Sacroiliac joint dysfunction
Sacroiliac joint dysfunction, also called sacroiliac joint disorder, sacroiliac joint disease, sacroiliac joint syndrome or sacroiliac syndrome, or "sacroilliac dysfunction and instability", generally refers to pain in the sacroiliac joint region that is caused by abnormal motion in the sacroiliac joint, either too much motion or too little motion. It typically results in inflammation of the sacroiliac joint, and can be debilitating.
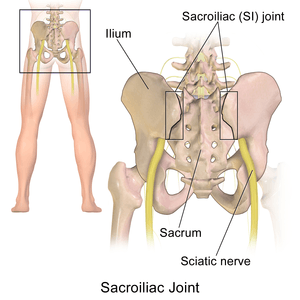
Anatomy and physiology of the sacroiliac joints
The sacroiliac joint is a true diarthrodial joint that joins the sacrum to the pelvis.[1][2][3][4] The sacrum connects on the right and left sides to the ilia (pelvic bones) to form the sacroiliac joints. The pelvic girdle is made up of two innominate bones (the iliac bones) and the sacrum. The innominate bones join in the front of the pelvis to form the pubic symphysis, and at back of the sacrum to form the sacroiliac (SI) joints. Each innominate bone (ilium) joins the femur (thigh bone) to form the hip joint; thus the sacroiliac joint moves with walking and movement of the torso.[5]
In this joint, hyaline cartilage on the sacral side moves against fibrocartilage on the iliac side. The sacroiliac joint contains numerous ridges and depressions that function in stability. Studies have documented that motion does occur at the joint; therefore, slightly subluxed and even locked positions can occur.[2][3][6][7][8][9][10]
Muscles and ligaments surround and attach to the SI joint in the front and back, primarily on the ilial or sacral surfaces. These can all be a source of pain and inflammation if the SI joint is dysfunctional.[5][6] The sacroiliac joint is highly dependent on its strong ligamentous structure for support and stability.[5] The most commonly disrupted and/or torn ligaments are the iliolumbar ligament and the posterior sacroiliac ligament.[5] The ligamentous structures offer resistance to shear and loading. The deep anterior, posterior, and interosseous ligaments resist the load of the sacrum relative to the ilium.[1] More superficial ligaments (e.g., the sacrotuberous ligament) react to dynamic motions (such as straight-leg raising during physical motion).[1] The long dorsal sacroiliac ligament can become stretched in periods of reduced lumbar lordosis (e.g., during pregnancy).[1]
Common symptoms
Common symptoms include lower back pain, buttocks pain, sciatic leg pain, groin pain, hip pain (for explanation of leg, groin, and hip pain, see referred pain), urinary frequency, and "transient numbness, prickling, or tingling."[1][6][8][11][12][13][14] Pain can range from dull aching to sharp and stabbing and increases with physical activity.[1][2][6] Symptoms also worsen with prolonged or sustained positions (i.e., sitting, standing, lying).[2][5][6] Bending forward, stair climbing, hill climbing, and rising from a seated position can also provoke pain. Pain is reported to increase during menstruation in women.[2][5][6] Patients with severe and disabling sacroiliac joint dysfunction can suffer from insomnia and depression.[15]
Affected muscle groups
Many large and small muscles have relationships with the ligaments of the sacroiliac joint including the piriformis (see “piriformis syndrome”, a condition often related with sacroiliac joint dysfunction), rectus femoris, gluteus maximus and minimus, erector spinae, latissimus dorsi, thoracolumbar fascia, and iliacus.[1] Any of these muscles can be involved or spasm with a painful and dysfunctional sacroiliac joint.[1][2][6][8][9][10] The SI joint is a pain-sensitive structure richly innervated by a combination of unmyelinated free nerve endings and the posterior primary rami of spinal segments L2-S3. The wide possibility of innervation may explain why pain originating from the joint can manifest in so many various ways, with different and unique referral patterns (see “referred pain”) for individual patients.[1][7] Patients with sacroiliac joint dysfunction can also develop tightness and dysfunction in the hamstring, quadriceps, iliotibial tract (see “iliotibial band syndrome”) and hip flexors, including the psoas muscle. Individuals with severe and long-standing sacroiliac joint dysfunction can develop muscle deconditioning and atrophy throughout the body due to limitation of activities and exercise that bring about pain in the low back.[1]
Causes of hypermobility and hypomobility
Hypermobility
