Health effects of sunlight exposure

The ultraviolet radiation in sunlight has both positive and negative health effects, as it is both a principal source of vitamin D3 and a mutagen.[1] A dietary supplement can supply vitamin D without this mutagenic effect.[2] Vitamin D has a wide range of positive health effects, which include strengthening bones[3] and possibly inhibiting the growth of some cancers.[4][5] UV exposure also has positive effects for endorphin levels, and possibly for protection against multiple sclerosis. Visible sunlight to the eyes gives health benefits through its association with the timing of melatonin synthesis, maintenance of normal and robust circadian rhythms, and reduced risk of seasonal affective disorder.[6]
Long-term sunlight exposure is known to be associated with the development of skin cancer, skin aging, immune suppression, and eye diseases such as cataracts and macular degeneration.[7] Short-term over-exposure is the cause of sunburn, snow blindness, and solar retinopathy.
UV rays, and therefore sunlight and sunlamps, are the only listed carcinogens that are known to have health benefits,[8] and a number of public health organizations state that there needs to be a balance between the risks of having too much sunlight or too little.[9] There is a general consensus that sunburn should always be avoided.
Synthesis of vitamin D3

UVB radiation with a wavelength of 290–315 nanometers penetrates uncovered skin and converts cutaneous 7-dehydrocholesterol to previtamin D3, which in turn becomes vitamin D3.[10][11][12] UVB radiation does not penetrate glass, so exposure to sunshine indoors through a window does not produce vitamin D.[13] Time of day, time of year, geographic latitude, ground altitude, cloud cover, smog, skin melanin content, and sunscreen are among the factors that greatly affect UV intensity and vitamin D synthesis,[12] making it difficult to provide general guidelines. It has been suggested by some researchers, for example, that adequate amounts of vitamin D can be produced with moderate sun exposure to the face, arms and legs, averaging 5–30 minutes twice per week without sunscreen. (The darker the complexion, or the weaker the sunlight, the more minutes of exposure are needed, approximating 25% of the time for minimal sunburn. Vitamin D overdose is impossible from UV exposure; the skin reaches an equilibrium where the vitamin degrades as fast as it is created.)[12][14][15] Individuals with limited sun exposure need to include good sources of vitamin D in their diet or take a supplement.
The only way to quantify adequate levels of vitamin D is with a serum 25(OH)D3 (calcifediol) test.[16] In the United States, serum 25(OH)D3 was below the recommended level for more than a third of white men in a 2005 study, with serum levels even lower in women and in most minorities. This indicates that vitamin D deficiency may be a common problem in the US.[17] Australia and New Zealand have had similar findings, which indicate insufficient protection against rickets for children and osteoporosis for adults.[18]
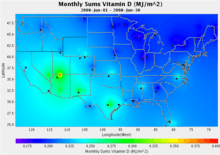
Over the past several years, levels of ultraviolet radiation have been tracked at over 30 sites across North America as part of the United States Department of Agriculture's UVB Monitoring and Research Program at Colorado State University. The first map at right shows levels of UVB radiation in June 2008, expressed in Vitamin D Equivalents.[19]
Using satellite data, measurements from the European Space Agency produce similar maps expressed in units of the widely followed UV Index, for locations around the world:[20]

Lower prevalence of multiple sclerosis
Multiple sclerosis (MS) is least prevalent in the sunniest regions.[21][22][23] Exposure to the ultraviolet-B radiation of sunlight appears to be most important and this may operate via vitamin D synthesis.[24]
Risks to skin

Ultraviolet (UV) irradiation present in sunlight is an environmental human carcinogen. The toxic effects of UV from natural sunlight and therapeutic artificial lamps are a major concern for human health. The major acute effects of UV irradiation on normal human skin comprise sunburn inflammation erythema, tanning, and local or systemic immunosuppression.[25] The most deadly form, malignant melanoma, is mostly caused by indirect DNA damage from UVA radiation. This can be seen from the absence of a direct UV signature mutation in 92% of all melanoma.[26] UVC is the highest-energy, most-dangerous type of ultraviolet radiation, and causes adverse effects that can variously be mutagenic or carcinogenic.[27]
Despite the importance of the sun to vitamin D synthesis, it is prudent to limit the exposure of skin to UV radiation from sunlight[28] and from tanning beds.[29] According to the National Toxicology Program Report on Carcinogens from the US Department of Health and Human Services, broad-spectrum UV radiation is a carcinogen whose DNA damage is thought to contribute to most of the estimated 1.5 million skin cancers and the 8,000 deaths due to metastatic melanoma that occur annually in the United States.[28][30] Lifetime cumulative UV exposure to skin is also responsible for significant age-associated dryness, wrinkling, elastin and collagen damage, freckling, age spots and other cosmetic changes. The American Academy of Dermatology advises that photoprotective measures be taken, including the use of sunscreen, whenever one is exposed to the sun.[31] Short-term over-exposure causes the pain and itching of sunburn, which in extreme cases can produce more-severe effects like blistering.
