Assisted suicide
| Suicide |
|---|
 |
|
Related phenomena |
Assisted suicide is suicide committed with the aid of another person, sometimes a physician.[1] The term is often used interchangeably with physician-assisted suicide (PAS), which involves a doctor "knowingly and intentionally providing a person with the knowledge or means or both required to commit suicide, including counseling about lethal doses of drugs, prescribing such lethal doses or supplying the drugs."[2]
Canada, Belgium, the Netherlands, Luxembourg, and Switzerland allow physicians to physically assist in the death of patients. The United States has authorized medical aid in dying in six states, which refers to a terminally ill person with 6 months or less to live taking a medication prescribed by a doctor; this is legally distinguished from physician assisted suicide per the individual state laws. Assisted suicide is prohibited by common law or criminal statute in all U.S.
Physician-assisted suicide is often confused with euthanasia. In cases of euthanasia the physician administers the means of death, usually a lethal drug. In physician-assisted suicide (PAS), it is required that the person voluntarily expresses his or her wish to die, and also makes a request for medication for the purpose of ending his or her life. Physician-assisted suicide thus involves a person’s self-administration of deadly drugs that are supplied by a doctor.[3]
Support
Personal autonomy
Medical decisions are personal and should be made by individuals and their families while respecting the federal and state laws. Libertarians strongly support medical aid in dying legislation for this reason.
Reducing suffering
One argument for medical aid in dying is that it reduces prolonged suffering in those with terminal illnesses. When death is imminent (6 months or less) patients can choose to have aid in dying as a medical option to shorten an unbearable dying process. The three most frequently mentioned end‐of‐life concerns reported by Oregon residents who took advantage of the Death With Dignity Act in 2015 were: decreasing ability to participate in activities that made life enjoyable (96.2%), loss of autonomy (92.4%), and loss of dignity (75.4%).[4]
Washington vs. Glucksberg
Assisted suicide is a very controversial topic, In Washington, it did not become legal until 2008.[5] In 1997, four Washington physicians, and three deathly ill patients brought forth a lawsuit that would challenge the ban on medical aid in dying that was in place at the time. This lawsuit was first part of a district court hearing, where it ruled in favor of Glucksberg,[6] which was the group of physicians and terminally ill patients. The lawsuit was then affirmed by the Ninth Circuit.[7] Thus, it was taken to the Supreme Court, and there the Supreme Court decided to grant Washington certiorari. Eventually, the Supreme Court decided, with a unanimous vote, that medical aid in dying was not a protected right under the constitution as of the time of this case.[8] The laws and arguments on this topic are often argued and changed depending on legal evaluation and decision.
Oregon Statistics
A study of hospice nurses and social workers in Oregon reported that symptoms of pain, depression, anxiety, extreme air hunger and fear of the process of dying were more pronounced among hospice patients who did not request aid-in-dying medication.[9]
A Journal of Palliative Medicine report on patterns of hospice use noted that Oregon was in both the highest quartile of hospice use and the lowest quartile of potentially concerning patterns of hospice use. A similar trend was found in Vermont, where AiD was authorized in 2013.[10]
In Oregon, in hospital death rates are at the lowest in the nation, at home death rates are at the highest in the nation, and violent suicide among hospice patients has been reduced significantly.[10]
In February 2016, Oregon released a report on their 2015 numbers. During 2015, there were 218 people in the state who were approved and received the lethal prescription medicines to end their own life. Of that 218, 132 terminally ill patients ultimately made the decision to ingest the medication, resulting in their death. According to the state of Oregon Public Health Division’s survey, the majority of the participants, 78%, where 65 years of age or older and predominately Caucasian, 93.1%. 72% of the terminally ill patients who opted for ending their own lives had been diagnosed with some form of cancer. In the state of Oregon’s 2015 survey, they asked the terminally ill who were participating in medical aid in dying, what their biggest end-of-life concerns were: 96.2 percent of those people mentioned the loss of the ability to participate in activities that once made them enjoy life, 92.4 percent mentioned the loss of autonomy, or their independence of their own thoughts or actions, and 75.4 percent stated loss of their dignity (Oregon Death With Dignity Act).
Washington State Statistics
An increasing trend in deaths caused from ingesting lethal doses of medications prescribed by physicians was also noted in Washington: from 64 deaths in 2009 to 202 deaths in 2015.[11] Among the deceased, 72% had terminal cancer and 8% had neurodegenerative diseases (including ALS).[11]
U.S. Polls
A poll conducted by National Journal and Regence Foundation found that both Oregonians and Washingtonians were more familiar with the terminology "end-of-life care" than the rest of the country and residents of both states are slightly more aware of the terms palliative and hospice care.[12]
A survey from the Journal of Palliative Medicine found that family caregivers of patients who chose medical AiD were more likely to find positive meaning in caring for a patient and were more prepared for accepting a patient's death than the family caregivers of patients who didn’t request AiD.[13]
Safeguards to protect vulnerable populations
Many current aid in dying laws contain oversight and investigative processes to ensure that the law is used only in eligible scenarios and within the confines of the law.
This includes stringent eligibility and qualification processes, mandatory state reporting by the medical team, and medical board oversight. In Oregon and other states, two doctors and two witnesses must attest that a person's request for aid in dying medication wasn’t coerced or under undue influence.