SI joint dysfunction is sometimes referred to as "sacroiliac joint instability" or "sacroiliac joint insufficiency" due to the lack of support the once strong and taut ligaments can no longer sustain.[2][5][6][10] When the joint is hypermobile or loose, it is classified as an extra-articular dysfunction because abnormal joint movement and alignment is a consequence of weakened, injured, or sprained ligaments, while the joint itself is structurally normal and healthy. The sacroiliac joint itself often will not show degenerative changes, such as arthritis, until many years of the dysfunction being allowed to continue.[2] Injury to the ligaments that hold the sacroiliac joints in proper support is thought to be caused by a torsion or high impact injury (such as an automobile accident) or a hard fall, resulting in the hypermobility.[2] As many as 58% of patients diagnosed with sacroiliac joint pain had some inciting traumatic injury based on clinical examination findings.[14] The joint that was once stabilized by strong ligaments, now overly stretched, sprained, or torn, will move beyond its normal range. This is thought to result in the ilium and sacral surfaces "locking" in an incongruent or asymmetrical fashion (one innominate bone is tilted anteriorly; the other innominate bone is tilted posteriorly) causing pain that can be debilitating.[2]
Hormone imbalances, particularly those associated with pregnancy and the hormone relaxin, can also cause a ligamentous laxity resulting in the weakening of the sacroiliac structure. [16] During pregnancy, relaxin serves as nature's way of allowing the female pelvis to achieve distention of the birthing canal.[16] Pelvic joint pain in post pregnancy women is thought to be derived from the inability of the stretched out ligaments to return to normal tautness.[16] Women who have delivered large babies or who have had extended labors also are prone to developing chronic sacroiliac joint pain and instability. Concern has been expressed that specific testing is necessary to determine if peri-partum or post-partum hypermobility is present because there is a case in which the patient had all classical signs and symptoms of instability, yet micromotion testing revealed the joint to be stuck, and mobilization was effective in one visit.[17] Pain, including a long history of interstitial cystitis, and peri-partum urinary frequency were much improved and she had a very easy delivery. It is suggested that the stretch receptors of the bladder and uterus provoked the symptoms which were interpreted as "instability."
In some people, the sacroiliac joints reverse the normal concave-convex 'locking' relationship, which can lead to rotational misalignment.[2][5][6] The variation in joint configuration results in some sacroiliac joints being inherently weaker or more prone to misalignment.[5] Certain biomechanical or muscle length imbalances may ultimately predispose a person to sacroiliac dysfunction and pain. Likely, this is a result of altered gait patterns and repetitive stress to the SI joint and related structures.[1] These conditions exist in persons with leg-length inequality, scoliosis, a history of polio, poor-quality footwear, and hip osteoarthritis.[1] There is also a notable incidence of lumbar spinal fusion patients that present with sacroiliac pain and hypermobility, potentially due to the adjacent lumbar joints being fixed and unable to move. Clinical studies have found up to 75% of post-lumbar fusion patients develop SI joint degeneration within five years of surgery.[18]
Hypomobility
A model of hypomobility has been developed (Hesch, 2015) and makes the distinction between treatable and non-treatable hypomobility. Hypomobility is directly related to hypermobility when both conditions interact. As an example, a sacroiliac joint can be hypermobile in one direction, yet hypomobile in the opposite direction, for a variety of reasons. By gaining motion in the direction that was hypomobile, the mobility of the opposite hypermobile direction is reduced, improving stability to the joint. This a foundational principle to the Hesch Method of treating sacroiliac joint dysfunction. This scale applies to both typical movements such as flexion/extension, rotation, etc. It also applies to passive accessory motions such as superior, inferior, medial and lateral glide, etc. It is relevant to realize that one cannot always know at the initial examination whether a specific classification such as treatable/non-treatable hypomobility can be assigned. At times the appropriate grading is known only after attempt at intervention is made.
1. Hypomobile: non-treatable joint (ankylosed)
Considerable limitation which is non-mutable per appropriate attempts to gain motion. Etiology can be from ageing, disease, old trauma with intra-articular bleed with unyielding scar tissue, etc.
