Levator ani
| Levator ani | |
|---|---|
 Left Levator ani seen from within. | |
 Coronal section through the male anal canal. B. Cavity of urinary bladder V.D. Vas deferens. S.V. Seminal vesicle. R. Second part of rectum. A.C. Anal canal. L.A. Levator ani. I.S. Internal anal sphincter. E.S External anal sphincter. | |
| Details | |
| Origin | Inner surface of the side of the lesser pelvis |
| Insertion | Inner surface of coccyx, levator ani of opposite side, and into structures that penetrate it. |
| Artery | Inferior gluteal artery |
| Nerve | |
| Actions | Supports the viscera in pelvic cavity |
| Identifiers | |
| Latin | Musculus levator ani |
| Dorlands /Elsevier | m_22/12549567 |
| TA | A04.5.04.002 |
| FMA | 19087 |
The levator ani is a broad, thin muscle, situated on either side of the pelvis. It is formed from three muscle components: the puborectalis, the pubococcygeus muscle (which includes the puborectalis) and the iliococcygeus muscle.
It is attached to the inner surface of each side of the lesser pelvis, and these unite to form the greater part of the pelvic floor. The coccygeus muscle completes the pelvic floor which is also called the pelvic diaphragm.
It supports the viscera in the pelvic cavity, and surrounds the various structures that pass through it.
The levator ani is the main pelvic floor muscle and contracts rhythmically during orgasm.[3]
Structure
The levator ani is divided into three parts:
- Iliococcygeus muscle
- Pubococcygeus muscle
- Puborectalis muscle
The iliococcygeus arises from the inner side of the ischium (the lower and back part of the hip bone) and from the posterior part of the tendinous arch of the obturator fascia, and is attached to the coccyx and anococcygeal body; it is usually thin, and may be absent, or be largely replaced by fibrous tissue. An accessory slip at its posterior part is sometimes named the iliosacralis.
The pubococcygeus muscle is then divided into three parts on its own.
- The true pubococcygeus
- puborectalis
- pubovaginalis (female) or puboprostaticus (male)
Origin and insertion
The levator ani arises, in front, from the posterior surface of the superior pubic ramus lateral to the symphysis; behind, from the inner surface of the spine of the ischium; and between these two points, from the obturator fascia.
Posteriorly, this fascial origin corresponds, more or less closely, with the tendinous arch of the pelvic fascia, but in front, the muscle arises from the fascia at a varying distance above the arch, in some cases reaching nearly as high as the canal for the obturator vessels and nerve.
The fibers pass downward and backward to the middle line of the floor of the pelvis; the most posterior are inserted into the side of the last two segments of the coccyx; those placed more anteriorly unite with the muscle of the opposite side, in a median fibrous ridge called the anococcygeal body or raphe, which extends between the coccyx and the margin of the anus.
The middle fibers are inserted into the side of the rectum, blending with the fibers of the Sphincter muscles; lastly in the male, the anterior fibers descend upon the side of the prostate to unite beneath it with the muscle of the opposite side, joining with the fibers of the external anal sphincter and transverse perineal muscles, at the central tendinous point of the perineum.
The anterior portion is occasionally separated from the rest of the muscle by connective tissue.
From this circumstance, as well as from its peculiar relation with the prostate, which it supports as in a sling, it has been described as a distinct muscle, under the name of levator prostatæ.
In the female the anterior fibers of the levator ani descend upon the side of the vagina.
Innervation
The levator ani muscles are mostly innervated by the pudendal nerve, perineal nerve and inferior rectal nerve acting together.[4]
Variation
In addition, sacral spinal nerves (S3, S4) innervate the muscles directly as well (in ~70%[4] of people). Sometimes (in ~40%[4] of people) the inferior rectal nerve innervates the levator ani muscles independently of the pudendal nerve.
Pubococcygeus
| Pubococcygeus muscle | |
|---|---|
| Details | |
| Origin | back of the pubis and from the anterior part of the obturator fascia |
| Insertion | coccyx and sacrum |
| Nerve | S3, S4 |
| Actions | controls urine flow and contracts during orgasm |
| Identifiers | |
| Latin | musculus pubococcygeus |
| Dorlands /Elsevier | m_22/12550316 |
| TA | A04.5.04.002 |
| FMA | 19087 |
The pubococcygeus muscle or PC muscle is a hammock-like muscle, found in both sexes, that stretches from the pubic bone to the coccyx (tail bone) forming the floor of the pelvic cavity and supporting the pelvic organs. It is part of the levator ani muscle.
Structure
The pubococcygeus arises from the back of the pubis and from the anterior part of the obturator fascia, and is directed backward almost horizontally along the side of the anal canal toward the coccyx and sacrum, to which it finds attachment.
Between the termination of the vertebral column and the anus, the two pubococcygei muscles come together and form a thick, fibromuscular layer lying on the raphe (ridge) or (anococcygeal body) formed by the iliococcygei.
The greater part of this muscle is inserted into the coccyx and into the last one or two pieces of the sacrum.
Variation
This insertion into the vertebral column is, however, not accepted by all observers.
