Urinary system
| Urinary System | |
|---|---|
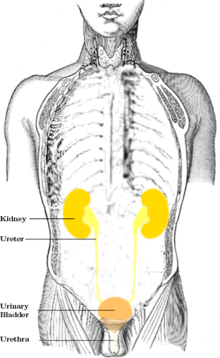
 1. Human urinary system: 2. Kidney, 3. Renal pelvis, 4. Ureter, 5. Urinary bladder, 6. Urethra. (Left side with frontal section) 7. Adrenal gland Vessels: 8. Renal artery and vein, 9. Inferior vena cava, 10. Abdominal aorta, 11. Common iliac artery and vein With transparency: 12. Liver, 13. Large intestine, 14. Pelvis The order of impurities being excreted from the kidneys: Kidneys → Ureters → Urinary Bladder → Urethra | |
| Details | |
| Identifiers | |
| Latin | Systema urinarium |
| TA | A08.0.00.000 |
| FMA | 7159 |
The urinary system, also known as the renal system, consists of the kidneys, ureters, bladder, and the urethra. Each kidney consists of millions of functional units called nephrons. The purpose of the renal system is to eliminate wastes from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Following filtration of blood and further processing, wastes (in the form of urine) exit the kidney via the ureters, tubes made of smooth muscle fibers that propel urine towards the urinary bladder, where it is stored and subsequently expelled from the body by urination (voiding). The female and male urinary system are very similar, differing only in the length of the urethra.[1]
Urine is formed in the kidneys through a filtration of blood. The urine is then passed through the ureters to the bladder, where it is stored. During urination, the urine is passed from the bladder through the urethra to the outside of the body.
800–2,000 milliliters (mL) of urine are normally produced every day in a healthy human. This amount varies according to fluid intake and kidney function.
Structure
The urinary system refers to the structures that produce and conduct urine to the point of excretion. The human body normally has two paired kidneys, one on the left and one on the right. Urine is formed by nephrons, the functional unit of the kidney, and then flows through a system of converging tubules called collecting ducts. The collecting ducts join together to form minor calyces, then major calyces, which ultimately join the pelvis of the kidney (renal pelvis). Urine flows from the renal pelvis into the ureter, a tube-like structure that carries the urine from the kidneys into the bladder.
During urination, urine stored in the bladder is discharged through the urethra. In males, the urethra begins at the internal urethral orifice in the trigone of the bladder, continues through the external urethral orifice, and then becomes the prostatic, membranous, bulbar, and penile urethra. Urine exits through the external urethral meatus. The female urethra is much shorter, beginning at the bladder neck and terminating in the vaginal vestibule.
Development
Histology
Under microscopy, the urinary system is covered in a unique lining called urothelium, a type of transitional epithelium. Unlike the epithelial lining of most organs, transitional epithelium can flatten and distend. Urothelium covers most of the urinary system, including the renal pelvis, ureters, and bladder.
Function
There are several functions of the Urinary System:
- Removal of waste product from the body (mainly urea and uric acid)
- Regulation of electrolyte balance (e.g. sodium, potassium and calcium)
- Regulation of acid-base homeostasis
- Controlling blood volume and maintaining blood pressure
Urine formation
Average urine production in adult humans is about 1–2 litres (L) per day, depending on state of hydration, activity level, environmental factors, weight, and the individual's health. Producing too much or too little urine requires medical attention. Polyuria is a condition of excessive urine production (> 2.5 L/day). Oliguria when < 400 mL (millilitres) are produced, and anuria one of < 100 mL per day.
The first step in urine formation is the filtration of blood in the kidneys. In a healthy human the kidney receives between 12 and 30% of cardiac output, but it averages about 20% or about 1.25 L/min.
The basic structural and functional unit of the kidney is the nephron. Its chief function is to regulate the concentration of water and soluble substances like sodium by filtering the blood, reabsorbing what is needed and excreting the rest as urine.
In the first part of the nephron, Bowman's capsule filters blood from the circulatory system into the tubules. Hydrostatic and osmotic pressure gradients facilitate filtration across a semipermeable membrane. The filtrate includes water, small molecules, and ions that easily pass through the filtration membrane. However larger molecules such as proteins and blood cells are prevented from passing through the filtration membrane. The amount of filtrate produced every minute is called the glomerular filtration rate or GFR and amounts to 180 litres per day. About 99% of this filtrate is reabsorbed as it passes through the nephron and the remaining 1% becomes urine.