These safeguards include proving your residency and eligibility. You must meet with two physicians and they must confirm your diagnoses before you can continue, in some cases, they do include a psychiatric evaluation as well to determine whether or not the patient is making this decision on his/her own. The next steps are two oral requests, a waiting period of a minimum of 15 days before making your next request. A written request which must be witnessed by two different people, one of which cannot be a family member, and then another waiting period by your doctor in which they either say you're eligible for the drugs or not ("Death with Dignity").
"Slippery slope" fears not realized
The state of Oregon provides nearly two decades of data on their Death with Dignity Act.
An October 2007 study, published in the Journal of Medical Ethics, found that "rates of assisted dying in Oregon and in the Netherlands showed no evidence of heightened risk for the elderly, women, the uninsured (inapplicable in the Netherlands, where all are insured), people with low educational status, the poor, the physically disabled or chronically ill, minors, people with psychiatric illnesses including depression, or racial or ethnic minorities, compared with background populations. The only group with a heightened risk was people with AIDS."[14]
Support organizations
Listed below are some major organizations that support medical aid in dying:
Death with Dignity National Center
The Death with Dignity National Center is a nonprofit organization that has been in existence since 1993. This organization is most notably associated with the original writing and continued advocating of the Oregon Death with Dignity Law that was enacted on October 27, 1997.[15] Oregon, Washington, and Vermont laws state that mentally competent, and terminally ill adult patients can determine if they want to receive prescription medication so they can die in a humane and peaceful way.[16]
Dignitas (Switzerland)
Dignitas helps Swiss nationals and foreigners to die by providing advice and lethal drugs. The legal pre-requisites are that a person must have either a terminal illness, an unendurable incapacitating disability or unbearable and uncontrollable pain.[17] However, in practice they also accept mentally ill patients[18] or those without a medical diagnosis. 25% of people in Switzerland who take advantage of assisted suicide do not have a terminal illness but are "tired of life",[19] for example the retired British art teacher who killed herself on 27 March 2014 "in part because she had become fed up with the modern world of emails, TVs, computers and supermarket ready meals."[20]
Dignity in Dying
Dignity in Dying is a voluntary[21] located in London.[22]
Disabled Activists for Dignity in Dying
DADID[23] is a campaign group in the UK for disabled people in association with Dignity in Dying, led by disabled people who support a change in the law to allow terminally ill, mentally competent adults the choice of an assisted death within upfront safeguards. Disability is an issue claimed both by activists and opponents in support of their arguments. Most court cases appealing for medical aid in dying have been brought by disabled persons. A Yougov poll[24] in the U.K. suggested that 80% of disabled persons support a change in the law, such as Lord Falconer's Bill[25] to allow some form of medical aid in dying.
Exit
Exit is a Scottish organization that supports a permissive model of right-to-die legislation[26] based on published research and recommendations from Glasgow University using an 'exceptions to the rule' (against euthanasia) format to facilitate transparency and open safeguards.[27] Exit published the world's first guide on medical aid in dying, called How to Die With Dignity (1980); followed by Departing Drugs (1993), and the Five Last Acts series.[28][29] Exit also publishes a Blog with broad-ranging analysis of assisted-suicide related issues.[30]
Exit International
Exit International is the publisher of the assisted dying guidebook The Peaceful Pill Handbook by Dr. Philip Nitschke and Dr. Fiona Stewart.[31] Founded in 2006 by Nitschke and based in Bellingham, Washington,[32] Exit International is a pro-choice assisted dying organization with an online membership of around 18,000 internationally. The organization holds meetings and workshops in the US, Canada, the UK and Ireland, Australia and New Zealand.
Final Exit Network
Final Exit Network, Inc. is a nonprofit organization founded in 2004 for the purpose of serving as a resource to individuals seeking information and emotional support in dying medically as a means to end suffering from chronically painful—though not necessarily terminal—illness.
World Federation of Right to Die Societies
The World Federation of Right to Die Societies was founded in 1980 and encompasses thirty-eight right to die organizations in twenty-three different countries.[33]
Opposition
Medical ethics
Hippocratic Oath
Some doctors[34] remind that physician-assisted suicide is contrary to the Hippocratic Oath of 400 B.C.E., which is the oath historically taken by physicians. It states "I will give no deadly medicine to anyone if asked, nor suggest any such counsel".[35][36] The original oath however has been modified many times and, contrary to popular belief, is not required by most modern medical schools.[37]
The Declaration of Geneva
The Declaration of Geneva is a revision of the Hippocratic Oath, first drafted in 1948 by the World Medical Association in response to forced euthanasia, eugenics and other medical crimes performed in Nazi Germany. It contains, "I will maintain the utmost respect for human life."
