Lymphotoxin alpha
Lymphotoxin-alpha (LT-α) or tumor necrosis factor-beta (TNF-β) is a protein that in humans is encoded by the LTA gene.[5][6] Belonging to the hematopoietic cell line, LT-α exhibits anti-proliferative activity and causes the cellular destruction of tumor cell lines.[5] As a cytotoxic protein, LT-α performs a variety of important roles in immune regulation depending on the form that it is secreted as. In other words, LT-α has both a membrane-bound and soluble form that perform distinct roles in immune regulation.[7]
LT-α has a significant impact on the maintenance of the immune system including the development of secondary lymphoid organs.[7][8] Absence of LT-α leads to the disruption of gastrointestinal development, prevents Peyer's patch development, and results in a disorganized spleen.[9]
As a signaling molecule, LT-α is involved in the regulation of cell survival, proliferation, differentiation, and apoptosis.[10] LT-α plays an important role in innate immune regulation and its presence has been shown to prevent tumor growth and destroy cancerous cell lines.[11] In contrast, unregulated expression of LT-α can result in a constantly active signaling pathway, thus leading to uncontrolled cellular growth and creation of tumors.[10] Hence depending on the context, LT-α may function to prevent growth of cancer cells or facilitate the development of tumors. Furthermore, LT-α effects depend on the type of organ it acts upon, type of cancer cells, cellular environment, gender, and time of effect during an immune response.[12][11]
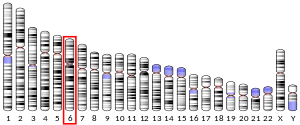
Gene
The human gene encoding for LT-α was cloned in 1985.[5][13] The gene of LT-α is located on chromosome 6 and is in close proximity of the gene encoding major histocompatibility complex.[14]
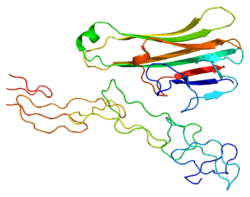
Structure
LT-α is translated as a 25 kDa glycosylated polypeptide with 171 amino acid residues.[6] Furthermore, human LT-α is 72% identical to mouse LT-α at the protein's primary sequence.[15]
LTα expression is highly inducible and when secreted, forms a soluble homotrimeric molecule. LT-α can also form heterotrimers with lymphotoxin-beta, which anchors lymphotoxin-alpha to the cell surface. The interaction between LT-α and LT-β results in the formation of a membrane bound complex (LT-α1-β2).[8]
Function
Lymphotoxin alpha, a member of the tumor necrosis factor family, is a cytokine produced by lymphocytes. LT-α1-β2 can interact with receptors such as LT-β receptors.[10] Absence of LT-β on cell surfaces will diminish the ability of LT-α to form LT-α1-β2, thus decreasing its effective ability as a cytokine.[7][8] LT-α mediates a large variety of inflammatory, immunostimulatory, and antiviral responses. LT-α is also involved in the formation of secondary lymphoid organs during development and plays a role in apoptosis.[16]
In LT-α knockout mice, Peyer's patches and lymph nodes will fail to develop, thus illustrating the cytokine's essential role in immunological development.[17]
As a cytotoxic protein, LT-α causes the destruction of cancerous cell lines, activates signaling pathways, and effectively kills transformed tumor cells.[7][10] However, mice with overexpression of LT-α or LT-β showed increased tumor growth and metastasis in several models of cancer. Interestingly, in other studies, mice with gene knockout of LT-α showed enhanced tumor growth, implicating possible protective role of LT-α in cancer. However, these studies utilized mice with complete LT-α deficiency that did not allow to distinguish effects of soluble versus membrane-associated LT.[18]
LT-α mediated signaling pathway
As a member of the TNF family, LT-α binds to various receptors and activates the NF-κB pathway, thus promoting immune regulation through the innate immune response.[10] In order for activation to occur, LT-α must form a complex with LT-β to form the LT-α1-β2 complex. Formation of LT-α1-β2 complex enables binding to LT-β receptors and subsequent activation of signaling pathways.[19] Activation of signaling pathways such as NF-κB ultimately leads to various cellular fates, including cell proliferation and cell death. After LT-β receptor activation, IKK-α, β, and γ are produced, which increases degradation of I-κB, an inhibitor or NF-kB, and produce NF-kB1 (p50) and ReIA (p60).[19] The production of NF-kB1 and ReIA increases rates of gene transcription of cytokines and inflammatory-inducing molecules.[19][20]
Anti-carcinogenic properties
Activation of LT-β receptors is capable of inducing cell death of cancerous cells and suppressing tumor growth.[21][22] The process of cell death is mediated by the presence of IFN-γ and can involve apoptotic or necrotic pathways.[21] It is seen that LT-β receptors facilitate the upregulation of adhesion molecules and recruit lymphocytes to tumor cells to combat tumor growth.[5][10] In other words, LT-α interactions with LT-β receptors can increase anti-tumor effects through direct destruction of tumor cells.
