degeneration, diabetic retinopathy, glaucoma, cataracts, retinitis pigmentosa, and stroke.
| Disease | Clinical Presentation | Associated Disabilities |
|---|---|---|
| Age-related macular degeneration | Reduced visual acuity and Loss of central vision (central scotoma) | Difficulty reading, inability to recognize faces, distortion or disappearance of central vision, reduced color vision, reduced contrast perception, mobility difficulties related to loss of depth and contrast cues. |
| Diabetic retinopathy | Reduced visual acuity, scattered central scotoma, peripheral and mid-peripheral scotoma, and macula edema | Difficulty with tasks requiring fine-detail vision such as reading, distorted central vision, fluctuating vision, loss of color perception, mobility problems due to loss of depth and contrast cues. In severe cases, total blindness can occur. |
| Glaucoma | Degeneration of the optic disc and loss of peripheral vision (constricted visual field) | Mobility and reading problems due to restricted visual fields, people suddenly appearing in the visual field. In severe cases, total blindness can occur. |
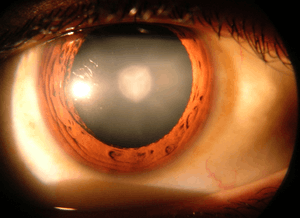
| Cataract | Reduced visual acuity, light scatter, sensitivity to glare, and image distortion | Remedied by lens extraction in 90% of cases. If not remedied, there is difficulty with detail vision, bright and changing light levels, color vision, contrast perception, and mobility related to loss of depth and contrast cues. |

Clinical studies and treatments
Since rehabilitation is becoming increasingly adopted, many researchers conduct studies pertaining to vision rehabilitation. There are many treatments for patients to choose from including training sessions, therapies, and surgeries. Most physical approaches focus on helping people by changing the environment or acquiring skills to survive in difficult situations. Neurological approaches focus on treatments that will slow the process of degradation or improve visual acuity. Psychological consulting sometimes is used because vision impairment can lead to depression.[8]
Neurological approach
There are many treatments and therapies to slow degradation of vision loss or improve the vision using neurological approaches. Studies have found that low vision can be restored to good vision.[4][9] In some cases, vision cannot be restored to normal levels but progressive visual loss can be stopped through interventions.[5]
Clinical studies of neurological approach
| Study title | Categories | Conditions |
|---|---|---|
| VA Low Vision Intervention Trials[10] | Low vision intervention | Low vision |
| The Impact of Rehabilitation on Quality of Life in Visually Impaired[11] | Procedure: blindness | Blindness |
| Safety and Efficacy of ATG003 in Patients with Wet Age-Related Macular Degeneration (AMD)[12] | Drug: mecamylamine; Drug: placebo | Macular degeneration |
| Low Vision Intervention Trail II (LOVIT II)[13] | Other: interdisciplinary low vision service; Other: basic low vision service | Central vision loss from macular diseases |
| Functional Vision in TBI[14] | Other: Vision restoration therapy; Behavioral: NVT eye scanning therapy; Behavioral: eccentric viewing training; Behavioral: sham | Visually impaired persons; brain injuries |
| The Effect of Somatosensory Cue on Postural Stability in Blinded Persons[15] | Other: observational | Visual impairment |
Chemical treatments
In general, chemical treatments are designed to slow the process of vision loss. Some research is done with neuroprotective treatment that will slow the progression of vision loss.[16] Despite other approaches existing, neuroprotective treatments seem to be most common among all chemical treatments.
Gene therapy
Gene therapy uses DNA as a delivery system to treat visual impairments. In this approach, DNA is modified through a viral vector, and then cells related to vision cease translating faulty proteins.[17] Gene therapy seems to be the most prominent field that might be able to restore vision through therapy. However, there are some problems with gene therapy which can lead to severe conditions such as death.

Physical approach
For physical approaches to vision rehabilitation, most of the training is focused on ways to make environments easier to deal with for those with low vision. Occupational therapy is commonly suggested for these patients.[18] Also, there are devices that help patients achieve higher standards of living. These include video magnifiers, peripheral prism glasses, transcranial direct current stimulation (tDCS), closed-circuit television (CCTV), RFID devices, electronic badges with emergency alert systems, virtual sound systems, and smart wheelchairs.
