Pleurisy
| Pleurisy | |
|---|---|
| Synonyms | Pleuritis, pleuritic chest pain[1] |
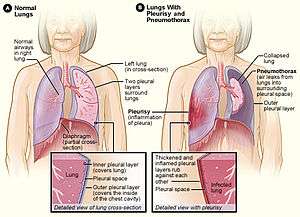 | |
| Figure A shows normal anatomy. Figure B shows lungs with pleurisy in the right lung and a pneumothorax of the left lung. | |
| Specialty | Pulmonology |
| Symptoms | Sharp chest pain[1] |
| Causes | Viral infection, pneumonia, pulmonary embolism[2] |
| Diagnostic method | Chest X-ray, electrocardiogram (ECG), blood tests[3] |
| Similar conditions | Pericarditis, heart attack, cholecystitis[3] |
| Treatment | Based on the underlying cause[3] |
| Medication | Paracetamol (acetaminophen), ibuprofen[4] |
| Frequency | 1 million cases per year (United States)[5] |
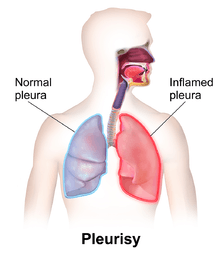
Pleurisy, also known as pleuritis, is inflammation of the membranes (pleurae) that surround the lungs and line the chest cavity. This can result in a sharp chest pain with breathing.[1] Occasionally the pain may be a constant dull ache. Other symptoms may include shortness of breath, cough, fever, or weight loss depending on the underlying cause.[6]
The most common cause is a viral infection. Other causes include pneumonia, pulmonary embolism, autoimmune disorders, lung cancer, following heart surgery, pancreatitis, chest trauma, and asbestosis. Occasionally the cause remains unknown.[2] The underlying mechanism involves the rubbing together of the pleurae instead of smooth gliding.[1] Other conditions that can produce similar symptoms include pericarditis, heart attack, cholecystitis, and pneumothorax. Diagnosis may include a chest X-ray, electrocardiogram (ECG), and blood tests.[3][7]
Treatment depends on the underlying cause.[3] Paracetamol and ibuprofen may be used to help with the pain.[4] Incentive spirometry may be recommended to encourage larger breaths. About one million people are affected in the United States each year.[5] Descriptions of the condition date from at least as early as 400 BC by Hippocrates.[8]
Signs and symptoms
The defining symptom of pleurisy is a sudden sharp, stabbing, burning or dull pain in the right or left side of the chest during breathing, especially when one inhales and exhales.[9] It feels worse with deep breathing, coughing, sneezing, or laughing. The pain may stay in one place, or it may spread to the shoulder or back.[10] Sometimes, it becomes a fairly constant dull ache.[11]
Depending on its cause, pleuritic chest pain may be accompanied by other symptoms:[12]
- Dry cough
- Fever and chills
- Rapid, shallow breathing
- Shortness of breath
- Tachycardia
- Sore throat followed by pain and swelling in the joints
Causes
The pleural space can be invaded by fluid, air, and particles from different parts of the body which fairly complicates the diagnosis.[12][13] Viral infection (coxsackie B virus, HRSV, CMV, adenovirus, EBV, parainfluenza, influenza) is the most common cause of pleurisy. However, many other different conditions can cause pleuritic chest pain:[11]
- Aortic dissections
- Autoimmune disorders such as systemic lupus erythematosus (or drug-induced lupus erythematosus), Autoimmune hepatitis (AIH) and rheumatoid arthritis
- Bacterial infections associated with pneumonia and tuberculosis
- Chest injuries (blunt or penetrating)
- Familial Mediterranean fever, an inherited condition that often causes fever and swelling in the abdomen or the lungs
- Fungal or parasitic infections
- Heart surgery, especially coronary-artery bypass grafting
- Cardiac problems (ischemia, pericarditis)
- Inflammatory bowel disease
- Lung cancer and lymphoma
- Other lung diseases like cystic fibrosis, sarcoidosis, asbestosis, lymphangioleiomyomatosis, and mesothelioma
- Pneumothorax
- Pulmonary embolisms, which are blood clots that enter the lungs
When the space between the pleurae starts to fill with fluid, as in pleural effusion, the chest pain can be eased but a shortness of breath can result, since the lungs need room to expand during breathing. Some cases of pleuritic chest pain are idiopathic, which means that the exact cause cannot be determined.