2. Hypomobile: treatable
Significantly rigid, AKA Rigid hypomobility. These typically respond to brief intervention and may reflect both a positional and a reflex muscular interaction. Perhaps these are underappreciated in the clinical realm.
Moderate limit
Slight limit
3. Normal
Pathological Hypomobility (too little movement) of the sacroiliac joint is an intra-articular disorder in which the joint locks due to wearing down with age or degenerative joint disease. Hypomobility of this kind can also occur with an inflammatory disease such as ankylosing spondylitis,[20] rheumatoid arthritis, or an infection.
Diagnosis and testing
Perhaps the biggest reason for misdiagnosis or lack of diagnosis of sacroiliac joint dysfunction is based on the inability of common radiological imaging to discern the disorder. Diagnostic testing, such as X-ray, CT scan, or MRI, do not usually reveal abnormalities; therefore, they cannot reliably be used for diagnosis of sacroiliac joint dysfunction.[5][6] There is a new definitive imaging test SPECT/CT which can sometimes detect sacroiliac joint dysfunction. There is also a lack of evidence that sacroiliac joint mobility maneuvers (Gillet, Standing flexion test, and Seated Flexion test) detect motion abnormalities.[21][22] Given the inherent technical limitations of the visible and palpable signs from these sacroiliac joint mobility maneuvers another broad category of clinical signs have been described called provocative maneuvers. These maneuvers are designed to reproduce or increase pain emanating within the sacroiliac joint.
A clinician (i.e., a spine surgeon, orthopedic surgeon, sports medicine doctor, medical massage therapist, physical therapist, physiatrist, osteopath or chiropractor) can develop a probable diagnosis of sacroiliac joint dysfunction by using a hands on approach through palpating the painful areas and performing the following provocative maneuvers below:
- Gaenslen test - This pain provocation test applies torsion to the joint. With one hip flexed onto the abdomen, the other leg is allowed to dangle off the edge of the table. Pressure should then be directed downward on the leg in order to achieve hip extension and stress the sacroiliac joint.[1][6]
- Iliac Gapping Test - Distraction can be performed to the anterior sacroiliac ligaments by applying pressure to the anterior superior iliac spine.[1]
- Iliac Compression Test - Apply compression to the joint with the patient lying on his or her side. Pressure is applied downward to the uppermost iliac crest.[1]
- FABER or Patrick test - To identify if pain may come from the sacroiliac joint during flexion, abduction, and external rotation, the clinician externally rotates the hip while the patient lies supine. Then, downward pressure is applied to the medial knee stressing both the hip and sacroiliac joint.[1][6][11]
- Thigh Thrust - This test applies anteroposterior shear stress on the SI joint. The patient lies supine with one hip flexed to 90 degrees. The examiner stands on the same side as the flexed leg. The examiner provides either a quick thrust or steadily increasing pressure through the line of the femur. The pelvis is stabilized at the sacrum or at the opposite ASIS with the hand of the examiner
Cautious interpretation is warranted because there are no biomechanical studies showing that the Thigh Thrust test isolates forces in the SIJ when performed at 90 degrees and due to intra-individual variation in body type, hip flexibility, general flexibility of the trunk and pelvis.[23] In all the tests, pain along the typical area raises suspicion for sacroiliac joint dysfunction. However no single test is very reliable in the diagnosis of sacroiliac joint dysfunction. It is important to remember true neurogenic weakness, numbness, or loss of reflex should alert the clinician to consider nerve root pathology.[24]
The current "gold standard" for diagnosis of sacroiliac joint dysfunction emanating within the joint is sacroiliac joint injection confirmed under fluoroscopy or CT-guidance using a local anesthetic solution. The diagnosis is confirmed when the patient reports a significant change in relief from pain and the diagnostic injection is performed on 2 separate visits. Published studies have used at least a 75 percent change in relief of pain before a response is considered positive and the sacroiliac joint deemed the source of pain.[25][26][27] However, several other injection studies have compared intra-articular with extra-articular injection, and indicate that the ligament injection behind the joint is oftentimes superior to injection in the joint and seems to be a very underutilized diagnostic tool.[24][28]
Misdiagnosis and controversy
