Transurethral resection of the prostate
| Transurethral resection of the prostate | |
|---|---|
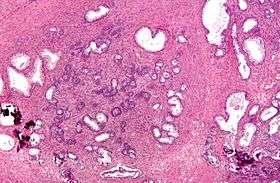 Micrograph of a transurethral resection of the prostate (TURP) specimen, showing BPH (nodular hyperplasia of the prostate) - left-of-center in image. H&E stain. | |
| ICD-9-CM | 60.29 |
| MeSH | D020728 |
| MedlinePlus | 002996 |
Transurethral resection of the prostate (commonly known as a TURP, plural TURPs, and rarely as a transurethral prostatic resection, TUPR) is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. This is considered the most effective treatment for BPH. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80-90% of BPH patients.
Indications
BPH is normally initially treated medically. This is done through alpha antagonists such as tamsulosin or 5-alpha-reductase inhibitors such as finasteride and dutasteride. If medical treatment does not reduce a patient's urinary symptoms, a TURP may be considered following a careful examination of the prostate/bladder through a cystoscope. If TURP is contraindicated a urologist may consider a simple prostatectomy, in and out catheters, or a supra-pubic catheter to help a patient void urine effectively.[1] As medical management of BPH improves, the numbers of TURPs have been decreasing.
Types of TURP
Traditionally, a cystoscope [a resectoscope which has a 30-degree viewing angle, along with resectoscopy sheath & working element] has been used to perform TURP. The scope is passed through the urethra to the prostate where surrounding prostate tissue can then be excised.
A monopolar device utilizing a wire loop with electric current flowing in one direction (thus monopolar) can be used to excise tissue via the resectoscope. A grounding ESU pad and irrigation by a nonconducting fluid is required to prevent this current from disturbing surrounding tissues. This fluid (usually glycine) can cause damage to surrounding tissue after prolonged exposure, resulting in TUR syndrome, so surgery time is limited.
TURP using a bipolar device is a newer technique that uses bipolar current to remove the tissue.[6] [7] Bipolar TURP allows saline irrigation and eliminates the need for an ESU grounding pad thus preventing post-TURP hyponatremia (TUR syndrome) and reducing other complications. As a result, bipolar TURP is also not subject to the same surgical time constraints of conventional TURP.
Another transurethral method utilizes laser energy to remove tissue. With laser prostate surgery a fiber optic cable pushed through the urethra is used to transmit lasers such as holmium-Nd:YAG high powered "red" or potassium titanyl phosphate (KTP) "green" to vaporize the adenoma. More recently the KTP laser has been supplanted by a higher power laser source based on a lithium triborate crystal, though it is still commonly referred to as a "Greenlight" or KTP procedure. The specific advantages of utilizing laser energy rather than a traditional electrosurgical TURP is a decrease in the relative blood loss, elimination of the risk of post-TURP hyponatremia (TUR syndrome), the ability to treat larger glands, as well as treating patients who are actively being treated with anti-coagulation therapy for unrelated diagnoses.
Risks
Because of bleeding risks associated with the surgery, TURP is not considered safe for many patients with cardiac problems.
Postoperative complications include [2]
- Bleeding (most common). Bleeding may be reduced by pre-treatment with an anti-androgen such as finasteride[3][4][5] or flutamide.
- Clot retention and clot colic
- Bladder wall injury such as perforation (rare)
- TURP Syndrome: Hyponatremia and water intoxication (symptoms resembling brain stroke in an elderly presenting patient) caused by an overload of fluid absorption (e.g. 3 to 4 Litres) from the open prostatic sinusiods during the procedure. This complication can lead to confusion, changes in mental status, vomiting, nausea, and even coma. To prevent TURP syndrome the 1) length of the procedure is limited to less than one hour in many centers, and 2) the height of the container of irrigating solution above the surgical table determining the hydrostatic pressure driving fluid into the prostatic veins and sinuses is kept to a minimum.[6]
- Bladder neck stenosis
- Urinary incontinence due to injury of external sphincter system which may be prevented by taking the Verumontanum of the prostate as a distal limiting boundary during TURP
- Retrograde ejaculation due to injury of preprostatic (internal) sphincter system. This is one of the most frequent complications of the procedure.
Additionally, transurethral resection of the prostate is associated with a low risk of mortality.
See also
- Transurethral needle ablation of the prostate
- Transurethral incision of the prostate
- Prostatectomy, describes monopolar and bipolar [electrocautery] TURP
- Prostatic stent
- prostate artery embolisation, alternative to TURP for BHP
References
- ↑ Collins, MD; Chief Editor: Edward David Kim, MD Transurethral Resection of the Prostate Medscape:
- ↑ Rassweiler J, Teber D, Kuntz R, Hofmann R (November 2006). "Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention". Eur. Urol. 50 (5): 969–79; discussion 980. PMID 16469429. doi:10.1016/j.eururo.2005.12.042.
- ↑ Ö L Özdal, C Özden, K Benli, S Gökkaya, S Bulut and A Memis cedil Effect of short-term finasteride therapy on peroperative bleeding in patients who were candidates for transurethral resection of the prostate (TUR-P): a randomized controlled study Prostate Cancer and Prostatic Diseases (2005) 8, 215–218. doi:10.1038/sj.pcan.4500818; published online 5 July 2005 pubmed 15999118 http://www.nature.com/pcan/journal/v8/n3/full/4500818a.html
- ↑ LI Ming-xiong,TANG Zheng-yan,SU Jian,et al. Effect of Finasteride on Perioperative and Postoperative Bleeding Following Transurethral Resection of Prostate http://en.cnki.com.cn/Article_en/CJFDTOTAL-SYYY200903092.htm DOI CNKI:SUN:SYYY.0.2009-03-092
- ↑ Rassweiler J, Teber D, Kuntz R, Hofmann R (November 2006). "Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention". Eur. Urol. 50: 969–79; discussion 980. PMID 16469429. doi:10.1016/j.eururo.2005.12.042.
- ↑ Imiak; et al. (1 Jan 1999). "TURP Syndrome".