Diagnosis
A diagnosis of pleurisy or another pleural condition is based on a medical history, physical examinations, and diagnostic tests.[12] The goals are to rule out other sources of the symptoms and to find the cause of the pleurisy so that the underlying disorder can be treated.
Physical examination
A doctor uses a stethoscope to listen to the breathing. This method detects any unusual sounds in the lungs. A person with pleurisy may have inflamed layers of the pleurae that make a rough, scratchy sound as they rub against each other during breathing. This is called pleural friction rub.
Diagnostic tests
Depending on the results of the physical examination, diagnostic tests are sometimes performed.
Chest x-ray
A chest x-ray takes a picture of the heart and lungs. It may show air or fluid in the pleural space. It also may show the cause (e.g., pneumonia, a fractured rib, or a lung tumor) of the pleurisy.
Sometimes an x-ray is taken while lying on the painful side. This may show fluid, as well as changes in fluid position, that did not appear in the vertical x-ray.
Blood test
Blood tests can detect bacterial or viral infections, pneumonia, rheumatic fever, a pulmonary embolism, or lupus.
ECG
Electrocardiography test can determine if a heart condition contributes to the symptoms.
Ultrasound
Ultrasonography uses sound waves to create an image. It may show where fluid is located in the chest. It also can show some tumors. Although ultrasound may detect fluid around the lungs, also known as a pleural effusion, sound waves are scattered by air. Therefore, an actual picture of the lungs cannot be obtained with ultrasonography.
Computed tomography (CT) scan
A CT scan provides a computer-generated picture of the lungs that can show pockets of fluid. It also may show signs of pneumonia, a lung abscess, or a tumor.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI), also called nuclear magnetic resonance (NMR) scanning, uses powerful magnets to show pleural effusions and tumors.
Arterial blood gas
In arterial blood-gas sampling, a small amount of blood is taken from an artery, usually in the wrist. The blood is then checked for oxygen and carbon-dioxide levels. This test shows how well the lungs are taking in oxygen.
Thoracentesis
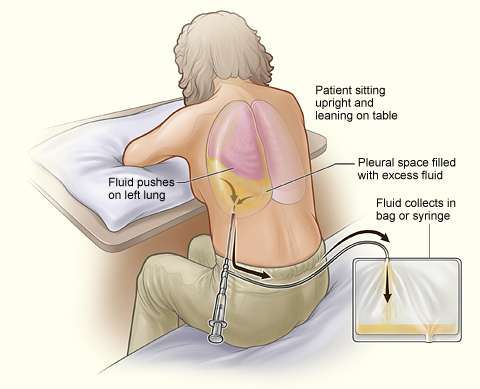
Once the presence of an excess fluid in the pleural cavity, or pleural effusion, is suspected and location of fluid is confirmed, a sample of fluid can be removed for testing.[14] The procedure to remove fluid in the chest is called a diagnostic thoracentesis.[15] The doctor inserts a small needle or a thin, hollow, plastic tube in the chest wall and withdraws fluid.[16]
Thoracentesis can be done in the doctor's office or at the hospital. Ultrasound is used to guide the needle to the fluid that is trapped in small pockets around the lungs.
Thoracentesis usually does not cause serious complications. Generally, a chest x-ray is done after the procedure to evaluate the lungs. Possible complications of thoracentesis include the following:
- Bleeding and bruising where the needle went in. In rare cases, bleeding may occur in or around the lung. The doctor can use a chest tube to drain the blood. In some cases, surgery is needed.
- Infection where the needle went in
- Injury to the liver or spleen (in rare cases)
- Pain.