Clinical studies of physical approach
| Study title | Categories | Conditions |
|---|---|---|
| Clinical Trial of Peripheral Prism Glasses for Hemianopia[19] | Device: high power peripheral prism glasses, Device: low power peripheral prism glasses | Homonymous hemianopia |
| Predictors of Driving Performance and Successful Mobility - Rehabilitation in Patients with Medical Eye Condition[20] | Procedure: low vision | Low vision |
| Reading Performance with a Video Magnifier[21] | Behavioral: video camera magnifier | Macular degeneration |
| Project Magnify - A Comparison of Two Strategies to Improve Reading Ability[22] | Device: optical aids | Low vision |
| Evaluation of Eye Movement Tracking Systems for Visual Rehabilitation[23] | Procedure: visual | Blindness |
| The Use of Transcranial Direct Current Stimulation (TDCS) to Enhance the Rehabilitative Effect of Vision Restoration Therapy[24] | Behavioral: vision restoration therapy (VRT); Device: transcranial direct current stimulation (tDCS) | Hemianopia; quadrantanopia; scotoma; visual field loss |
| Low Vision Study Comparing EV Training vs. CCTV for AMD Rehabilitation[25] | Behavioral: eccentric viewing (EV) training; Device: closed-circuit television (CCTV) | AMD |
| Wayfinding Information Access System for People with Vision Loss[26] | Device: RFID device | Blindness |
| Emergency Egress and Information System for Persons with Vision Loss[27] | Device: electronic badge | Blindness |
| Restricted Useful Field View as a Risk Factor in Older Adults[28] | Procedure: prevention of falls | Visual impairment |
| Virtually Reality Mobility Training System for Veterans with Vision Loss[29] | Device: virtual sound system | Blindness |
| Vision Restoration Therapy (VRT) to Treat Non-Arteritic Anterior Ischemic Optic Neuropathy[30] | Device: vision restoration therapy (NOVAVISION) | Non-arteritic anterior ischemic optic neuropathy |
| Low Vision Depression Prevention Trial for Age Related Macular Degeneration (VITAL)[31] | Behavioral: BA-LVR; Behavioral: ST-LVR | AMD; depression |
| Improving Vision and Quality of Life in the Nursing Home[32] | Device: spectacles; Procedure: cataract surgery | Refractive error; cataract |
| Living Successfully with Chronic Eye Diseases[33] | Behavioral: low vision self-management program | Chronic diseases; low vision; diabetic retinopathy; glaucoma; AMD |
| Use of "Smart Wheelchairs" to Provide Independent Mobility to Visual and Mobility Impairments[34] | Device: Smart Power Assistance Module (SPAM); Device: Smart Wheelchair Component System (SWCS) | Blindness; wheelchair users |
| Yoga for Persons with Severe Visual Impairment (RPY)[35] | Behavioral: yoga intervention | Sleep disturbance; stress; anxiety; depression; balance impairment |
Mobility training
Mobility training improves the ability for patients with visual impairment to live independently by training patients to become more mobile.[36] For low vision patients, there are multiple mobility training methods and devices available including the 3D sound virtual reality system, talking braille, and RFID floors.
The 3D sound virtual reality system transforms sounds into locations and maps the environment.[37] This system alerts patients to avoid possible dangers. The talking braille is a device that helps low vision patients to read braille by detecting light and transmitting this information through Bluetooth technology.[38] RFID floors are GPS-like navigation systems which help patients to detect building interiors, which ultimately allow them to detour around obstacles.[39]
Home skills training
Home skills training allows patients to improve communication skills, self-care skills, cognitive skills, socialization skills, vocational training, psychological testing, and education.[40] One study indicates that multicomponent group interventions for older adults with low vision as an effective approach related to home training.[41] The multicomponent group interventions include learning new knowledge or skills each week, having multiple sessions to allow participants to apply learned knowledge or skills in their living environment, and building relationships with their health care providers.[42] The most important factor in this intervention is support from family, which includes assistance with changes in lifestyles, financial concerns, and future planning.[43]
See also
References
- ↑ Brandt Jr, E. N., & Pope, A. M. (Eds.). (1997). Enabling America: Assessing the role of rehabilitation science and engineering. National Academies Press.