The International Code of Medical Ethics
The International Code of Medical Ethics, last revised in 2006, includes "A physician shall always bear in mind the obligation to respect human life" in the section "Duties of physicians to patients".[38]
The Statement of Marbella
The Statement of Marbella was adopted by the 44th World Medical Assembly in Marbella, Spain, in 1992. It provides that "physician-assisted suicide, like euthanasia, is unethical and must be condemned by the medical profession."[39]
"Slippery slope" argument
There are many health care professionals, especially those concerned with bioethics, who are opposed to PAS due to the detrimental effects that the procedure can have with regard to vulnerable populations. This argument is known as the "slippery slope".[40] This argument encompasses the apprehension that once PAS is initiated for the terminally ill it will progress to other vulnerable communities, namely the disabled, and may begin to be used by those who feel less worthy based on their demographic or socioeconomic status. In addition, vulnerable populations are more at risk of untimely deaths because, "patients might be subjected to PAS without their genuine consent".[41]
Religious stances
Buddhism
According to Buddhist thought, assisted suicide and euthanasia constitute deliberate killing of another person. These practices contradict the fundamental Buddhist principle of refraining from killing a living being. Suicide is considered an uncompassionate act as it causes grief to others and is believed to deprive them of spiritual development. Buddhism also says that assisted suicide is uncompassionate because death will not relieve the killed person of suffering, and is instead thought to postpone the suffering to their next life. The perpetrator is also believed to experience negative karma and suffering in the next life, as killing another person, no matter the reason, is seen as a negative act.
Catholicism
The Roman Catholic Church acknowledges the fact that moral decisions regarding a person's life must be made according to one's own conscience and faith.[42] Catholic tradition has said that one's concern for the suffering of another is not a sufficient reason to decide whether it is appropriate to act upon euthanasia. According to the Catechism of the Catholic Church, "God is the creator and author of all life." In this belief system God created human life, therefore God is the judge when to end life.[42] From the Roman Catholic Church’s perspective, deliberately ending one’s life or the life of another is morally wrong and defies the Catholic doctrine. Furthermore, ending one’s life deprives that person and his or her loved ones of the time left in life and causes enormous grief and sorrow for those left behind.[43]
Pope Francis[44] is the current dominant figure of the Catholic Church. He affirms that death is a glorious event and should not be decided for by anyone other than God. Pope Francis insinuates that defending life means defending its sacredness.[45] The Roman Catholic Church teaches its followers that the act of euthanasia is unacceptable because it is perceived as a sin, as it goes against the Ten Commandments, "you shall not kill." As implied by the fifth commandment, the act of assisted suicide contradicts the dignity of human life as well as the respect one has for God.[46]
The Roman Catholic Church also recognizes the story of the Good Samaritan. It uses the story to call earnestly upon the Good Samaritan's actions and his love for his neighbor. In this tradition, the act of assisted suicide negates the respect and love we should have for our neighbors, as it mistakenly places the love God has for his followers in the hands of physicians.
As an alternative to the Physician-Assisted Suicide and in order to alleviate pain, the Catholic Church proposes that terminally ill patients focus on religion and making peace with the Creator while receiving the love and mercy of their families and caregivers.[47] Additionally, the Roman Catholic Church recommends that terminally ill patients should receive palliative care, which deals with physical pain while treating psychological and spiritual suffering as well, instead of Physician-Assisted Suicide.[48]
Judaism
While preservation of life is one of the greatest values in Judaism, there are rare instances of suicide and assisted suicide appearing in the Bible and Rabbinic literature.[49] The medieval authorities debate the legitimacy of those measures and in what limited circumstances they might apply. The conclusion of the majority of later rabbinic authorities, and accepted normative practice within Judaism, is that suicide and assisted suicide can not be sanctioned even for a terminal patient in intractable pain.[50]
Unitarianism
According to a 1988 General Resolution, "Unitarian Universalists advocate the right to self-determination in dying, and the release from civil or criminal penalties of those who, under proper safeguards, act to honor the right of terminally ill patients to select the time of their own deaths".[51]
Mormonism
The Church of Jesus Christ of Latter-day Saints is against euthanasia. Anyone who takes part in euthanasia, including "assisted suicide", is regarded as having violated the commandments of God.[52] However the Church recognizes that when a person is in the final stages of terminal illness there may be difficult decisions to be taken. The Church states that 'When dying becomes inevitable, death should be looked upon as a blessing and a purposeful part of an eternal existence. Members should not feel obligated to extend mortal life by means that are unreasonable.[53]
Organizations opposed to assisted suicide
- ADAPT – the American Disabled for Attendant Programs Today is a United States organisation that is active in the disability rights movement. They oppose the legalization of physician-assisted suicide, arguing that it is a "violation of the equal protection guaranteed by the Americans with Disabilities Act."[54]
- Agudath Israel of America[55]
- Autistic Self Advocacy Network
- British Medical Association
- Care Not Killing is a group based in the United Kingdom that combines a number of organisations opposed to assisted suicide under a common banner.[56]
- Christian Medical Fellowship
- Disability Rights Education and Defense Fund[57]
- The Euthanasia Prevention Coalition International, founded in 1998 in Canada, is an international organisation opposed to euthanasia and assisted suicide.
- Family First New Zealand[58]
- Family Institute of Connecticut[59]
- National Council on Disability
- National Spinal Cord Injury Association
- Not Dead Yet is a United States disability rights group that opposes assisted suicide and euthanasia for people with disabilities.[60]
- Orthodox Union is one of the oldest Orthodox Jewish organizations in the United States[61]
- Patients' Rights Action Fund
- Royal College of General Practitioners
- Royal College of Physicians[62]
- TASH is an international advocacy association of people with disabilities, their family members, other advocates, and people who work in the disability field. The mission of TASH is to promote the full inclusion and participation of children and adults with significant disabilities in every aspect of their community, and to eliminate the social injustices that diminish human rights.