- Pneumothorax, or buildup of air in the pleural space, with a collapsed or partially collapsed lung. Sometimes air comes in through the needle or the needle makes a hole in the lung. Usually, a hole will seal itself. But sometimes air can build up around the lung and make it collapse. A chest tube can remove the air and let the lung expand again.
The lung fluid is examined under a microscope and is evaluated for the presence of chemicals and for its color and texture. The degree of clarity is an indicator of infection, cancer, or other conditions that may be causing the buildup of fluid or blood in the pleural space.
Biopsy
If tuberculosis or cancer is suspected, a small piece of the pleura may be examined under a microscope to make a definitive diagnosis. This is called a biopsy.
Several approaches to taking tissue samples are available
- Insertion of a needle through the skin on the chest to remove a small sample of the outer layer of the pleura.
- Insertion of a small tube with a light on the end (endoscope) into tiny cuts in the chest wall in order to visualize the pleura. Small pieces of tissue can be biopsied though the endoscope.
- Removal of a sample of the pleura through a small cut in the chest wall. This is called an open pleural biopsy. It is usually done if the sample from the needle biopsy is too small for an accurate diagnosis.
Treatment
Treatment has several goals:[12]
- Relief of symptoms
- Removal of the fluid, air, or blood from the pleural space
- Treatment of the underlying condition
Procedures
If large amounts of fluid, air, or blood are not removed from the pleural space, they may cause the lung to collapse.
The surgical procedures used to drain fluid, air, or blood from the pleural space are as follows:
- During thoracentesis, a needle or a thin, hollow, plastic tube is inserted through the ribs in the back of the chest into the chest wall. A syringe is attached to draw fluid out of the chest. This procedure can remove more than 6 cups (1.5 litres) of fluid at a time.
- When larger amounts of fluid must be removed, a chest tube may be inserted through the chest wall. The doctor injects a local painkiller into the area of the chest wall outside where the fluid is. A plastic tube is then inserted into the chest between two ribs. The tube is connected to a box that suctions the fluid out. A chest x-ray is taken to check the tube's position.
- A chest tube is also used to drain blood and air from the pleural space. This can take several days. The tube is left in place, and the patient usually stays in the hospital during this time.
- Sometimes the fluid contains thick pus or blood clots, or it may have formed a hard skin or peel. This makes it harder to drain the fluid. To help break up the pus or blood clots, the doctor may use the chest tube to put certain medicines into the pleural space. These medicines are called fibrinolytics. If the pus or blood clots still do not drain out, surgery may be necessary.
Medications
A couple of medications are used to relieve pleurisy symptoms:
- Paracetamol (acetaminophen) or anti-inflammatory agents to control pain and decrease inflammation. Only indomethacin (brand name Indocin) has been studied with respect to relief of pleurisy.[17]
- Codeine-based cough syrups to control the cough
There may be a role for the use of corticosteroids (for tuberculous pleurisy), tacrolimus (Prograf) and methotrexate (Trexall, Rheumatrex) in the treatment of pleurisy. Further studies are needed.
Lifestyle changes
The following may be helpful in the management of pleurisy:
- Lying on the painful side may be more comfortable
- Breathing deeply and coughing to clear mucus as the pain eases. Otherwise, pneumonia may develop.
- Getting rest
Treating the cause
Ideally, the treatment of pleurisy is aimed at eliminating the underlying cause of the disease.
- If the pleural fluid is infected, treatment involves antibiotics and draining the fluid. If the infection is tuberculosis or from a fungus, treatment involves long-term use of antibiotics or antifungal medicines.
- If the fluid is caused by tumors of the pleura, it may build up again quickly after it is drained. Sometimes anti-tumor medicines will prevent further fluid buildup. If they don't, the doctor may seal the pleural space. This is called pleurodesis. Pleurodesis involves the drainage of all the fluid out of the chest through a chest tube. A substance is inserted through the chest tube into the pleural space. This substance irritates the surface of the pleura. This causes the two layers of the pleurae to squeeze shut so there is no room for more fluid to build up.
- Chemotherapy or radiation treatment also may be used to reduce the size of the tumors.