Function
The pubococcygeus muscle controls urine flow and contracts during orgasm as well as assisting in male ejaculation.[5] It also aids in childbirth as well as core stability.[6]
A strong pubococcygeus muscle has also been linked to a reduction in urinary incontinence and proper positioning of the baby's head during childbirth.
Kegel exercises
The Kegel exercises are a series of voluntary contractions of all the perineal muscles. Such movement is done in an effort to strengthen all the striated muscles in the perineum's area. They are often referred to simply as "kegels", named after their founder, Dr. Arnold Kegel.[7] These exercises also serve to contract, among others, the ischiocavernosus, bulbospongiosus, and cremaster muscle in men, as voluntary contraction of the pubococcygeus muscle also engages the cremasteric reflex, which lifts the testicles up, although this does not occur in all men. Kegel exercises have been prescribed to ameliorate erectile dysfunction due to venous leakage and to help men control premature ejaculation[8] and to treat urinary incontinence in both sexes.[9][10]
Puborectalis
| Puborectalis muscle | |
|---|---|
 The posterior aspect of the rectum exposed by removing the lower part of the sacrum and the coccyx. (Puborectalis not labeled, but levator ani labeled at bottom right, and external anal sphincter labeled at bottom center.) | |
| Details | |
| Origin | lower part of the pubic symphysis, superior fascia of the urogenital diaphragm |
| Nerve | S3, S4. levator ani nerve[11] |
| Actions | inhibit defecation |
| Identifiers | |
| Latin | musculus puborectalis |
| Dorlands /Elsevier | m_22/12550328 |
| TA | A04.5.04.002 |
| FMA | 19087 |
The fibers which form a sling for the rectum are named the puborectalis. They arise from the lower part of the pubic symphysis, and from the superior fascia of the urogenital diaphragm.
They meet with the corresponding fibers of the opposite side around the lower part of the rectum, and form for it a strong sling. Relaxation increases the angle between rectum and anus, allowing defecation in conjunction with relaxation of the internal and external anal sphincters.
Function
The levator ani muscles are responsible for "wagging" the tail in tailed quadrupeds. These muscles are not as strong in the human, as tail-wagging is more demanding than the support function that the muscles serve in humans.[12]
Clinical signifiance
Levator ani syndrome
Levator ani syndrome (also called levator spasm, puborectalis syndrome, chronic proctalgia, piriformis syndrome, pelvic tension myalgia, levator syndrome, and proctodynia) is episodic rectal pain that can waken the patient from sleep, caused by spasm of the levator ani muscle.<ref http://www.merckmanuals.com/professional/gastrointestinal-disorders/anorectal-disorders/levator-syndrome >Levator Syndrome, by Parswa Ansari, MD 7/2014, Merck Manuals</ref>[13][14] The cause is unknown, however it has been suggested that inflammation of the arcus tendon is the possible cause of levator ani syndrome.[15]
Symptoms include a dull ache to the left 2 inches above the Anus or higher in the rectum and a feeling of constant rectal pressure or burning. The pain may also be felt in the low pelvis or perineum.
The discomfort may be relieved by walking or pelvic tightening exercises similar to Kegel exercises. Other treatments include massage of the muscle, warm baths, muscle relaxant medications, therapeutic ultrasound and biofeedback. Electrical stimulation of the levator ani muscle has been used to try to break the spastic cycle. Injection of botulinum toxin A has also been used.
Variants of levator ani syndrome include proctalgia fugax (fleeting pain in the rectum) and coccydynia (pain in the coccygeal region). Proctalgia fugax and levator ani syndrome have not been found to be of psychosomatic origin, although stressful events may trigger attacks.[13] Patients with levator ani syndrome also have "significant elevations on the hypochondriasis, depression, and hysteria scales of the Minnesota Multiphasic Personality Inventory," which is also the case in general among chronic pain sufferers.[14]
Additional images
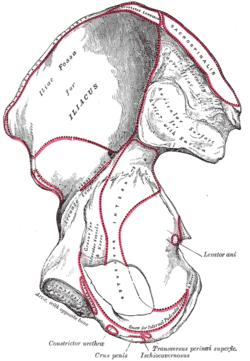 Right hip bone. Internal surface.
Right hip bone. Internal surface. Coronal section of pelvis, showing arrangement of fasciæ. Viewed from behind.
Coronal section of pelvis, showing arrangement of fasciæ. Viewed from behind. Muscles of male perineum.
Muscles of male perineum.
 The arteries of the pelvis.
The arteries of the pelvis. Sacral plexus of the right side.
Sacral plexus of the right side.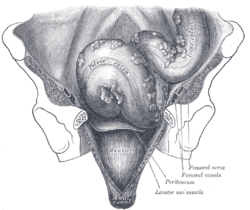 Iliac colon, sigmoid or pelvic colon, and rectum seen from the front, after removal of pubic bones and bladder.
Iliac colon, sigmoid or pelvic colon, and rectum seen from the front, after removal of pubic bones and bladder. The posterior aspect of the rectum exposed by removing the lower part of the sacrum and the coccyx.