Benefits of optic exposure
Light to the eyes, primarily blue-wavelength light, is important for the entrainment and maintenance of robust circadian rhythms. Exposure to sunlight in the morning is particularly effective; it leads to earlier melatonin onset in the evening and makes it easier to fall asleep. Bright morning light has been shown to be effective against insomnia, premenstrual syndrome and seasonal affective disorder (SAD).[6]
Effects on eyes
Prolonged optical exposure to sunlight, especially intense ultraviolet light, may be linked to cortical cataracts,[32] and high levels of visible light may be linked to macular degeneration.
However, significant daily exposure to bright light may be necessary for children to avoid myopia (nearsightedness).[33]
Short-term over-exposure can cause snow blindness, which is analogous to sunburn of the cornea, or can cause solar retinopathy, which is long-lasting retinal damage and vision impairment from sungazing.[34][35]
Frequent exposure to the sun can cause yellow non-cancerous bumps on the middle part of the sclera of the eye, called pingueculae. It is most common in younger people, mainly those who spend a lot of their time outdoors and do not protect their eyes from UV rays. To decrease the risk of developing pingueculae, it may be wise to wear sunglasses when outdoors, even on overcast days.[36]
Folate degradation
Blood levels of folate, a nutrient vital for fetal development, can be degraded by UV radiation,[37] raising concerns about sun exposure for pregnant women.[38] Lifespan and fertility can be adversely affected for individuals born during peaks of the 11-year solar cycle, possibly because of UV-related folate deficiency during gestation.[39]
Safe level of sun exposure
According to a 2007 study submitted by the University of Ottawa to the US Department of Health and Human Services, there is not enough information to determine a safe level of sun exposure that imposes minimal risk of skin cancer.[40] In addition, there is not yet conclusive evidence on which components of ultraviolet radiation (UVA, UVB, UVC) are actually carcinogenic.[8] UVC is almost completely absorbed by the atmosphere and does not reach the surface in any appreciable quantity.[41] As a result, only the broad-spectrum combination (UVA, UVB, UVC) known as "ultraviolet radiation" is listed as a carcinogen; the components are only "likely to become" known carcinogens. Solar radiation (sunlight) and sunlamps are listed as carcinogens because they contain ultraviolet radiation.[8]
Lifetime sun exposure
There are currently no recommendations on a safe level of total lifetime sun exposure.[40] According to epidemiologist Robyn Lucas at Australian National University, analysis of lifespan versus disease shows that far more lives worldwide could be lost to diseases caused by lack of sunlight than to those caused by too much,[42] and it is inappropriate to recommend total avoidance of sunlight.[43]
Over thousands of years, in many climate zones, genetic selection has helped indigenous human populations adapt toward skin pigmentation levels that provide a healthy level of UV exposure. This largely explains the tendency toward darker-skinned populations in the sunniest tropical environments, and lighter skin tones in less-sunny regions and for those who most need vitamin D for rapid bone growth, specifically children and reproductive-age women. The map below illustrates the geographic distribution of skin color for native populations prior to 1940, based on von Luschan's chromatic scale. These long-term adaptations for optimal health can be confounded by patterns of food, clothing and shelter, especially at a time when large populations have migrated far from the climates for which their skin was genetically adapted.[44][45]

See also
References
- ↑ Osborne JE, Hutchinson PE (August 2002). "Vitamin D and systemic cancer: is this relevant to malignant melanoma?". Br. J. Dermatol. 147 (2): 197–213. PMID 12174089. doi:10.1046/j.1365-2133.2002.04960.x.
- ↑ "Dietary Supplement Fact Sheet: Vitamin D". Office of Dietary Supplements, National Institutes of Health.
- ↑ Cranney A, Horsley T, O'Donnell S, Weiler H, Puil L, Ooi D, Atkinson S, Ward L, Moher D, Hanley D, Fang M, Yazdi F, Garritty C, Sampson M, Barrowman N, Tsertsvadze A, Mamaladze V (August 2007). "Effectiveness and safety of vitamin D in relation to bone health". Evidence report/technology assessment (158): 1–235. PMC 4781354
 . PMID 18088161.
. PMID 18088161. - ↑ John E, Schwartz G, Koo J, Van Den Berg D, Ingles S (June 15, 2005). "Sun Exposure, Vitamin D Receptor Gene Polymorphisms, and Risk of Advanced Prostate Cancer". Cancer Research. 65 (12): 5470–5479. PMID 15958597. doi:10.1158/0008-5472.can-04-3134.