- If congestive heart failure is causing the fluid buildup, treatment usually includes diuretics and other medicines.
The treatment for pleurisy depends on its origin and is prescribed by a physician on a base of an individual assessment.[18] Paracetamol (acetaminophen) and amoxicillin, or other antibiotics in case of bacterial infections, are common remedies dispensed by doctors to relieve the initial symptoms and pain in the chest, while viral infections are self-limited. Non-steroidal anti-inflammatory drugs (NSAIDs), preferably indometacin, are usually employed as pain control agents.[12]
Alternative treatments
A number of alternative or complementary medicines are being investigated for their anti-inflammatory properties, and their use in pleurisy. At this time, clinical trials of these compounds have not been performed.
Extracts from the Brazilian folk remedy Wilbrandia ebracteata ("Taiuia") have been shown to reduce inflammation in the pleural cavity of mice.[19][20] The extract is thought to inhibit the same enzyme, cyclooxygenase-2 (COX-2), as the non-steroidal anti-inflammatory drugs.[20]
Related problems
Pleurisy is often associated with complications that affect the pleural space.
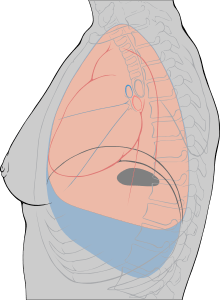
Pleural effusion
In some cases of pleurisy, excess fluid builds up in the pleural space. This is called a pleural effusion. The buildup of fluid usually forces the two layers of the pleura apart so they don't rub against each other when breathing. This can relieve the pain of pleurisy. A large amount of extra fluid can push the pleura against the lung until the lung, or a part of it, collapses. This can make it hard to breathe.
In some cases of pleural effusion, the extra fluid gets infected and turns into an abscess. This is called an empyema.
Pleural effusion involving fibrinous exudates in the fluid may be called fibrinous pleurisy. It sometimes occurs as a later stage of pleurisy.
A person can develop a pleural effusion in the absence of pleurisy. For example, pneumonia, heart failure, cancer, or a pulmonary embolism can lead to a pleural effusion.
Pneumothorax
Air or gas also can build up in the pleural space. This is called a pneumothorax. It can result from acute lung injury or a lung disease like emphysema. Lung procedures, like surgery, drainage of fluid with a needle, examination of the lung from the inside with a light and a camera, or mechanical ventilation, also can cause a pneumothorax.
The most common symptom is sudden pain in one side of the lung and shortness of breath. A pneumothorax also can put pressure on the lung and cause it to collapse.
If the pneumothorax is small, it may go away on its own. If large, a chest tube is placed through the skin and chest wall into the pleural space to remove the air.
Hemothorax
Blood also can collect in the pleural space. This is called hemothorax. The most common cause is injury to the chest from blunt force or surgery on the heart or chest. Hemothorax also can occur in people with lung or pleural cancer.
Hemothorax can put pressure on the lung and force it to collapse. It also can cause shock, a state of hypoperfusion in which an insufficient amount of blood is able to reach the organs.
Prognosis
Pleurisy and other disorders of the pleurae can be serious, depending on what caused them. Generally, pleurisy treatment has an excellent prognosis, but if left untreated it can cause severe complications. For example, a resulting pulmonary heart disease cor pulmonale, which manifests itself with an inflammation of the arms and legs, can lead to heart failure. If the conditions that caused the pleurisy or other pleural disorders were adequately diagnosed and treated early, one can expect a full recovery. Help of a pulmonologist (respiratory physician in the U.K. and Australia) may be enlisted to address the underlying cause and chart post-illness rehabilitation.
