Oculomotor nerve
| Oculomotor nerve | |
|---|---|
 Nerves of the orbit. Seen from above. | |
 Inferior view of the human brain, with the cranial nerves labelled. | |
| Details | |
| From | oculomotor nucleus, Edinger-Westphal nucleus |
| To | superior branch, inferior branch |
| Innervates | Superior rectus, Inferior rectus, Medial rectus, Inferior oblique, Levator palpebrae, sphincter pupillae (parasympathetics), ciliaris muscle (parasympathetics) |
| Identifiers | |
| Latin | nervus oculomotorius |
| MeSH | A08.800.800.120.600 |
| TA | A14.2.01.007 |
| FMA | 50864 |
| Cranial nerves |
|---|
|
The oculomotor nerve is the third cranial nerve. It enters the orbit via the superior orbital fissure and innervates muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the muscles that enable pupillary constriction and accommodation (ability to focus on near objects as in reading). The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement. [1]
Structure
The oculomotor nerve originates from the third nerve nucleus at the level of the superior colliculus in the midbrain. The third nerve nucleus is located ventral to the cerebral aqueduct, on the pre-aqueductal grey matter. The fibers from the two third nerve nuclei located laterally on either side of the cerebral aqueduct then pass through the red nucleus. From the red nucleus fibers then pass via the substantia nigra exiting through the interpeduncular fossa.
On emerging from the brainstem, the nerve is invested with a sheath of pia mater, and enclosed in a prolongation from the arachnoid. It passes between the superior cerebellar (below) and posterior cerebral arteries (above), and then pierces the dura mater anterior and lateral to the posterior clinoid process, passing between the free and attached borders of the tentorium cerebelli.
It traverses the cavernous sinus, above the other orbital nerves receiving in its course one or two filaments from the cavernous plexus of the sympathetic nervous system, and a communicating branch from the ophthalmic division of the trigeminal nerve. As the oculomotor nerve enters the orbit it divides into a superior and an inferior branch, which enter the orbit through the superior orbital fissure.[1]
Superior branch
The superior branch of the oculomotor nerve or the superior division, the smaller, passes medially over the optic nerve. It supplies the superior rectus and levator palpebrae superioris.
Inferior branch
The inferior branch of the oculomotor nerve or the inferior division, the larger, divides into three branches.
- One passes beneath the optic nerve to the medial rectus.
- Another, to the inferior rectus.
- The third and longest runs forward between the inferior recti and lateralis to the inferior oblique. From the last a short thick branch is given off to the lower part of the ciliary ganglion, and forms its short root.
All these branches enter the muscles on their ocular surfaces, with the exception of the nerve to the inferior oblique, which enters the muscle at its posterior border.
Nuclei
The oculomotor nerve (CN III) arises from the anterior aspect of mesencephalon (midbrain). There are two nuclei for the oculomotor nerve:
- The oculomotor nucleus originates at the level of the superior colliculus. The muscles it controls are the striated muscle in levator palpebrae superioris and all extraocular muscles except for the superior oblique muscle and the lateral rectus muscle.
- The Edinger-Westphal nucleus supplies parasympathetic fibers to the eye via the ciliary ganglion, and thus controls the sphincter pupillae muscle (affecting pupil constriction) and the ciliary muscle (affecting accommodation).
Sympathetic postganglionic fibres also join the nerve from the plexus on the internal carotid artery in the wall of the cavernous sinus and are distributed through the nerve, e.g., to the smooth muscle of superior tarsal (Mueller's) muscle.
Function
The oculomotor nerve include axons of type GSE, general somatic efferent, which innervate skeletal muscle of the levator palpebrae superioris, superior rectus, medial rectus, inferior rectus, and inferior oblique muscles.(innervates all the extrinsic muscles except superior oblique and lateral rectus.)
The nerve also includes axons of type GVE, general visceral efferent, which provide preganglionic parasympathetics to the ciliary ganglion. From the ciliary ganglion post ganglionic fibers pass through the short ciliary nerve to the constrictor pupillae of the iris and the cilliary muscles.
Clinical significance
Disease
Paralysis of the oculomotor nerve, i.e., oculomotor nerve palsy, can arise due to:
- direct trauma,
- demyelinating diseases (e.g., multiple sclerosis),
- increased intracranial pressure (leading to uncal herniation)
- due to a space-occupying lesion (e.g., brain cancer) or a
- spontaneous subarachnoid haemorrhage (e.g., berry aneurysm), and
- microvascular disease, e.g., diabetes.
In people with diabetes and older than 50 years of age, an oculomotor nerve palsy, in the classical sense, occurs with sparing (or preservation) of the pupillary reflex. This is thought to arise due the anatomical arrangement of the nerve fibers in the oculomotor nerve; fibers controlling the pupillary function are superficial and spared from ischemic injuries typical of diabetes. On the converse, an aneurysm which leads to compression of the oculomotor nerve affects the superficial fibers and manifests as a third nerve palsy with loss of the pupillary reflex (in fact, this third nerve finding is considered to represent an aneurysm—until proven otherwise—and should be investigated).[2]
Examination
Eye muscles
Cranial nerves III, IV, and VI are usually tested together as part of the cranial nerve examination. The examiner typically instructs the patient to hold his head still and follow only with the eyes a finger or penlight that circumscribes a large "H" in front of the patient. By observing the eye movement and eyelids, the examiner is able to obtain more information about the extraocular muscles, the levator palpebrae superioris muscle, and cranial nerves III, IV, and VI. Loss of function of any of the eye muscles results in ophthalmoparesis.
Since the oculomotor nerve controls most of the eye muscles, it may be easier to detect damage to it. Damage to this nerve, termed oculomotor nerve palsy is also known by the down 'n out symptoms, because of the position of the affected eye (lateral, downward deviation of gaze).
Pupillary reflex
The oculomotor nerve also controls the constriction of the pupils and thickening of the lens of the eye. This can be tested in two main ways. By moving a finger toward a person's face to induce accommodation, their pupils should constrict.
Shining a light into one eye should result in equal constriction of the other eye. The neurons in the optic nerve decussate in the optic chiasm with some crossing to the contralateral optic nerve tract. This is the basis of the "swinging-flashlight test".
Loss of accommodation and continued pupillary dilation can indicate the presence of a lesion on the oculumotor nerve.
Additional images
 Map of the oculomotor nerve.
Map of the oculomotor nerve. Median sagittal section of brain.
Median sagittal section of brain.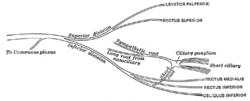 Plan of oculomotor nerve.
Plan of oculomotor nerve. Pathways in the Ciliary Ganglion.
Pathways in the Ciliary Ganglion.
See also
References
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
External links
| Wikimedia Commons has media related to Nervus oculomotorius. |
- MedEd at Loyola GrossAnatomy/h_n/cn/cn1/cn3.htm
- oph/183 at eMedicine - "Oculomotor nerve palsy"
- Oculomotor Nerve at the US National Library of Medicine Medical Subject Headings (MeSH)
- hier-479 at NeuroNames
- Animations of extraocular cranial nerve and muscle function and damage (University of Liverpool)
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (III)
- Notes on Oculomotor Nerve