- 1 2 Scheiman, M., Scheiman, M., & Whittaker, S. (2007). Low vision rehabilitation: A practical guide for occupational therapists. SLACK Incorporated.
- ↑ Liu, C.J., Brost, M.A., Horton, V.E, Kenyon, S.B., & Mears, K.E. (2013). "Occupational Therapy Interventions to Improve Performance of Daily Activities at Home for Older Adults with Low Vision:A Systematic Review". Journal of Occupational Therapy. 67 (3).
- 1 2 Fletcher, K., & Barton, J.J.S. (2012). "Vision Rehabilitation: multidisciplinary care of the patient following brain injury". Perception. 41 (10): 1287–1288. doi:10.1068/p4110rvw.
- 1 2 3 4 Vision Rehabilitation for Elderly Individuals with Low Vision or Blindness. USA: Department of Health & Human Services. 2004. p. 20.
- ↑ Ponsford, J., Sloan, S., & Snow, P. (2012). Traumatic brain injury: Rehabilitation for everyday adaptive living. Psychology Press.
- ↑ Occupational Therapy Interventions to Improve Performance of Daily Activities at Home for Older Adults With Low Vision: A Systematic Review. USA: American Journal of Occupational Therapy. 2013. pp. 279–287.
- ↑ Meadows, L. M.; Verdi, A. J.; Crabtree, B. F. (2003). "Keeping up appearances: using qualitative research to enhance knowledge of dental practice". Journal of Dental Education. 67 (9): 981–990.
- ↑ Markowitz, S. N. (2006). "Principles of modern low vision rehabilitation". Canadian Journal of Ophthalmology. 41 (3): 289–312. PMID 16767184. doi:10.1139/i06-027.
- ↑ Stelmack, J. A.; Tang, X. C.; Reda, D. J.; Rinne, S.; Mancil, R. M.; Cummings, R.; Massof, R. W. (2007). "The Veterans Affairs Low Vision Intervention Trial (LOVIT): design and methodology". Clinical Trials. 4 (6): 650–660. doi:10.1177/1740774507085274.
- ↑ The Impact of Rehabilitation on Quality of Life in Visually Impaired, http://clinicaltrials.gov/show/NCT00013403
- ↑ Safety and Efficacy of ATG003 in Patients with Wet Age-Related Macular Degeneration (AMD), http://clinicaltrials.gov/show/NCT00414206
- ↑ Low Vision Intervention Trail II (LOVIT II), http://clinicaltrials.gov/show/NCT00958360
- ↑ Functional Vision in TBI, http://clinicaltrials.gov/show/NCT01214070
- ↑ The Effect of Somatosensory Cue on Postural Stability in Blinded Persons, http://clinicaltrials.gov/show/NCT00650676
- ↑ Pardue, MT; Phillips, MJ; Yin, H; Sippy, BD; Webb-wood, S; Chow, AY; Ball, SL (2005). "Neuroprotective effect of subretinal implants in the RCS rat". Investigative Ophthalmology & Visual Science. 46: 674–682. doi:10.1167/iovs.04-0515.
- ↑ Strachan, T., & Read, A. P. (1999). Gene therapy and other molecular genetic-based therapeutic approaches.
- ↑ McGrath, C. E.; Rudman, D. L. (2013). "Factors that influence the occupational engagement of older adults with low vision: a scoping review". British Journal of Occupational Therapy. 76 (5): 234–241. doi:10.4276/030802213x13679275042762.
- ↑ Bowers AR, Keeney K, Peli E (May 2008). "Community-based trial of a peripheral prism visual field expansion device for hemianopia". Arch. Ophthalmol. 126 (5): 657–64. PMC 2396447
 . PMID 18474776. doi:10.1001/archopht.126.5.657.