Notable cases
- Gaius Marius, a Roman general and statesman, according to Plutarch died of the disease in 86 BC.[21]
- Flavius Constantius III, a co-emperor of the Western Roman Empire, died of pleurisy according to Sidonius Apollinaris on 2 September 421 AD.[22]
- Charlemagne, known as the father of Europe for reuniting much of the Roman Empire, died in 814 of pleurisy.[23]
- Catherine de' Medici, sometimes described as a "wife of one King and mother of three others", died from pleurisy in January 1589 at age 69.[24]
- Benjamin Franklin developed fever and chest pain in 1790 at the age of 84. He spent ten days in bed having severe cough and difficulty breathing. He died after an abscess in his lungs burst from what is believed to be a case of pleurisy.[25]
- Juan O'Donojú, last viceroy of the Spanish colony of New Spain (Mexico), died of pleurisy on 8 October 1821.[26]
- Francis Scott Key died in 1843 at the home of his daughter Elizabeth Howard in Baltimore from pleurisy.[27]
- William Wordsworth, the English poet, died of pleurisy aged 80 on 23 April 1850.[28]
- Dominic Savio, Italian Saint, became ill and died in March 1857 at the age of 14 possibly from pleurisy.[29]
- Tad Lincoln, the fourth and youngest son of Abraham Lincoln, had difficulty breathing when lying down and had to sleep sitting in a chair, and probably died of pleuristic attack, which was believed to be tubercular in origin, in Chicago in 1871 at age 18.[30]
- Devil Anse Hatfield, a leader of the Hatfield clan and the driving force of the infamous Hatfield–McCoy feud, had a bout of pleurisy in the 1890s (probably 1897).[31]
- Frank C. Stanley, former Peerless Quartet member, died of pleurisy at the age of 41 on 12 December 1910 at his home in Orange.[32]
- Mahatma Gandhi suffered from pleurisy during the First World War, while he was in London.[33]
- Enrico Caruso was struggling with pleurisy in the winter of 1920-1921, which contributed to his premature death.[34][35]
- Eli Bowen, a circus performer known as "The Legless Wonder", or "The Legless Acrobat", died on 2 May 1924 in Coney Island of pleurisy days before a scheduled performance for The Dreamland Circus at age 79.[36]
- Erik Satie, French composer, died from pleurisy at l'Hôpital St. Joseph on 1 July 1925.[37]
- Rudolph Valentino, an international movie star, died in August 1926 from pleurisy at age 31.[38]
- Alvin Kraenzlein was the first athlete to win four Olympic titles in a single event at the 1900 Summer Olympics in Paris. He suffered from bouts of pleurisy at the end of 1927 and died from a related complication early 1928 at the age of 51.[39]
- Thomas Hardy, English novelist and poet, became ill with pleurisy and died of related causes in 1928 at age 87.[40]
- Anna Pavlova, one of the world's most famous ballerinas, died unexpectedly of pleurisy at age 49 at the Hotel des Indes in The Hague in January 1931,[41]
- Florenz Ziegfeld, Jr., a Broadway impresario, who was credited with staging several hit musicals including Show Boat (1927), died on 22 July 1932 of pleurisy after a lung infection at age 65.[42]
- Kenji Miyazawa, a Japanese poet and writer, suffered from chronic pleurisy and died of pneumonia in September 1933 at age 37.[43]
- Nino Manfredi, prominent actor in the commedia all'italiana genre, was given three months to live for his bilateral pleurisy in 1937. He eventually survived and died at age 83 in 2004.[44]
- Sir Robert Chesebrough, inventor of Vaseline, suffered pleurisy in his 50s and is said to have treated it by rubbing his whole body with petroleum jelly.[45]
- Carson McCullers, author of The Heart Is a Lonely Hunter, was diagnosed with influenza and pleurisy in 1944.[46]
- Ringo Starr, former Beatles drummer and solo artist, had chronic-pleurisy at age 13 in 1953.[47]
- LeBron James, an American professional basketball player, was diagnosed with pleurisy after being admitted to the Cleveland Clinic in October 2005 with complaints about chest pain during practice.[48]
- Ken Griffey Jr., an American professional baseball player, complained of soreness in the chest and, after a chest x-ray, was diagnosed with pleurisy in April, 2007.[49]
- Edmund Husserl, a German philosopher who established the school of phenomenology died of a form of pleurisy on 27 April 1938.[50]
References
- 1 2 3 4 "What Are Pleurisy and Other Pleural Disorders?". NHLBI. 21 September 2011. Retrieved 1 November 2016.