- The Russian Orthodox Church Canons consider any form of suicide, except suicides committed out of mental disturbances (insanity), a grave sin and a human fault: "A perpetrator of calculated suicide, who 'did it out of human resentment or other incident of faintheartedness' shall not be granted Christian burial or liturgical commemoration (Timothy of Alexandria, Canon 14).[63]
- The United States Conference of Catholic Bishops has stated its opposition to assisted suicide.[64]
- Voice for Life[65]
- The World Medical Association's official position is: "Physicians-assisted suicide, like euthanasia, is unethical and must be condemned by the medical profession. Where the assistance of the physician is intentionally and deliberately directed at enabling an individual to end his or her own life, the physician acts unethically. However the right to decline medical treatment is a basic right of the patient and the physician does not act unethically even if respecting such a wish results in the death of the patient."[66]
Attitudes of physicians and healthcare professionals
It is widely acknowledged that physicians must play some role in the process of assisted suicide and euthanasia (as evident in the name "physician assisted suicide"), often putting them at the forefront of the issue. Just like the general public, physician and other healthcare professional opinions vary on the issue of assisted suicide.
United States
2014 Medscape Survey
The Medscape Ethics Report of 2014 found that 54% of U.S. based doctors surveyed agreed that physician-assisted suicide should be allowed. 31% disagreed. Support for the measure has increased 8 percentage points since 2010.[67]
1994 New England Journal of Medicine study
A study published in 1994 in the New England Journal of Medicine found that physicians’ attitudes toward physician assisted suicide and euthanasia were polarizing. 39% of the 938 participants polled agreed with the statement that physician assisted suicide is never ethically justified, 50% disagreed. 53% said physician assisted suicide should be legal in some cases, and 40% said they would be willing to assist a patient in committing suicide.[68]
United Kingdom
2009 studies
An extensive survey of 3733 medical physicians was sponsored by the National Council for Palliative Care, Age Concern, Help the Hospices, Macmillan Cancer Support, the Motor Neurone Disease Association, the MS Society and Sue Ryder Care. It showed that the proportion against a change in the law was 66% against euthanasia and 65% against assisted suicide. Opposition to euthanasia and PAS was highest among Palliative Care and Care of the Elderly specialists, while more than 90% of palliative care specialists were against a change in the law.[69]
Evidence shows that physicians already perform euthanasia and assisted suicide in the UK. In a 2009 survey of 8857 physicians, the proportion of UK deaths involving voluntary euthanasia (i.e. at the patient's request) was 0.21% (CI: 0–0.52), and involuntary euthanasia (i.e. without the patient's request) was 0.30% (0–0.60).[70]
1997 Glasgow University Study
Glasgow University's Institute of Law & Ethics in Medicine surveyed UK medical practitioners and pharmacists and found that 54% were in favour of a change in the law to allow physician-assisted suicide to take place in specific circumstances, with only 36% against. 60% of the 1000 practitioners who responded had treated a patient who was considering suicide, 12% personally knew another health professional who had assisted a patient to kill themselves and 4% had themselves provided the means (such as drugs or information about lethal acts) to assist a patient to kill themselves. One finding of the second study was that most medical practitioners found physician-assisted suicide preferable to voluntary euthanasia (43% in comparison to 19%), especially in view of the findings of a first study by the University which showed the public's preference for voluntary euthanasia. There was little by way of differences in the percentages of hospital physicians, medical GPs, surgeons or psychiatrists favouring a change in the law – approximately 48% were in favour. This was in stark contrast to the percentage of pharmacists in favour (72%) and anaesthetists (56%). Pharmacists were twice as likely as medical GPs to endorse the view that "if a patient has decided to end their own life then doctors should be allowed in law to assist". (McLean, S., 1997, "Sometimes a Small Victory", Institute of Law and Ethics in Medicine, University of Glasgow.)
Legality by country
Voluntary euthanasia was legalized in Colombia (in 1997),[71] the Netherlands (in 2002), Belgium (in 2002), Luxembourg (in 2008),[72] and Canada (in 2016).[73] Assisted suicide, where the patient has to take the final action themselves (unlike voluntary euthanasia), is legal in Canada, the Netherlands, Luxembourg, Switzerland and parts of the United States. In the United States there are assisted dying laws restricted to terminally ill and mentally competent adults in Oregon, Montana, Washington, Vermont, California, Colorado and Washington D.C.[74] Oregon was the first United States state to legalize assisted suicide, which was achieved through popular vote. The Act was a citizens' initiative passed twice by Oregon voters. The first time was in a general election in November 1994 when it passed by a margin of 51% to 49%. An injunction delayed implementation of the Act until it was lifted on October 27, 1997. In November 1997, a measure was placed on the general election ballot to repeal the Act. Voters chose to retain the Act by a margin of 60% to 40%.[75]
Australia
Assisted suicide is currently illegal throughout Australia, but was for a time legal in the Northern Territory under the Rights of the Terminally Ill Act 1995.
Belgium
The "Euthanasia Act" legalized euthanasia in Belgium in 2002,[76][77] but it didn't cover assisted suicide.[78]
In 2006, Belgium partially legalized euthanasia with certain regulations:
- The patient must be an adult and in a "futile medical condition of constant and unbearable physical or mental suffering that cannot be alleviated".[79]
- The patient must have a long-term history with the doctor, with euthanasia/physician assisted suicide only allowed for permanent residents.