In the early 1900s, dysfunction of the sacroiliac joint was a common diagnosis associated with low back and sciatic nerve pain.[7] However, research by Danforth and Wilson in 1925 concluded that the sacroiliac joint could not cause sciatic nerve pain because the joint does not have a canal in which the nerves can be entrapped against the joint.[29] The biomechanical relationship between the sacroiliac joint, the piriformis muscle (see “piriformis syndrome”), and the sciatic nerve had not yet been discovered.[7]
In 1934, the work of Mixter and Barr shifted all emphasis in research and treatment from the sacroiliac to the herniated intervertebral disc, namely lumbar discs.[30] Medical focus on herniated discs was further forwarded by the invention of the MRI in 1977.[31] Recent medical research has revealed that patients with degenerating or herniated discs shown on MRI can frequently complain of little to no pain symptoms, while patients with an unremarkable MRI and no disc pathology can have severe back or sciatic pain.[32] Over-diagnosis and attention on herniated discs has led to the SI joint becoming an underappreciated pain generator in an estimated 15% to 25% of patients with axial low back pain.[1][2][8][12][13][14]
The ligaments in the sacroiliac are among the strongest in the body[32] and are not suspected by many clinicians to ever be susceptible to spraining or tearing. Skepticism of the existence of sacroiliac joint dysfunction within the medical community is furthered by the debate on how little or much the sacroiliac joint moves. A discrepancy as large as 2-17 degrees has been reported in clinical findings.[33][34][35]
The sacroiliac joint has been found to be the primary nociceptive structure in up to 30% of patients with chronic lower back pain.
Treatment
Treatment is often dependent on the duration and severity of the pain and dysfunction. In the acute phase (first 1–2 weeks) for a mild sprain of the sacroiliac, it is typical for the patient to be prescribed rest, ice/heat, and physical therapy; anti-inflammatory medicine can also be helpful.[1][11] Pelvic clock exercise, as described in Moshe Feldenkrais’s Awareness Through Movement, is one of the most effective components of physical therapy treatment.[36] It activates and strengthens muscles of pelvic cavity, helps reducing unnecessary tension in muscles involved in a lower back spasms. It plays an important role in the rehabilitation and neuromuscular education of the lower body, and is deeply rooted in the movement therapy known as somatics, which is used in the mobilization and alignment of lumbar, pelvic and hip joints, as well as relaxation, activation, and strengthening of deep core muscles.
If the pain does not resolve in the first 1–2 weeks, then the patient may benefit from a steroid and anesthetic mixture fluoroscopically injected into the joint (this also serves in confirming diagnosis), as well as manipulative or manual therapy.[1][2][5][6][8][10] For the most severe and chronic forms of sacroiliac dysfunction, treatment should proceed with the support of a sacroiliac belt, injection therapy, and finally, surgery.[1][2][5][6][7] The anti-inflammatory effect of injection therapy is not permanent, and the injections do not offer an opportunity to stabilize an incompetent joint.[37] Surgery is often considered a last resort, but for some patients, it is the only method of effectively stabilizing the loose joint. A fixation of the joint (screws or similar hardware only, without the use of bone grafting) is more common than a spinal fusion, as it is much less invasive, surgically straightforward, and results in a quicker recovery time for the patient.[2][5][7][38] Some experts in the field believe that it is important to make sure the sacroiliac joint is in an anatomically correct position prior to fixation or fusion, but published research contradicts this belief.[2][5][6][7][39][40] The problem of alignment of the pelvis is that this does not accurately indicate the true status of the inside articular structure, the SIJ. After over 2 decades of pre-fusion pelvic alignment, there is no objective measure to indicate the utility. Part of the difficulty lies in the fact that well intentioned clinicians blame the SIJ as causative for the patient's pelvic misalignment. Aligning the pelvis provides temporary relief or relief of pain may occur because multiple structures respond to malalignment such as the hip and lumbar spine; provoking a self-fulfilling prophecy of so-called "SIJ instability." Numerous studies have indicated poor to fair intertester reliability with pelvic palpation and the dubious nature of palpation and traditional gross motion testing was brought into question.[41][42][43]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Sherman, Andrew; Gotlin, Robert; et al. "Sacroiliac Joint Injury". Retrieved 18 January 2011.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Lippitt, AB (1995). "Percutaneous Fixation of the Sacroiliac Joint". In Vleeming, A. The integrated function of the lumbar spine and sacroiliac joint. et al. Rotterdam: European Conference Organizers. pp. 369–390.