- ↑ Egan K, Sosman J, Blot W (February 2, 2005). "Sunlight and Reduced Risk of Cancer: Is The Real Story Vitamin D?". J Natl Cancer Inst. 97 (3): 161–163. doi:10.1093/jnci/dji047.
- 1 2 Mead MN (April 2008). "Benefits of sunlight: a bright spot for human health". Environmental Health Perspectives. 116 (4): A160–A167. PMC 2290997
 . PMID 18414615. doi:10.1289/ehp.116-a160.
. PMID 18414615. doi:10.1289/ehp.116-a160. - ↑ Lucas RM, Repacholi MH, McMichael AJ (June 2006). "Is the current public health message on UV exposure correct?". Bulletin of the World Health Organization. 84 (6): 485–491. PMC 2627377
 . PMID 16799733. doi:10.2471/BLT.05.026559.
. PMID 16799733. doi:10.2471/BLT.05.026559. - 1 2 3 "13th Report on Carcinogens: Ultraviolet-Radiation-Related Exposures" (PDF). National Toxicology Program. October 2014. Retrieved December 22, 2014.
- ↑ "Risks and Benefits of Sun Exposure" (PDF). Cancer Council Australia. May 3, 2007. Retrieved March 25, 2015.
- ↑ Hayes CE, Nashold FE, Spach KM, Pedersen LB (March 2003). "The immunological functions of the vitamin D endocrine system". Cellular and Molecular Biology. 49 (2): 277–300. PMID 12887108.
- ↑ Holick MF (October 1994). "McCollum Award Lecture, 1994: vitamin D—new horizons for the 21st century". The American Journal of Clinical Nutrition. 60 (4): 619–630. PMID 8092101.
- 1 2 3 Holick, MF (February 2002). "Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health". Current Opinion in Endocrinology, Diabetes and Obesity. 9 (1): 87–98. doi:10.1097/00060793-200202000-00011.
- ↑ Holick MF (2005). "Photobiology of vitamin D". In Feldman, David Henry; Glorieux, Francis H. Vitamin D. Amsterdam: Elsevier Academic Press. ISBN 0-12-252687-2.
- ↑ Holick MF (September 2002). "Sunlight and Vitamin D". Journal of General Internal Medicine. 17 (9): 733–735. PMC 1495109
 . PMID 12220371. doi:10.1046/j.1525-1497.2002.20731.x.
. PMID 12220371. doi:10.1046/j.1525-1497.2002.20731.x. - ↑ Holick MF (July 2007). "Vitamin D deficiency". The New England Journal of Medicine. 357 (3): 266–281. PMID 17634462. doi:10.1056/NEJMra070553.
- ↑ Topiwala, S (July 19, 2012). "25-hydroxy vitamin D test". MedlinePlus. US National Institutes of Health. Retrieved March 25, 2015.
- ↑ Zadshir A, Tareen N, Pan D, Norris K, Martins D (2005). "The prevalence of hypovitaminosis D among US adults: data from the NHANES III". Ethnicity & Disease. 15 (4 Suppl 5): S5–97 – S5–101. PMID 16315387.
- ↑ Nowson C, Margerison C (2002). "Vitamin D intake and vitamin D status of Australians". Med J Aust. 177 (3): 149–152. PMID 12149085.
- ↑ "UV-B Monitoring and Research Program". Colorado State University. Retrieved May 13, 2010.
- ↑ "UV index & UV dose based on GOME". KNMI/TEMIS. Retrieved March 17, 2015.
- ↑ Ascherio A, Munger KL (June 2007). "Environmental risk factors for multiple sclerosis. Part II: Noninfectious factors". Annals of Neurology. 61 (6): 504–513. PMID 17492755. doi:10.1002/ana.21141.
- ↑ Milo R, Kahana E (March 2010). "Multiple sclerosis: geoepidemiology, genetics and the environment". Autoimmun Rev. 9 (5): A387–A394. PMID 19932200. doi:10.1016/j.autrev.2009.11.010.
- ↑ Ascherio A, Munger KL, Simon KC (June 2010). "Vitamin D and multiple sclerosis". Lancet Neurol. 9 (6): 599–612. PMID 20494325. doi:10.1016/S1474-4422(10)70086-7.
- ↑ Koch MW, Metz LM, Agrawal SM, Yong VW (2013). "Environmental factors and their regulation of immunity in multiple sclerosis". J. Neurol. Sci. 324 (1–2): 10–16. PMID 23154080. doi:10.1016/j.jns.2012.10.021.