- There need to be several requests that are reviewed by a commission and approved by two doctors.[80]
As of November 2015, Belgium had the most liberal assisted suicide laws in the world.[81]
In 2014, Belgium became the first country to authorize euthanasia for children, on request, if they have a terminal illness and understand the repercussions of their act.[82]
Canada
Suicide was considered a criminal offence in Canada until 1972. Physician-assisted suicide has been legal in the Province of Quebec since June 5, 2014.[83] It was declared legal across the country because of the Supreme Court of Canada decision Carter v Canada (AG), of February 6, 2015. After a lengthy delay, the House of Commons passed a Bill (C-14) in mid June 2016 that allows for doctor-assisted suicide.
China
In China, assisted suicide is illegal under Articles 232 and 233 of the Criminal Law of the People's Republic of China.[84]
An article in People's Daily reported that "Nine people from Xi'an City in China made news when they 'jointly wrote to local media asking for euthanasia, or mercy killings'.[84] These people had uremia, a disease due to the failure of the kidneys, and expressed their "unbearable suffering and [an unwillingness] to burden their families any more".[85] In China, suicide or neglect is considered homicide and can be punished by three to seven years in prison.[85] Zhong’s case rejected the legality of assisted suicide.
Colombia
In May 1997 the Colombian Constitutional Court allowed for the euthanasia of sick patients who requested to end their lives, by passing Article 326 of the 1980 Penal Code.[80] This ruling owes its success to the efforts of a group that strongly opposed euthanasia. When one of its members brought a lawsuit to the Colombian Supreme Court against it, the court issued a 6 to 3 decision that "spelled out the rights of a terminally ill person to engage in voluntary euthanasia."[86]
In February 2015, the Supreme Court gave the government 30 days to create a comprehensive set of guidelines for doctors, to assist them in avoiding breaches of the law, as although technically legal, many physicians face lawsuits where they must prove that all legal requirements were met prior to the procedure. This fear of legal action has led many doctors to refuse to perform the procedure, in spite of its legality.[87]
Denmark
In Denmark, passive euthanasia, or the refusal to accept treatment is not illegal. But voluntary euthanasia when a patient actively tries to kill themselves is illegal. 71% of Denmark's population is in favor of legalizing assisted suicide.[88]
France
The controversy over legalising euthanasia and physician assisted suicide is not as big as in the United States because of the country's "well developed hospice care programme".[89] However, in 2000 the controversy over the topic was ignited with Vincent Humbert. After a car crash that left him "unable to 'walk, see, speak, smell or taste'", he used the movement of his right thumb to write a book, I Ask the Right to Die (Je vous demande le droit de mourir) in which he voiced his desire to "die legally".[89] After his appeal was denied, his mother assisted in killing him by injecting him with an overdose of barbiturates that put him into a coma, killing him 2 days later. Though his mother was arrested for aiding in her son's death and later acquitted, the case did jump-start new legislation which states that when medicine serves "no other purpose than the artificial support of life" it can be "suspended or not undertaken".[90]
In 2013 President Francois Hollande said that France should hold a national debate on the issue, and stated his intention to introduce a bill to parliament before the end of the year. Opinion polls in France show that the majority of the public are in favor of an assisted suicide law,[91] however France's national ethics committee has advised against any change in the law.[92]
Germany
Killing somebody in accordance with his demands is always illegal under the German criminal code (Paragraph 216, "Killing at the request of the victim; mercy killing").[93]
Assisting with suicide by, for example, providing poison or a weapon, is generally legal. Since suicide itself is legal, assistance or encouragement is not punishable by the usual legal mechanisms dealing with complicity and incitement (German criminal law follows the idea of "accessories of complicity" which states that "the motives of a person who incites another person to commit suicide, or who assists in its commission, are irrelevant").[94] Nor is assisting with suicide explicitly outlawed by the criminal code. There can however be legal repercussions under certain conditions for a number of reasons. Aside from laws regulating firearms, the trade and handling of controlled substances and the like (e.g. when acquiring poison for the suicidal person), this concerns three points:
Free vs. manipulated will
If the suicidal person is not acting out of his own free will, then assistance is punishable by any of a number of homicide offences that the criminal code provides for, as having "acted through another person" (§25, section 1 of the German criminal code,[95] usually called "mittelbare Täterschaft"). Action out of free will is not ruled out by the decision to end one's life in itself; it can be assumed as long as a suicidal person "decides on his own fate up to the end [...] and is in control of the situation."[94]
Free will cannot be assumed, however, if someone is manipulated or deceived. A classic textbook example for this, in German law, is the so-called Sirius case on which the Federal Court of Justice ruled in 1983: The accused had convinced an acquaintance that she would be re-incarnated into a better life if she killed herself. She unsuccessfully attempted suicide, leading the accused to be charged with, and eventually convicted of attempted murder.[96] (The accused had also convinced the acquaintance that he hailed from the star Sirius, hence the name of the case).
Apart from manipulation, the criminal code states three conditions under which a person is not acting under his own free will:
- if the person is under 14
- if the person has "one of the mental diseases listed in §20 of the German Criminal Code"[97]
- a person that is acting under a state of emergency.
Under these circumstances, even if colloquially speaking one might say a person is acting of his own free will, a conviction of murder is possible.