Pro-carcinogenic properties
However, recent studies have shown the contribution of LT-α mediated signaling to the development of cancer.[7][10][11][12] As mentioned previously, LT-α signaling can promote inflammatory responses, but prolonged inflammation can cause serious cellular damage and increase the risk of certain diseases including cancer.[11] Thus, mutations in regulatory factors in LT-α signaling pathways can promote cell signaling disruptions and encourage the creation of cancerous cell lines. One of these mutations includes constant binding of LT-α1-β2 complex to LT-β receptors, which results in the constant activation of the NF-κB alternative pathway.[10][11] Presence of a constitutively active NF-κB pathway manifests in multiple myeloma and other cancer-related diseases.[10] Removal of LT-β receptors has shown to inhibit tumor growth and decrease angiogenesis.[11] Thus, lymphotoxin and its downstream signaling via the NF-κB pathway illustrate the cytokine's influence on tumor development and metastasis.
A fully humanized anti-LT-α antibody (Pateclizumab or MLTA3698A) has been shown to react with both LT-α and LT-β.[7] Clinical trials involving this antibody have yet to be employed, but the creation of this antibody offers alternative inhibitory methods for the NF-κB pathway.
Effects on gastrointestinal system
The gastrointestinal immune system contains up to 70-80% of the antibody producing cells of the body.[9] During embryonic development, LT-α signaling plays an active part in the formation of the gastrointestinal immune system.[9] In particular, LT-α mediated signaling is responsible for the development of intestinal lymphoid structures such as Peyer’s patches.[23][24] This intestinal lymphoid follicle plays an important role in the immune system of the digestive tract.
Peyer’s patches are highly specialized lymphoid nodules located in the intestine. They are surrounded by follicle-associated epithelium and are able to interact with other immune cells through the transcytosis of foreign antigens.[25] In addition to this function, Peyer’s patches facilitate the production Ig-A producing immunocytes, thus increasing the efficacy of the adaptive immune system.[26]
The development of Peyer’s patches requires the binding and activation of LT-β receptor with LT-α1-β2 complex. Experiments involving transgenic mice have shown that the absence of LT-α resulted in the lack of Peyer’s patches and other lymph nodes.[9] The lack of Peyer’s patches and other lymph nodes have also been shown to reduce levels of Ig-A.[9] Being the most produced immunoglobulin, Ig-A protects against mucosal pathogens by regulating bacterial growth and inhibiting antigen adhesion to the intestine under normal conditions.[27] Reduced levels of Ig-A greatly diminishes gut immune regulation and deregulate protection against microbes, thereby emphasizing the importance of LT-mediated response for the expression of Ig-A.