- 1 2 "What Causes Pleurisy and Other Pleural Disorders?". NHLBI. 21 September 2011. Retrieved 1 November 2016.
- 1 2 3 4 5 Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017: 5 Books in 1. Elsevier Health Sciences. p. 981. ISBN 9780323448383.
- 1 2 "How Are Pleurisy and Other Pleural Disorders Treated?". NHLBI. 21 September 2011. Retrieved 1 November 2016.
- 1 2 Disease & Drug Consult: Respiratory Disorders. Lippincott Williams & Wilkins. 2012. p. Pleurisy. ISBN 9781451151947.
- ↑ "What Are the Signs and Symptoms of Pleurisy and Other Pleural Disorders". NHLBI. 21 September 2011. Retrieved 1 November 2016.
- ↑ Kass, SM; Williams, PM; Reamy, BV (1 May 2007). "Pleurisy.". American family physician. 75 (9): 1357–64. PMID 17508531.
- ↑ Light, Richard W.; Lee, Y. C. Gary (2008). Textbook of Pleural Diseases Second Edition (2 ed.). CRC Press. p. 2. ISBN 9780340940174.
- ↑ "The Lung Center: Understanding Pleurisy" (PDF). An online information portal for the community. The Lung Center, New Deli, India. Retrieved 2013-06-22.
- ↑ Beth Walsh, MA. Pleurisy (pleuritis).
- 1 2 Ferri, Fred F. Ferri's Clinical Advisor 2012. Philadelphia, PA: Elsevier Mosby, 2012, P. 790.
- 1 2 3 4 5 Sara M. Kass, CDR, MC, USN, Pamela M. Williams, MAJ, USAF, MC, and Brian V. Reamy, COL, USAF, MC, Uniformed Services University of the Health Sciences, Bethesda, Maryland. Pleurisy. American Family Physician. 2007, 1 May; 75(9):1357-1364.PDF
- ↑ Maskell, Nick, and Ann Millar. Oxford Desk Reference. Oxford: Oxford University Press, 2009. Chapter 14. Pleural Disease. PDF
- ↑ Raed A. Dweik. Cleveland Clinic Center for Continuous Education: Pleural Disease.
- ↑ Light, R.W. Diagnostic principles in pleural disease. European Respiratory Journal, 1997 Feb; 10(2): 476-81.PDF
- ↑ Sahn, Steven A. Pleural Disease. Philadelphia: Saunders, 2006.
- ↑ Klein RC (October 1984). "Effects of indomethacin on pleural pain". South. Med. J. 77 (10): 1253–4. PMID 6207594. doi:10.1097/00007611-198410000-00011.
- ↑ Fishman, Alfred P., and Jack A. Elias. Fishman's Pulmonary Diseases and Disorders. New York: McGraw-Hill, Health Professions Division, 1997.
- ↑ Peters RR, Saleh TF, Lora M, et al. (1999). "Anti-inflammatory effects of the products from Wilbrandia ebracteata on carrageenan-induced pleurisy in mice". Life Sci. 64 (26): 2429–37. PMID 10403502. doi:10.1016/S0024-3205(99)00200-3.
- 1 2 Siqueira JM, Peters RR, Gazola AC, et al. (March 2007). "Anti-inflammatory effects of a triterpenoid isolated from Wilbrandia ebracteata Cogn". Life Sci. 80 (15): 1382–7. PMID 17286991. doi:10.1016/j.lfs.2006.12.021.
- ↑ "Plutarch, Life of Marius".
- ↑ Livermore, Harold (2006). The twilight of the Goths : the rise and fall of the kingdom of Toledo c.575-711. Bristol, United Kingdom: Intellect. p. 36. ISBN 978-1-84150-966-2.
- ↑ Einhard, The Life Of Charlemagne (University of Michigan Press, 5th edition, 1964) at p. 59
- ↑ Frieda, Leonie. Catherine De Medici: Renaissance Queen of France. New York: Fourth Estate, 2003, p. 381.