Neglected duty to rescue
German criminal law obliges everybody to come to the rescue of others in an emergency, within certain limits (§323c of the German criminal code, "Omission to effect an easy rescue").[98] This is also known as a duty to rescue in English. Under this rule, the party assisting in the suicide can be convicted if, in finding the suicidal person in a state of unconsciousness, he does not do everything in his power to revive him.[99] In other words, if someone assists a person in committing suicide, leaves, but comes back and finds the person unconscious, he must try to revive him.[100]
This reasoning is disputed by legal scholars, citing that a life-threatening condition that is part, so to speak, of a suicide underway, is not an emergency. For those who would rely on that defence, the Federal Court of Justice has considered it an emergency in the past.
Homicide by omission
German law puts certain people in the position of a warrantor (Garantenstellung) for the well-being of another, e.g. parents, spouses, doctors and police officers. Such people might find themselves legally bound to do what they can to prevent a suicide; if they do not, they are guilty of homicide by omission.
Iceland
Assisted suicide is illegal. "At the current time, there are no initiatives in Iceland that seek the legalization of euthanasia or assisted suicide. The discussion on euthanasia has never received any interest in Iceland, and both lay people and health care professionals seem to have little interest in the topic. A few articles have appeared in newspapers but gained little attention."[101]
Luxembourg
In March 2003, a vote to legalise assisted suicide was lost by a single vote (at the time, assisted suicide was not illegal, as suicide was permitted under the criminal code, but a person assisting someone to take their own life could face prosecution).[102] After again failing to get royal assent for legalizing euthanasia and assisted suicide, in December 2008 Luxembourg's parliament amended the country's constitution to take this power away from the monarch, the Grand Duke of Luxembourg.[103] Euthanasia and assisted suicide were legalized in the country in April, 2009.[104]
The Netherlands
Physician-assisted suicide is legal under the same conditions as euthanasia. Physician-assisted suicide became allowed under the Act of 2001 which states the specific procedures and requirements needed in order to provide such assistance. Assisted suicide in the Netherlands follows a medical model which means that only doctors of terminally ill patients are allowed to grant a request for an assisted suicide. The Netherlands only allows people over the age of 12 to pursue an assisted suicide when deemed necessary.
New Zealand
Assisted suicide is illegal in New Zealand. Under Section 179 of the Crimes Act 1961, it is illegal to 'aid and abet suicide.'
South Africa
South Africa is struggling with the debate over legalizing euthanasia. Owing to the underdeveloped health care system that pervades the majority of the country, Willem Landman, "a member of the South African Law Commission, at a symposium on euthanasia at the World Congress of Family Doctors" stated that many South African doctors would be willing to perform acts of euthanasia when it became legalized in the country.[105] He feels that because of the lack of doctors in the country, "[legalizing] euthanasia in South Africa would be premature and difficult to put into practice [...]".[105]
On 30 April 2015 the High Court in Pretoria granted Advocate Robin Stransham-Ford an order that would allow a doctor to assist him in taking his own life without the threat of prosecution. On 6 December 2016 the Supreme Court of Appeal overturned the High Court ruling.[106]
Switzerland
Though it is illegal to assist a patient in dying in some circumstances, there are others where there is no offence committed.[107] The relevant provision of the Swiss Criminal Code[108] refers to "a person who, for selfish reasons, incites someone to commit suicide or who assists that person in doing so will, if the suicide was carried out or attempted, be sentenced to a term of imprisonment (Zuchthaus) of up to 5 years or a term of imprisonment (Gefängnis)."
A person brought to court on a charge could presumably avoid conviction by proving that they were "motivated by the good intentions of bringing about a requested death for the purposes of relieving "suffering" rather than for "selfish" reasons.[109] In order to avoid conviction, the person has to prove that the deceased knew what he or she was doing, had capacity to make the decision, and had made an "earnest" request, meaning he/she asked for death several times. The person helping also has to avoid actually doing the act that leads to death, lest they be convicted under Article 114: Killing on request (Tötung auf Verlangen) - A person who, for decent reasons, especially compassion, kills a person on the basis of his or her serious and insistent request, will be sentenced to a term of imprisonment (Gefängnis). For instance, it should be the suicide subject who actually presses the syringe or takes the pill, after the helper had prepared the setup.[110] This way the country can criminalise certain controversial acts, which many of its people would oppose, while legalising a narrow range of assistive acts for some of those seeking help to end their lives.
In July 2009, British conductor Sir Edward Downes and his wife Joan died together at a suicide clinic outside Zürich "under circumstances of their own choosing". Sir Edward was not terminally ill, but his wife was diagnosed with rapidly developing cancer.[111]
In March 2010, the PBS FRONTLINE TV program in the United States showed a documentary called "The Suicide Tourist" which told the story of Professor Craig Ewert, his family, and Dignitas, and their decision to commit assisted suicide using sodium pentobarbital in Switzerland after he was diagnosed and suffering with ALS (Lou Gehrig's disease).[112]
In May 2011, Zurich held a referendum that asked voters whether (i) assisted suicide should be prohibited outright; and (ii) whether Dignitas and other assisted suicide providers should not admit overseas users. Zurich voters heavily rejected both bans, despite anti-euthanasia lobbying from two Swiss social conservative political parties, the Evangelical People's Party of Switzerland and Federal Democratic Union. The outright ban proposal was rejected by eighty four percent of voters, while seventy eight percent voted to keep services open should overseas users require them.[113]
In June 2011, The BBC televised the assisted suicide of Peter Smedley, a canning factory owner, who was suffering from motor neurone disease. The programme – Sir Terry Pratchett's Choosing To Die – told the story of Peter's journey to the end where he used The Dignitas Clinic, a euthanasia clinic in Switzerland, to assist him in carrying out the taking of his own life. The programme shows Peter eating chocolates to counter the unpalatable taste of the liquid he drinks to end his own life. Moments after drinking the liquid, Peter begged for water, gasped for breath and became red, he then fell into a deep sleep where he snored heavily while holding his wife's hand. Minutes later, Peter stopped breathing and his heart stopped beating.