- 1 2 Foley, BS; Buschbacher, RM (2006). "Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment". Am J Phys Med Rehabil. 85 (12): 997–1006. doi:10.1097/01.phm.0000247633.68694.c1.
- ↑ Frieberg, AH; Vinke, TH. "Sciatica and the sacroiliac joint". Clin Orthop Relat Res. 1974 (16): 126–34.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Sacroiliac Dysfunction: General Information, Anatomy, and Treatment". Retrieved January 18, 2011.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Sims, Vicki, PT (2004). The Secret Cause of Low Back Pain: How to End Your Suffering. Georgia: sipress. pp. 11–12. ISBN 978-0-9760347-0-4.
- 1 2 3 4 5 6 7 Richard Don Tigney. "The Sacroiliac Joint". Retrieved January 18, 2011.
- 1 2 3 4 5 Schwarzer, AC; et al. (Jan 1995). "The sacroiliac joint in chronic low back pain". Spine. 20 (1): 31–37. PMID 7709277. doi:10.1097/00007632-199501000-00007.
- 1 2 Hungerford, B; et al. Spine. 28 (14): 1593–1600. doi:10.1097/00007632-200307150-00022. Missing or empty
|title=(help) - 1 2 3 4 Heller, M (2006). "Sacroliliac Instability: An Overview". Dynamic Chiropractic. 24 (21).
- 1 2 3 Gentile, Julie (21 September 2010). "What is Sacroiliac Joint Dysfunction". Retrieved 18 January 2011.
- 1 2 Kirkaldy-Willis, WH; Bernard, TN Jr (1999). "Making a specific diagnosis". Managing Low Back Pain (4th ed.). Philadelphia: Churchill Livingstone. pp. 206–26.
- 1 2 Sembrano, Jonathan N.; et al. (2009). "How Often Is Low Back Pain Not Coming From the Back?". Spine 2009. 34 (1): E27–E32. doi:10.1097/BRS.0b013e31818b8882.
- 1 2 3 Bernard, TN Jr; Kirkaldy-Willis, WH (1987). "Recognizing specific characteristics of nonspecific low back pain". Clin Orthop Relat Res (217): 266–280. doi:10.1097/00003086-198704000-00029.
- ↑ Isaac, Zacharia; Devine, Jennifer. "Sacroiliac Joint Dysfunction". In Frontera, WR. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain and Rehabilitation. Saunders/Elsevier. ISBN 978-1-4160-4007-1.
- 1 2 3 MacLennan, AH; MacLenna, SC (1997). "Symptom-giving Pelvic Girdle Relaxation of Pregnancy, Postnatal Pelvic Joint Syndrome and Developmental Dysplasia of Hip". Acta Obstet Gynecol Scand. 76 (8): 760–764. doi:10.3109/00016349709024343.
- ↑ Hesch, J. CASE STUDY: False Positive Pelvic Instability in Pregnancy. Fall 2010 Newsletter International Organization of Physical Therapists in Women’s Health.
- ↑ Ha; et al. "Degeneration of Sacroiliac Joint After Instrumented Lumbar or Lumbosacral Fusion: A Prospective Cohort Study Over Five-Years Follow-Up". Spine. 33 (11): 1192–1198. doi:10.1097/brs.0b013e318170fd35.
- ↑ http://www.HeschInstitute.com
- ↑ Jee, WH; et al. (2004). "Sacroiliitis in patients with ankylosing spondylitis: association of MR findings with disease activity". Magn Reson Imaging: 245–250.
- ↑ Sturesson B. Selvik G, Uden A. Movements of the sacroiliac joints: aa roentgen stereophotogrammetric analysis" Spine 1989;14:162-165
- ↑ Sturesson B, Uden A, Vleeming A. A radiosteroemetric analysis of movements of the sacroiliac joint during the standing hip flexion test" Spine 2000; 25:364-368
- ↑ Hesch, Jerry (2011). Sacral Torsion in Dalton E. Dynamic Body. Oklahoma City, OK: Freedom From Pain. pp. 206–7. ISBN 978-0-615-27939-8.