- ↑ Isaacson, Walter (2003). Benjamin Franklin : an American life. New York: Simon & Schuster.
- ↑ (Spanish) "Juan O'Donojú," Enciclopedia de México, v. 10. Mexico City, 1987.
- ↑ Jason, Philip K.; Graves, Mark A. (2001). Encyclopedia of American war literature. Westport, Conn.: Greenwood Press. p. 197.
- ↑ Gill, Stephen (1989). William Wordsworth: a Life. Oxford, England: Clarendon Press. ISBN 978-0-19-812828-1.
- ↑ Michele Molineris. Nuova vita di Domenico Savio. Castelnuovo Don Bosco, 1974, pp. 268-270.
- ↑ Emerson, Jason. Giant in the Shadows: The Life of Robert T. Lincoln. Carbondale: Southern Illinois University Press, 2012, P. 478.
- ↑ "Pleurisy: Devil Anse Hatfield's Illness On Haftields & McCoys". Huffingtonpost.com. 2012-05-31. Retrieved 2013-03-12.
- ↑ https://archive.org/details/FrankC.Stanley-31-40
- ↑ Gandhi, Rajmohan (2006). Gandhi: the man, his people, and the empire. Berkeley, California: University of California Press. p. 174. ISBN 978-0-520-25570-8.
- ↑ "Times topics". The New York Times. 1920–1921. Retrieved 2013-06-23.
- ↑ Caruso, E., & Farkas, A. (1990). Enrico Caruso: My father and my family. Portland, Or: Amadeus Press, pp. 328-334.
- ↑ "Eli Bowen: The Legless Acrobat". Thehumanmarvels.com. Retrieved 2013-03-12.
- ↑ Templier, Pierre-Daniel, Erik Satie. Translated by Elena L. French and David S. French. Cambridge: MA Institute of Technology, 1969. 51-53.
- ↑ Brunskill, Ian. The Times Great Lives: A Century in Obituaries. London: Times Books, 2005.
- ↑ The Pennsylvania Gazette: Weekly Magazine of the University of Pennsylvania. 26 (7). 1927. Missing or empty
|title=(help) - ↑ "Famous People: Poets: Thomas Hardy Biography". Thefamouspeople.com. Retrieved 2013-06-17.
- ↑ "Anna Pavlova Dies at Height of Fame". The New York Times. 23 January 1931. Retrieved 2013-06-23.
- ↑ "Florenz Ziegfeld Dies in Hollywood After Long Illness". The New York Times. 23 July 1932. Retrieved 2013-06-30.
- ↑ Kodansha Encyclopedia of Japan. Volume 6. Tokyo: Kodansha, 1983.
- ↑ Nino Manfredi, Antonio Cocchia. Nudo d'attore. Mondadori, 1993. ISBN 8804332077.
- ↑ Lindsay, David (2000). House of invention : the secret life of everyday products. New York, N.Y.: Lyons Press. pp. 20–21.
- ↑ Carr, Virginia Spencer. The Lonely Hunter: A Biography of Carson McCullers. Athens, Ga.: Univ. of Georgia Press, 2003, p. 573.
- ↑ Myers, F.W.H. (2006). Wordsworth. BiblioBazaar, LLC. p. 177. ISBN 1-4264-3226-7.
- ↑ "James out of hospital after treatment for pleurisy". sports.espn.go.com. 14 October 2005. Retrieved 30 June 2013.
- ↑ "Griffey is limited by pleurisy". Los Angeles Times. 28 April 2007. Retrieved 2013-06-18.
- ↑ Smith, A. D. (2003). Husserl and the Cartesian Meditations. New York: Routledge. p. xii. ISBN 020342266X.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
- Tim Kenny; Colin Tidy (2002–2013). "Pleurisy and Pleuritic Pain". www.patient.info. Retrieved 2013-06-30.
- The Lung Association of Canada explanation of Pleurisy (also available in French)
- Pleurisy by the American Academy of Family Physicians