In Switzerland non-physician assisted suicide is legal, the assistance mostly being provided by volunteers, whereas in Belgium and the Netherlands, a physician must be present. In Switzerland, the doctors are primarily there to assess the patient's decision capacity and prescribe the lethal drugs. Additionally, unlike cases in the United States, a person is not required to have a terminal illness but only the capacity to make decisions. Interestingly, 25% of people in Switzerland who take advantage of assisted suicide do not have a terminal illness but are simply old or "tired of life."[19]
Uruguay
Assisted suicide, while criminal, does not appear to have caused any convictions, as article 37 of the Penal Code (effective 1934) states: "The judges are authorized to forego punishment of a person whose previous life has been honorable where he commits a homicide motivated by compassion, induced by repeated requests of the victim."[114]
United Kingdom
England and Wales, Northern Ireland
Deliberately assisting a suicide is illegal.[115] Between 2003 and 2006 Lord Joffe made four attempts to introduce bills that would have legalised assisted suicide in England & Wales—all were rejected by the UK Parliament.[116] In the meantime the Director of Public Prosecutions has clarified the criteria under which an individual will be prosecuted in England and Wales for assisting in another person's suicide.[117] These have not been tested by an appellate court as yet[118] In 2014 Lord Falconer of Thoroton tabled an Assisted Dying Bill in the House of Lords which passed its Second Reading but ran out of time before the General Election. During its passage peers voted down two amendments which were proposed by opponents of the Bill. In 2015 Labour MP Rob Marris introduced another Bill, based on the Falconer proposals, in the House of Commons. The Second Reading was the first time the House was able to vote on the issue since 1997. A Populus poll had found that 82% of the British public agreed with the proposals of Lord Falconer's Assisted Dying Bill.[119] However, in a free vote on 11 September 2015, only 118 MPs were in favour and 330 against, thus defeating the bill.[120]
Scotland
Unlike the other jurisdictions in the United Kingdom, suicide was not illegal in Scotland before 1961 (and still is not) thus no associated offences were created in imitation. Depending on the actual nature of any assistance given to a suicide, the offences of murder or culpable homicide might be committed or there might be no offence at all; the nearest modern prosecutions bearing comparison might be those where a culpable homicide conviction has been obtained when drug addicts have died unintentionally after being given "hands on" non-medical assistance with an injection. Modern law regarding the assistance of someone who intends to die has a lack of certainty as well as a lack of relevant case law; this has led to attempts to introduce statutes providing more certainty.
Independent MSP Margo MacDonald's "End of Life Assistance Bill" was brought before the Scottish Parliament to permit assisted suicide in January 2010. The Catholic Church and the Church of Scotland, the largest denomination in Scotland, opposed the bill. The bill was rejected by a vote of 85–16 (with 2 abstentions) in December 2010.[121][122]
The Assisted Suicide (Scotland) Bill was introduced on 13 November 2013 by the late Margo MacDonald MSP and was taken up by Patrick Harvie MSP on Ms MacDonald's death. The Bill entered the main committee scrutiny stage in January 2015 and reached a vote in Parliament several months later; however the bill was again rejected.
United States
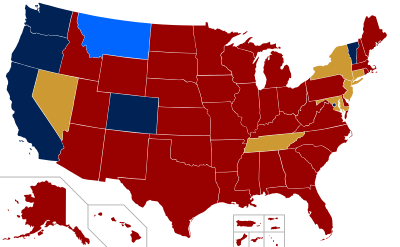
2 Legislation regarding assisted suicide currently under consideration, or a notable court case on the issue is in progress.
Medical aid-in-dying is legal in the American states of California (via the California End of Life Option Act),[123] Oregon (via the Oregon Death with Dignity Act),[124] Washington (Washington Death with Dignity Act), and Vermont (Patient Choice and Control at End of Life Act). In Montana (through the 2009 trial court ruling Baxter v. Montana), the court found no public policy against assisting suicide, so consent may be raised as a defense at trial. Oregon and Washington specify some restrictions. It was briefly legal in New Mexico from 2014, but this verdict was overturned in 2015.