- ↑ Matsumu, Y.; Ananthaswamy, H. N. (2004). "Toxic effects of ultraviolet radiation on the skin". Toxicology and Applied Pharmacology. 195 (3): 298–308. PMID 15020192. doi:10.1016/j.taap.2003.08.019.
- ↑ Davies H.; Bignell G. R.; Cox C. (June 2002). "Mutations of the BRAF gene in human cancer". Nature. 417 (6892): 949–954. PMID 12068308. doi:10.1038/nature00766.
- ↑ C.Michael Hogan. 2011. Sunlight. eds. P.Saundry & C.Cleveland. Encyclopedia of Earth.
- 1 2 Wolpowitz D, Gilchrest BA (February 2006). "The vitamin D questions: how much do you need and how should you get it?". Journal of the American Academy of Dermatology. 54 (2): 301–317. PMID 16443061. doi:10.1016/j.jaad.2005.11.1057.
- ↑ International Agency for Research on Cancer Working Group on artificial ultraviolet (UV) light and skin cancer (March 2007). "The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: A systematic review". International Journal of Cancer. 120 (5): 1116–1122. PMID 17131335. doi:10.1002/ijc.22453.
- ↑ "Ultraviolet (UV) Radiation, Broad Spectrum and UVA, UVB, and UVC". National Toxicology Program. January 5, 2009. Retrieved May 13, 2010.
- ↑ American Academy of Dermatology. Position statement on vitamin D. November 1, 2008.
- ↑ West SK, Duncan DD, Muñoz B, et al. (1998). "Sunlight exposure and risk of lens opacities in a population-based study: the Salisbury Eye Evaluation project". JAMA. 280 (8): 714–718. PMID 9728643. doi:10.1001/jama.280.8.714. Retrieved March 14, 2015.
- ↑ Dolgin, Elie (19 March 2015). "The Myopia Boom". Nature News. 519: 276–278. doi:10.1038/519276a. Retrieved 2015-10-08.
- ↑ Chen JC, Lee LR (2004). "Solar retinopathy and associated optical coherence tomography findings" (PDF). Clin Exp Optom. 87 (6): 390–393. PMID 15575813. doi:10.1111/j.1444-0938.2004.tb03100.x.
- ↑ Kallmark FP, Ygge J (2005). "Photo-induced foveal injury after viewing a solar eclipse". Acta Ophthalmol Scand. 83 (5): 586–589. PMID 16187997. doi:10.1111/j.1600-0420.2005.00511.x.
- ↑ Lusby, MD, Franklin; Zieve, MD, AHA, David; Ogilvie, PhD, Isla. "Pinguecula". MedicinePlus. U.S. National Library of Medicine. Retrieved 28 October 2016.
- ↑ Borradale D, Isenring E, Hacker E, Kimlin MG (February 2014). "Exposure to solar ultraviolet radiation is associated with a decreased folate status in women of childbearing age". Journal of Photochemistry and Photobiology B: Biology. 131: 90–95. doi:10.1016/j.jphotobiol.2014.01.002.
- ↑ "Pregnancy and Tanning". American Pregnancy Association. January 2014. Retrieved January 11, 2015.
- ↑ Skjærvø GR, Fossøy F, Røskaft E (February 2015). "Solar activity at birth predicted infant survival and women’s fertility in historical Norway". Proc. R. Soc. B. 282 (1801): 20142032. PMC 4308994
 . PMID 25567646. doi:10.1098/rspb.2014.2032.
. PMID 25567646. doi:10.1098/rspb.2014.2032. - 1 2 Cranney A, Horsley T, O'Donnell S, et al. (August 2007). "Effectiveness and safety of vitamin D in relation to bone health". Evidence Report/Technology Assessment (158): 1–235. PMC 4781354
 . PMID 18088161.
. PMID 18088161. - ↑ Brannon, H (January 1, 2014). "UVC Radiation". About.com. Retrieved March 25, 2015.
- ↑ Lucas RM, McMichael AJ, Armstrong BK, Smith WT (June 2008). "Estimating the global disease burden due to ultraviolet radiation exposure" (PDF). International Journal of Epidemiology. 37 (3): 654–667. PMID 18276627. doi:10.1093/ije/dyn017.
- ↑ Lucas RM, Ponsonby AL (December 2002). "Ultraviolet radiation and health: friend and foe". Medical Journal of Australia. 177 (11): 594–598. Retrieved March 24, 2015.
- ↑ Webb, AR (2006). "Who, what, where, and when: influences on cutaneous vitamin D synthesis". Progress in Biophysics and Molecular Biology. 92 (1): 17–25. PMID 16766240. doi:10.1016/j.pbiomolbio.2006.02.004.
- ↑ Jablonski, Nina (2012). Living Color. University of California Press. ISBN 978-0-520-25153-3.