The posterior aspect of the rectum exposed by removing the lower part of the sacrum and the coccyx.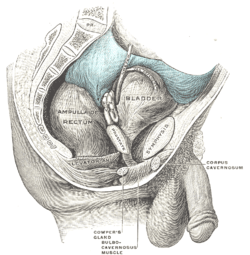 Male pelvic organs seen from right side.
Male pelvic organs seen from right side.
See also
| Wikimedia Commons has media related to Levator ani. |
References
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
- ↑ Essential Clinical Anatomy. K.L. Moore & A.M. Agur. Lippincott, 2nd ed. 2002. Page 217
- ↑ Wallner C, Maas C, Dabhoiwala N, Lamers W, Deruiter M (2006). "Evidence for the innervation of the puborectalis muscle by the levator ani nerve". Neurogastroenterol Motil. 18 (12): 1121–1122. PMID 17109696. doi:10.1111/j.1365-2982.2006.00846.x.
- ↑ Christopher R. Chapple (2006). Multidisciplinary Management of Female Pelvic Floor Disorders. Churchill Livingstone. pp. 4–. ISBN 978-0-443-07272-7.
- 1 2 3 Grigorescu BA, Lazarou G, Olson TR, et al. (2008). "Innervation of the levator ani muscles: description of the nerve branches to the pubococcygeus, iliococcygeus, and puborectalis muscles". Int Urogynecol J Pelvic Floor Dysfunct. 19 (1): 107–116. PMID 17565421. doi:10.1007/s00192-007-0395-8.
- ↑ Marieb, Elaine (2013). Anatomy & physiology : books a la carte edition. Benjamin-Cummings. p. 895. ISBN 9780321887603.
- ↑ "Core stabilization, Core Coordination, article by Aline Newton, M.A., certified Advanced Rolfer, the biomechanics of core stabilization, with core as a center of movement instead of a center of holding". Alinenewton.com. Retrieved 2012-02-20.
- ↑ Kegel exercises Gannet Health Services. Cornwell University website
- ↑ How To do Kegel Exercises (for men) Silverberg, Corey. About.com
- ↑ Dumoulin, Chantale; Hay-Smith, E. Jean C.; Mac Habée-Séguin, Gabrielle (2014-05-14). "Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women". The Cochrane Database of Systematic Reviews (5): CD005654. ISSN 1469-493X. PMID 24823491. doi:10.1002/14651858.CD005654.pub3.
- ↑ Anderson, Coral A.; Omar, Muhammad Imran; Campbell, Susan E.; Hunter, Kathleen F.; Cody, June D.; Glazener, Cathryn M. A. (2015-01-20). "Conservative management for postprostatectomy urinary incontinence". The Cochrane Database of Systematic Reviews. 1: CD001843. ISSN 1469-493X. PMID 25602133. doi:10.1002/14651858.CD001843.pub5.
- ↑ Wallner C, Maas C, Dabhoiwala N, Lamers W, Deruiter M (2006). "Evidence for the innervation of the puborectalis muscle by the levator ani nerve.". Neurogastroenterol Motil. 18 (12): 1121–2. PMID 17109696. doi:10.1111/j.1365-2982.2006.00846.x.
- ↑ Sloan, Ethel (2001, p. 53). Biology of Women, Wisconsin: CENGAGE Delmar Learning. ISBN 0-7668-1142-5 (excerpt available here)
- 1 2 Giulio Aniello Santoro; Andrzej Paweł Wieczorek; Clive I. Bartram (27 October 2010). Pelvic Floor Disorders: Imaging and Multidisciplinary Approach to Management. Springer. p. 601. ISBN 978-88-470-1542-5.
- 1 2 Bharucha AE, Trabuco E (September 2008). "Functional and chronic anorectal and pelvic pain disorders". Gastroenterology Clinics of North America. 37 (3): 685–96, ix. PMC 2676775
 . PMID 18794003. doi:10.1016/j.gtc.2008.06.002.
. PMID 18794003. doi:10.1016/j.gtc.2008.06.002. - ↑ Park DH, Yoon SG, Kim KU, et al. (May 2005). "Comparison study between electrogalvanic stimulation and local injection therapy in levator ani syndrome". International Journal of Colorectal Disease. 20 (3): 272–6. PMID 15526112. doi:10.1007/s00384-004-0662-9.
External links
- Anatomy figure: 41:05-00 at Human Anatomy Online, SUNY Downstate Medical Center—"Muscles of the female superficial perineal pouch."
- Anatomy figure: 42:04-00 at Human Anatomy Online, SUNY Downstate Medical Center—"Muscles of the male superficial perineal pouch."
- Anatomy photo:43:16-0102 at the SUNY Downstate Medical Center—"Muscles of the Pelvic Diaphragm"
- Anatomy image:9072 at the SUNY Downstate Medical Center
- Anatomy image:9089 at the SUNY Downstate Medical Center
- Anatomy image:9871 at the SUNY Downstate Medical Center
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- perineum at The Anatomy Lesson by Wesley Norman (Georgetown University) (analtriangle3) * pelvis at The Anatomy Lesson by Wesley Norman (Georgetown University) (femalepelvicdiaphragm, malepelvicdiaphragm)
- Merck Manual article on levator ani syndrome