Nomenclature
Discovered by Granger and his research group in 1960, LT-alpha was known as lymphotoxin.[28] As years progressed, its name was changed to tumor necrosis factor-beta (TNF-β).[29] Later discovery of LT-β and LT-α1-β2 complex prompted the disposal of TNF-β and the subdivision of LT into two classes: LT-α and LT-β.[30][31]
Interactions
Lymphotoxin alpha has been shown to interact with LTB.[32][33][34]
See also
References
- 1 2 3 ENSG00000223919, ENSG00000173503, ENSG00000226275, ENSG00000230279, ENSG00000238130, ENSG00000226979 GRCh38: Ensembl release 89: ENSG00000231408, ENSG00000223919, ENSG00000173503, ENSG00000226275, ENSG00000230279, ENSG00000238130, ENSG00000226979 - Ensembl, May 2017
- 1 2 3 GRCm38: Ensembl release 89: ENSMUSG00000024402 - Ensembl, May 2017
- ↑ "Human PubMed Reference:".
- ↑ "Mouse PubMed Reference:".
- 1 2 3 4 Nedwin GE, Naylor SL, Sakaguchi AY, Smith D, Jarrett-Nedwin J, Pennica D, Goeddel DV, Gray PW (September 1985). "Human lymphotoxin and tumor necrosis factor genes: structure, homology and chromosomal localization". Nucleic Acids Research. 13 (17): 6361–73. PMC 321958
 . PMID 2995927. doi:10.1093/nar/13.17.6361.
. PMID 2995927. doi:10.1093/nar/13.17.6361. - 1 2 Aggarwal BB, Eessalu TE, Hass PE (February 1986). "Characterization of receptors for human tumour necrosis factor and their regulation by gamma-interferon". Nature. 318 (6047): 665–7. PMID 3001529. doi:10.1038/318665a0.
- 1 2 3 4 5 6 Ruddle NH (April 2014). "Lymphotoxin and TNF: how it all began-a tribute to the travelers". Cytokine & Growth Factor Reviews. 25 (2): 83–9. PMC 4027955
 . PMID 24636534. doi:10.1016/j.cytogfr.2014.02.001.
. PMID 24636534. doi:10.1016/j.cytogfr.2014.02.001. - 1 2 3 Ngo VN, Korner H, Gunn MD, Schmidt KN, Riminton DS, Cooper MD, Browning JL, Sedgwick JD, Cyster JG (January 1999). "Lymphotoxin alpha/beta and tumor necrosis factor are required for stromal cell expression of homing chemokines in B and T cell areas of the spleen". The Journal of Experimental Medicine. 189 (2): 403–12. PMC 2192983
 . PMID 9892622.
. PMID 9892622. - 1 2 3 4 5 Gubernatorova EO, Tumanov AV (November 2016). "Tumor Necrosis Factor and Lymphotoxin in Regulation of Intestinal Inflammation". Biochemistry. Biokhimiia. 81 (11): 1309–1325. PMID 27914457. doi:10.1134/S0006297916110092.
- 1 2 3 4 5 6 7 8 9 Bauer J, Namineni S, Reisinger F, Zöller J, Yuan D, Heikenwälder M (2012-01-01). "Lymphotoxin, NF-ĸB, and cancer: the dark side of cytokines". Digestive Diseases. 30 (5): 453–68. PMID 23108301. doi:10.1159/000341690.
- 1 2 3 4 5 6 Fernandes MT, Dejardin E, dos Santos NR (April 2016). "Context-dependent roles for lymphotoxin-β receptor signaling in cancer development". Biochimica et Biophysica Acta. 1865 (2): 204–19. PMID 26923876. doi:10.1016/j.bbcan.2016.02.005.
- 1 2 Wong GH, Kaspar RL, Zweiger G, Carlson C, Fong SE, Ehsani N, Vehar G (January 1996). "Strategies for manipulating apoptosis for cancer therapy with tumor necrosis factor and lymphotoxin". Journal of Cellular Biochemistry. 60 (1): 56–60. PMID 8825416. doi:10.1002/(SICI)1097-4644(19960101)60:1<56::AID-JCB9>3.0.CO;2-2.