. PMID 18474776. doi:10.1001/archopht.126.5.657. - ↑ Predictors of Driving Performance and Successful Mobility - Rehabilitation in Patients with Medical Eye Condition, http://clinicaltrials.gov/show/NCT00013377
- ↑ Reading Performance with a Video Magnifier, http://clinicaltrials.gov/show/NCT01670643
- ↑ Project Magnify - A Comparison of Two Strategies to Improve Reading Ability, http://clinicaltrials.gov/show/NCT00366392
- ↑ Evaluation of Eye Movement Tracking Systems for Visual Rehabilitation, http://clinicaltrials.gov/show/NCT00013429
- ↑ The Use of Transcranial Direct Current Stimulation (TDCS) to Enhance the Rehabilitative Effect of Vision Restoration Therapy, http://clinicaltrials.gov/show/NCT00921427
- ↑ Low Vision Study Comparing EV Training vs. CCTV for AMD Rehabilitation, http://clinicaltrials.gov/show/NCT00971464
- ↑ Wayfinding Information Access System for People with Vision Loss, http://clinicaltrials.gov/show/NCT00829036
- ↑ Emergency Egress and Information System for Persons with Vision Loss, http://clinicaltrials.gov/show/NCT00262509
- ↑ Restricted Useful Field View as a Risk Factor in Older Adults, http://clinicaltrials.gov/show/NCT00013351
- ↑ Virtually Reality Mobility Training System for Veterans with Vision, http://clinicaltrials.gov/show/NCT00333879
- ↑ Vision Restoration Therapy (VRT) to Treat Non-Arteritic Anterior Ischemic Optic Neuropathy, http://clinicaltrials.gov/show/NCT00140491
- ↑ Low Vision Depression Prevention Trial for Age Related Macular Degeneration (VITAL), http://clinicaltrials.gov/show/NCT00769015
- ↑ Improving Vision and Quality of Life in the Nursing Home, http://clinicaltrials.gov/show/NCT00347620
- ↑ Living Successfully with Chronic Eye Diseases, http://clinicaltrials.gov/show/NCT01879501
- ↑ Use of "Smart Wheelchairs" to Provide Independent Mobility to Visual and Mobility Impairments, http://clinicaltrials.gov/show/NCT00333762
- ↑ Yoga for Persons with Severe Visual Impairment (RPY), http://clinicaltrials.gov/show/NCT01366677
- ↑ Jeon, B.-J.; Cha (2013). "The Effects of Balance of Low Vision Patients on Activities of Daily Living". Journal of Physical Therapy Science. 25 (6): 693–696. doi:10.1589/jpts.25.693.
- ↑ Lentz, T.; Schröder, D.; Vorländer, M.; Assenmacher, I. (2007). "Virtual reality systems with integrated sound field simulation and reproduction". EURASIP Journal on Applied Signal Processing. 2007 (1): 187–187.
- ↑ Ross, D. A., & Lightman, A. (2005, October). Talking braille: a wireless ubiquitous computing network for orientation and way-finding. In Proceedings of the 7th international ACM SIGACCESS conference on Computers and accessibility (pp. 98-105). ACM.
- ↑ Mori, T., Suemasu, Y., Noguchi, H., & Sato, T. (2004, October). Multiple people tracking by integrating distributed floor pressure sensors and RFID system. In Systems, Man and Cybernetics, 2004 IEEE International Conference on (Vol. 6, pp. 5271-5278). IEEE.
- ↑ "Occupational Therapy Interventions to Promote Driving and Community Mobility for Older Adults With Low Vision: A Systematic Review". American Journal of Occupational Therapy. 67 (3): 296–302. doi:10.5014/ajot.2013.005660.
- ↑ Berger, S.; McAteer, J.; Schreier, K.; Kaldenberg, J. (2013). "Occupational Therapy Interventions to Improve Leisure and Social Participation for Older Adults With Low Vision: A Systematic Review". American Journal of Occupational Therapy. 67 (3): 303–311. doi:10.5014/ajot.2013.005447.
- ↑ Smallfield, S.; Clem, K.; Myers, A. (2013). "Occupational Therapy Interventions to Improve the Reading Ability of Older Adults With Low Vision: A Systematic Review". American Journal of Occupational Therapy. 67 (3): 288–295. doi:10.5014/ajot.2013.004929.
- ↑ O'Connor, P. M.; Lamoureux, E. L.; Keeffe, J. E. (2008). "Predicting the need for low vision rehabilitation services". British Journal of Ophthalmology. 92 (2): 252–255. doi:10.1136/bjo.2007.125955.