Pelvic organ prolapse
| Pelvic organ prolapse | |
|---|---|
| Synonyms | Female genital prolapse |
| Classification and external resources | |
| Specialty | Gynecology |
| ICD-10 | N81 |
| ICD-9-CM | 618 |
| DiseasesDB | 25265 |
| MeSH | D014596 |
Pelvic organ prolapse (POP), also known as female genital prolapse, is characterized by descent of female genital organs beyond their normal anatomical confines. The condition usually occurs when the pelvic floor collapses as a result of childbirth or heavy lifting which can tear soft tissues, i.e. herniating fascia membranes so that the vaginal wall collapses, resulting in cystocele, rectocele or both. Remediation typically involves dietary and lifestyle changes, physical therapy, or surgery.
Types
anterior vaginal wall prolapse
Cystocele (bladder into vagina)
- Urethrocele (urethra into vagina)
- cystourethrocele (both bladder and urethra)
- posterior vaginal wall prolapse
- Enterocele (small intestine into vagina)
- Rectocele (rectum into vagina)
- apical vaginal prolapse
- Uterine prolapse (uterus into vagina)
- Vaginal vault prolapse (roof of vagina) - after hysterectomy
The term uterovaginal prolapse is sometimes defined as any or several of the above,[1] and sometimes as uterine prolapse specifically.[2]
Grading
Pelvic organ prolapses are graded either via the Baden-Walker System, Shaw's System, or the Pelvic Organ Prolapse Quantification (POP-Q) System.[3]
Shaw's System
Anterior wall
- Upper 2/3 cystocele
- Lower 1/3 urethrocele
Posterior wall
- Upper 1/3 enterocele
- Middle 1/3 rectocele
- Lower 1/3 deficient perenium
Uterine prolapse
- Grade 0 Normal position
- Grade 1 descent into vagina not reaching introitus
- Grade 2 descent up to the introitus
- Grade 3 descent outside the introitus
- Grade 4 Procidentia
Baden-Walker
| Grade | posterior urethral descent, lowest part other sites |
|---|---|
| 0 | normal position for each respective site |
| 1 | descent halfway to the hymen |
| 2 | descent to the hymen |
| 3 | descent halfway past the hymen |
| 4 | maximum possible descent for each site |
POP-Q
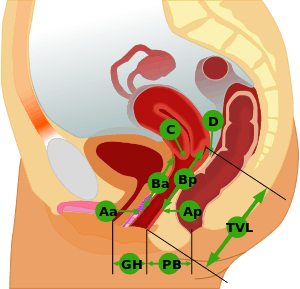
| Stage | description |
|---|---|
| 0 | No prolapse anterior and posterior points are all -3 cm, and C or D is between -TVL and -(TVL-2) cm. |
| 1 | The criteria for stage 0 are not met, and the most distal prolapse is more than 1 cm above the level of the hymen (less than -1 cm). |
| 2 | The most distal prolapse is between 1 cm above and 1 cm below the hymen (at least one point is -1, 0, or +1). |
| 3 | The most distal prolapse is more than 1 cm below the hymen but no further than 2 cm less than TVL. |
| 4 | Represents complete procidentia or vault eversion; the most distal prolapse protrudes to at least (TVL-2) cm. |
Management
Vaginal prolapses are treated according to the severity of symptoms. They can be treated:
- With conservative measures (changes in diet and fitness, Kegel exercises, pelvic floor physical therapy.)
- With a pessary, a rubber or silicon device fitted to the patient which is inserted into the vagina and may be retained for up to several months. Pessaries are a good choice of treatment for women who wish to maintain fertility, are poor surgical candidates, or who may not be able to attend physical therapy.[4] Pessaries require a provider to fit the device, but most can be removed, cleaned, and replaced by the woman herself. Pessaries should be offered to women considering surgery as a non-surgical alternative.
- With surgery (for example native tissue repair, biological graft repair, absorbable and non-absorbable mesh repair, colpopexy, colpocleisis). Surgery is used to treat symptoms such as bowel or urinary problems, pain, or a prolapse sensation. According to the Cochrane Collaboration review (2016)[5] current evidence does not support the use of transvaginal surgical mesh repair compared with native tissue repair for anterior compartment prolapse owing to increased morbidity. Safety and efficacy of many newer meshes is unknown[5]. The use of a transvaginal mesh in treating vaginal prolapses is associated with side effects including pain, infection, and organ perforation. According to the FDA, serious complications are "not rare."[6] A number of class action lawsuits have been filed and settled against several manufacturers of TVM devices.[7]
Epidemiology
Genital prolapse occurs in about 316 million women worldwide as of 2010 (9.3% of all females).[8]
See also
References
- ↑ Vierhout ME (December 2004). "[Diagnosis of uterovaginal prolapse]". Ned Tijdschr Geneeskd (in Dutch and Flemish). 148 (49): 2432–6. PMID 15626307.
- ↑ Monga, Ash (2011). Gynaecology. London: Hodder/Arnold. ISBN 0-340-98354-X.
- ↑ "ACOG Practice Bulletin No. 85: Pelvic organ prolapse". Obstet Gynecol. 110 (3): 717–29. September 2007. PMID 17766624. doi:10.1097/01.AOG.0000263925.97887.72.
- ↑ "Practice Bulletin No. 176". Obstetrics & Gynecology. 129 (4): e56–e72. 2017-04-01. ISSN 1873-233X. doi:10.1097/aog.0000000000002016.
- 1 2 Maher, Christopher; Feiner, Benjamin; Baessler, Kaven; Christmann-Schmid, Corina; Haya, Nir; Brown, Julie (2016-11-30). "Surgery for women with anterior compartment prolapse". The Cochrane Database of Systematic Reviews. 11: CD004014. ISSN 1469-493X. PMID 27901278. doi:10.1002/14651858.CD004014.pub6.
- ↑ "UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse: FDA Safety Communication". U.S. Food and Drug Administration. 13 July 2011. Retrieved 23 June 2015.
- ↑ "Women Implanted with Transvaginal Mesh Suffer from Painful, Permanent Injuries". Parker Waichman LLP. Retrieved 23 June 2015.
- ↑ Vos, T (Dec 15, 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010.". Lancet. 380 (9859): 2163–96. PMID 23245607. doi:10.1016/S0140-6736(12)61729-2.