- ↑ Pokholok DK, Maroulakou IG, Kuprash DV, Alimzhanov MB, Kozlov SV, Novobrantseva TI, Turetskaya RL, Green JE, Nedospasov SA (January 1995). "Cloning and expression analysis of the murine lymphotoxin beta gene". Proceedings of the National Academy of Sciences of the United States of America. 92 (3): 674–8. PMC 42682
 . PMID 7846035.
. PMID 7846035. - ↑ Nedospasov SA, Hirt B, Shakhov AN, Dobrynin VN, Kawashima E, Accolla RS, Jongeneel CV (October 1986). "The genes for tumor necrosis factor (TNF-alpha) and lymphotoxin (TNF-beta) are tandemly arranged on chromosome 17 of the mouse". Nucleic Acids Research. 14 (19): 7713–25. PMID 3490653.
- ↑ Pennica D, Nedwin GE, Hayflick JS, Seeburg PH, Derynck R, Palladino MA, Kohr WJ, Aggarwal BB, Goeddel DV (1984). "Human tumour necrosis factor: precursor structure, expression and homology to lymphotoxin". Nature. 312 (5996): 724–9. PMID 6392892. doi:10.1038/312724a0.
- ↑ "Entrez Gene: LTA lymphotoxin alpha (TNF superfamily, member 1)".
- ↑ Akirav E, Liao S, Ruddle N (2008). "Chapter 2: Lymphoid Tissues and Organs". In Paul W. Fundamental Immunology (6th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 27–55. ISBN 0-7817-6519-6.
- ↑ Korneev KV, Atretkhany KN, Drutskaya MS, Grivennikov SI, Kuprash DV, Nedospasov SA (January 2017). "TLR-signaling and proinflammatory cytokines as drivers of tumorigenesis". Cytokine. 89: 127–135. PMID 26854213. doi:10.1016/j.cyto.2016.01.021.
- 1 2 3 Müller JR, Siebenlist U (April 2003). "Lymphotoxin beta receptor induces sequential activation of distinct NF-kappa B factors via separate signaling pathways". The Journal of Biological Chemistry. 278 (14): 12006–12. PMID 12556537. doi:10.1074/jbc.M210768200.
- ↑ Yilmaz ZB, Weih DS, Sivakumar V, Weih F (January 2003). "RelB is required for Peyer's patch development: differential regulation of p52-RelB by lymphotoxin and TNF". The EMBO Journal. 22 (1): 121–30. PMID 12505990. doi:10.1093/emboj/cdg004.
- 1 2 Browning JL, Miatkowski K, Sizing I, Griffiths D, Zafari M, Benjamin CD, Meier W, Mackay F (March 1996). "Signaling through the lymphotoxin beta receptor induces the death of some adenocarcinoma tumor lines". The Journal of Experimental Medicine. 183 (3): 867–78. PMID 8642291.
- ↑ Lukashev M, LePage D, Wilson C, Bailly V, Garber E, Lukashin A, et al. (October 2006). "Targeting the lymphotoxin-beta receptor with agonist antibodies as a potential cancer therapy". Cancer Research. 66 (19): 9617–24. PMID 17018619. doi:10.1158/0008-5472.CAN-06-0217.
- ↑ Fu YX, Chaplin DD (1999-01-01). "Development and maturation of secondary lymphoid tissues". Annual Review of Immunology. 17: 399–433. PMID 10358764. doi:10.1146/annurev.immunol.17.1.399.
- ↑ Randall TD, Carragher DM, Rangel-Moreno J (2008-01-01). "Development of secondary lymphoid organs". Annual Review of Immunology. 26: 627–50. PMID 18370924. doi:10.1146/annurev.immunol.26.021607.090257.
- ↑ Cornes JS (June 1965). "Number, size, and distribution of Peyer's patches in the human small intestine: Part I The development of Peyer's patches". Gut. 6 (3): 225–9. PMID 18668776.