The urinary system is regulated by the endocrine system by hormones such as antidiuretic hormone, aldosterone, and parathyroid hormone.[2]
Regulation of concentration and volume
The urinary system is under influence of circulatory system, nervous system and endocrine system.
Aldosterone plays a central role in regulating blood pressure through its effects on the kidney. It acts on the distal tubules and collecting ducts of the nephron and increases reabsorption of sodium from the glomerular filtrate. Reabsorption of sodium results in retention of water, which increases blood pressure and blood volume. Antidiuretic hormone (ADH), is a neurohypophysial hormone found in most mammals. Its two primary functions are to retain water in the body and to constrict blood vessels. Vasopressin regulates the body's retention of water by increasing water reabsorption in the collecting ducts of the kidney nephron.[3] Vasopressin increases water permeability of the kidney's collecting duct and distal convoluted tubule by inducing translocation of aquaporin-CD water channels in the kidney nephron collecting duct plasma membrane.[4]
Urination
Urination is the ejection of urine from the urinary bladder through the urethra to the outside of the body. In healthy humans (and many other animals), the process of urination is under voluntary control. In infants, some elderly individuals, and those with neurological injury, urination may occur as an involuntary reflex. Physiologically, micturition involves coordination between the central, autonomic, and somatic nervous systems. Brain centers that regulate urination include the pontine micturition center, periaqueductal gray, and the cerebral cortex. In placental mammals the male ejects urine through the penis, and the female through the vulva.
Clinical significance
Urologic disease can involve congenital or acquired dysfunction of the urinary system.
Diseases of the kidney tissue are normally treated by nephrologists, while disease of the urinary tract are treated by urologists. Gynecologists may also treat female urinary incontinence.
Diseases of other bodily systems also have a direct effect on urogenital function. For instance it has been shown that protein released by the kidneys in diabetes mellitus sensitises the kidney to the damaging effects of hypertension.[5]
Diabetes also can have a direct effect in urination due to peripheral neuropathies which occur in some individuals with poorly controlled diabetes.[6]
Urinary incontinence can result from a weakening of the pelvic floor muscles caused by factors such as pregnancy, childbirth, aging and being overweight. Pelvic floor exercises known as Kegel exercises can help in this condition by strengthening the pelvic floor. There can also be underlying medical reasons for urinary incontinence which are often treatable. In children the condition is called enuresis.
See also
References
- ↑ C. Dugdale, David (16 September 2011). "Female urinary tract". MedLine Plus Medical Encyclopedia.
- ↑ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1.
- ↑ Caldwell HK, Young WS III, Lajtha A, Lim R (2006). "Oxytocin and Vasopressin: Genetics and Behavioral Implications" (PDF). Handbook of Neurochemistry and Molecular Neurobiology: Neuroactive Proteins and Peptides (3rd ed.). Berlin: Springer. pp. 573–607. ISBN 0-387-30348-0.
- ↑ Nielsen S, Chou CL, Marples D, Christensen EI, Kishore BK, Knepper MA (February 1995). "Vasopressin increases water permeability of kidney collecting duct by inducing translocation of aquaporin-CD water channels to plasma membrane". Proc. Natl. Acad. Sci. U.S.A. 92 (4): 1013–7. PMC 42627
 . PMID 7532304. doi:10.1073/pnas.92.4.1013.
. PMID 7532304. doi:10.1073/pnas.92.4.1013. - ↑ Baba, T; Murabayashi, S; Tomiyama, T; Takebe, K (1990). "Uncontrolled hypertension is associated with a rapid progression of nephropathy in type 2 diabetic patients with proteinuria and preserved renal function". The Tohoku journal of experimental medicine. 161 (4): 311–8. PMID 2256104. doi:10.1620/tjem.161.311.
- ↑ "Peripheral Neuropathy". Patient UK. Retrieved 2014-03-20.
External links
| The Wikibook Human Physiology has a page on the topic of: The Urinary System |
| The Wikibook Anatomy and Physiology of Animals has a page on the topic of: Urinary System |
| Library resources about Urinary system |