- 1 2 Borowsky CD, Fagen G (2008). "Sources of sacroiliac region pain: insights gained from a study comparing standard intra-articular injection with a technique combining intra- and peri-articular injection". Arch Phys Med Rehabil. 89 (11): 2048–56. doi:10.1016/j.apmr.2008.06.006.
- ↑ Schwarzer AC, April CN, Bogduk N (1995). "The sacroiliac joint in chronic low back pain". Spine. 20: 31–37. PMID 7709277. doi:10.1097/00007632-199501000-00007.
- ↑ Maigne JY, Boulahdour H, Chatellier G (1998). "Value of quantitative radionucleotide bone scanning in the diagnosis of sacroiliac joint syndrome in 32 patients with low back pain". Eur Spine J. 7: 328–331. PMC 3611275
 . PMID 9765042. doi:10.1007/s005860050083.
. PMID 9765042. doi:10.1007/s005860050083. - ↑ Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain" Spine 1996;21:1889-1892
- ↑ MurakamiE Tanaka Y, Aizwa T, et al. (2007). "Effect of peri-articular and intra-articular lidocaine injections for sacroiliac joint pain: prospective comparative study". J Ortoped Science. 12: 274–280.
- ↑ Danforth, M; Wilson, P (1925). J Bone Joint Surg Am (7): 109. Missing or empty
|title=(help) - ↑ Mixter, WJ; Barr, JS (1934). "Rupture of the Intervertebral Disc with Involvement of the Spinal Canal". N Engl J Med. 211: 210–5. doi:10.1056/nejm193408022110506.
- ↑ "MRI's inside story". Economist. 4 December 2003. Retrieved May 23, 2011.
- 1 2 "Birth of the Disc Herniation". Chriogeek.com. Retrieved January 18, 2011.
- ↑ Smidt, GL; et al. (1995). "Sacroiliac kinematics for reciprocal straddle positions". Spine. 20 (9): 1047–1054. PMID 7631234. doi:10.1097/00007632-199505000-00011.
- ↑ Smidt, GL; et al. (1997). "Sacroiliac motion for extreme hip positions: A fresh cadaver study". Spine. 22 (18): 2073–2082. PMID 9322317. doi:10.1097/00007632-199709150-00003.
- ↑ Sturesson; et al. (2000). "A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test". Spine. 25 (3): 364–368. PMID 10703111. doi:10.1097/00007632-200002010-00018.
- ↑ Feldenkrais, Moshe (1972). Awareness Through Movement. HarperCollins. p. 115. ISBN 9780062503220.
- ↑ Zelle Boris A; et al. (2005). "Sacroiliac joint dysfunction: evaluation and management". The Clinical Journal of Pain. 21 (5): 446–455. doi:10.1097/01.ajp.0000131413.07468.8e.
- ↑ http://www.isass.org/video/sas11_videos/thursday/sas11_thur_29_315.html
- ↑ Tullberg T; et al. (1998). "Manipulation does not alter the position of the sacroiliac joint. A roentgen stereophotogrammetric analysis". Spine. 23 (10): 1124–1128. PMID 9615363. doi:10.1097/00007632-199805150-00010.
- ↑ Walker J M (1992). "The sacroiliac joint: a critical review". Physical Therapy. 72 (12): 903–916.
- ↑ Hujbregts PA. (2008) Evidence-base diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 16(3): 153–154.
- ↑ Hesch J. Manual Therapy Evaluation of the Pelvic Joints using Palpatory and Articular Spring Tests. Presented at the First Interdisciplinary World Congress on Low Back Pain and Its Relation to the Sacroiliac Joint; November 6, 1992; San Diego, CA.
- ↑ Hesch J, Aisenbrey J, Guarino J. The Pitfalls Associated With Traditional Evaluation of Sacroiliac Dysfunction and Their Proposed Solution. Presented at Annual Conference of the American Physical Therapy Association, Anaheim, CA June 25, 1990.
External links
- Michael R. Moore, M.D. discusses misdiagnosis
- Overview by Vladimir Djuric, M.D.
- Video summary of SI Joint Dysfunction