- ↑ Craig SW, Cebra JJ (July 1971). "Peyer's patches: an enriched source of precursors for IgA-producing immunocytes in the rabbit". The Journal of Experimental Medicine. 134 (1): 188–200. PMID 4934147.
- ↑ Fagarasan S, Honjo T (January 2003). "Intestinal IgA synthesis: regulation of front-line body defences". Nature Reviews. Immunology. 3 (1): 63–72. PMID 12511876. doi:10.1038/nri982.
- ↑ Williams TW, Granger GA (September 1968). "Lymphocyte in vitro cytotoxicity: lymphotoxins of several mammalian species". Nature. 219 (5158): 1076–7. PMID 5673378.
- ↑ Shalaby MR, Aggarwal BB, Rinderknecht E, Svedersky LP, Finkle BS, Palladino MA (September 1985). "Activation of human polymorphonuclear neutrophil functions by interferon-gamma and tumor necrosis factors". Journal of Immunology. 135 (3): 2069–73. PMID 3926894.
- ↑ Browning JL, Ngam-ek A, Lawton P, DeMarinis J, Tizard R, Chow EP, Hession C, O'Brine-Greco B, Foley SF, Ware CF (March 1993). "Lymphotoxin beta, a novel member of the TNF family that forms a heteromeric complex with lymphotoxin on the cell surface". Cell. 72 (6): 847–56. PMID 7916655.
- ↑ Koni PA, Sacca R, Lawton P, Browning JL, Ruddle NH, Flavell RA (April 1997). "Distinct roles in lymphoid organogenesis for lymphotoxins alpha and beta revealed in lymphotoxin beta-deficient mice". Immunity. 6 (4): 491–500. PMID 9133428.
- ↑ Williams-Abbott L, Walter BN, Cheung TC, Goh CR, Porter AG, Ware CF (August 1997). "The lymphotoxin-alpha (LTalpha) subunit is essential for the assembly, but not for the receptor specificity, of the membrane-anchored LTalpha1beta2 heterotrimeric ligand". The Journal of Biological Chemistry. 272 (31): 19451–6. PMID 9235946. doi:10.1074/jbc.272.31.19451.
- ↑ Browning JL, Sizing ID, Lawton P, Bourdon PR, Rennert PD, Majeau GR, Ambrose CM, Hession C, Miatkowski K, Griffiths DA, Ngam-ek A, Meier W, Benjamin CD, Hochman PS (October 1997). "Characterization of lymphotoxin-alpha beta complexes on the surface of mouse lymphocytes". Journal of Immunology. 159 (7): 3288–98. PMID 9317127.
- ↑ Browning JL, Dougas I, Ngam-ek A, Bourdon PR, Ehrenfels BN, Miatkowski K, Zafari M, Yampaglia AM, Lawton P, Meier W (January 1995). "Characterization of surface lymphotoxin forms. Use of specific monoclonal antibodies and soluble receptors". Journal of Immunology. 154 (1): 33–46. PMID 7995952.
Further reading
- Körner H, Sedgwick JD (October 1996). "Tumour necrosis factor and lymphotoxin: molecular aspects and role in tissue-specific autoimmunity". Immunology and Cell Biology. 74 (5): 465–72. PMID 8912010. doi:10.1038/icb.1996.77.
- Wang Q (May 2005). "Molecular genetics of coronary artery disease". Current Opinion in Cardiology. 20 (3): 182–8. PMC 1579824
 . PMID 15861005. doi:10.1097/01.hco.0000160373.77190.f1.
. PMID 15861005. doi:10.1097/01.hco.0000160373.77190.f1. - Copeland KF (December 2005). "Modulation of HIV-1 transcription by cytokines and chemokines". Mini Reviews in Medicinal Chemistry. 5 (12): 1093–101. PMID 16375755. doi:10.2174/138955705774933383.
- Elewaut D, Ware CF (April 2007). "The unconventional role of LT alpha beta in T cell differentiation". Trends in Immunology. 28 (4): 169–75. PMID 17336158. doi:10.1016/j.it.2007.02.005.