Oregon requires a physician to prescribe medication but it must be self-administered. For the patient to be eligible, the patient must be diagnosed by an attending physician as well as by a consulting physician, with a terminal illness that will cause the death of the individual within 6 months. The law states that, in order to participate, a patient must be: 1) 18 years of age or older, 2) a resident of Oregon, 3) capable of making and communicating health care decisions for him/herself, and 4) diagnosed with a terminal illness that will lead to death within six months. It is up to the attending physician to determine whether these criteria have been met.[75] It is required the patient orally request the medication at least twice and contribute at least one (1) written request. The physician must notify the patient of alternatives; such as palliative care, hospice and pain management. Lastly the physician is to request but not require the patient to notify their next of kin that they are requesting a prescription for a lethal dose of medication. Assuming all guidelines are met and the patient is deemed competent and completely sure they wish to end their life, the physician will prescribe the medication.[125]
The law was passed in 1997. As of 2013, a total of 1,173 people had had DWDA prescriptions written and 752 patients had died from ingesting medications prescribed under the DWDA.[126] In 2013, there were approximately 22 assisted deaths per 10,000 total deaths in Oregon.[126]
Washington's rules and restrictions are similar, if not exactly the same, as Oregon's. Not only does the patient have to meet the above criteria, they also have to be examined by not one, but two doctors licensed in their state of residence. Both doctors must come to the same conclusion about the patient's prognosis. If one doctor does not see the patient fit for the prescription, then the patient must undergo psychological inspection to tell whether or not the patient is in fact capable and mentally fit to make the decision of assisted death or not.[125]
In May 2013, Vermont became the fourth state in the union to legalize medical aid-in-dying. Vermont's House of Representatives voted 75–65 to approve the bill, Patient Choice and Control at End of Life Act. This bill states that the qualifying patient must be at least 18, a Vermont resident and suffering from an incurable and irreversible disease, with less than six months to live. Also, two physicians, including the prescribing doctor must make the medical determination.[127]
In January 2014, New Mexico inched closer to being the fifth state in the United States to legalize medical aid-in-dying via a court ruling.[128] "This court cannot envision a right more fundamental, more private or more integral to the liberty, safety and happiness of a New Mexican than the right of a competent, terminally ill patient to choose aid in dying," wrote Judge Nan G. Nash of the Second District Court in Albuquerque. The NM attorney general's office said it was studying the decision and whether to appeal to the State Supreme Court. However, this was overturned on August 11, 2015 by the New Mexico Court of Appeals, in a 2-1 ruling, that overturned the Bernalillo County District Court Ruling. The Court gave the verdict: "We conclude that aid in dying is not a fundamental liberty interest under the New Mexico Constitution".[129]
In November 2016, the citizens of Colorado approved Proposition 106, the Colorado End of Life Options Act, with 65% in favor. This made it the third state to legalize medical aid-in-dying by a vote of the people, raising the total to six states.
Brittany Maynard
A pivotal case in the United States was the death of Brittany Maynard in 2014. After being diagnosed with terminal brain cancer, the 29 year old decided that instead of suffering with the side effects the cancer would bring, she wanted to die a painless death and live her last days without suffering. She was residing in California when she was diagnosed, where the Death with Dignity was not legal. She and her husband, Dan, moved up to Oregon where Death with Dignity was legal, so she could take advantage of the program. Before her death, she started the Brittany Maynard fund, which works to improve and expand the choice of ending one's life in cases of a terminal illness. In her final days she put a lot of work into the Brittany Maynard fund and Compassion and Choices, and her dying wish was to have her family continue to try and get the Dying with Dignity act passed in all fifty states.[130]
Published research
A study approved by the Dutch Ministry of Health, the Dutch Ministry of Justice, and the Royal Dutch Medical Association reviewed the efficacy in 111 cases of physician-aided dying (PAD).[131] This showed that 32% of cases had complications. These included 12% with time to death longer than expected (45 min – 14 days), 9% with problems administering the required drugs, 9% with a physical symptom (e.g. nausea, vomiting, myoclonus) and 2% waking from coma. In 18% of cases the doctors provided euthanasia because of problems or failures with PAD.
The Portland (Oregon) Veterans Affairs Medical Center and the Department of Psychiatry at the Oregon Health and Science University set out to assess the prevalence of depression in 58 patients who had chosen PAD.[132] Of 15 patients who went to receive PAD, three (20%) had a clinical depression. All patients who participated in the study were determined in advance to be mentally competent. The authors conclude that the "...current practice of the (Oregon) Death with Dignity Act may fail to protect some patients whose choices are influenced by depression from receiving a prescription for a lethal drug".
In a Dutch study of patients with severe and persistent symptoms requiring sedation, the researchers found that only 9% of patients received a palliative care consultation prior to being sedated.[133]
Resources for further reading
More research can be found on the website of Living and Dying Well UK, an organization who researches and analyzes evidence surrounding end-of-life issues.[134]
Popular culture
- Films
- Right to Die?
- Hin und weg
- Me Before You
- Million Dollar Baby
- Mar Adentro (The Sea Inside)
- Guzaarish (2010 film)
See also
- Betty and George Coumbias
- Bioethics
- Consensual homicide
- Euthanasia device
- Jack Kevorkian
- Right to Die? (2008 film)
- Brittany Maynard
- Philip Nitschke
- Senicide
- You don't know Jack (2010, film)
Notes
- ↑ Houghton Mifflin Harcourt Publishing Company. "American Heritage Dictionary Entry: assisted suicide". ahdictionary.com.
- ↑ "EUTHANASIA AND ASSISTED SUICIDE (UPDATE 2007)" (PDF). Canadian Medical Association. 2007. Archived from the original (PDF) on December 19, 2011.
- ↑ Materstvedt & Kaasa (2002). "Euthanasia and physician-assisted suicide in Scandinavia Ð with a conceptual suggestion regarding international research in relation to the phenomena". Palliative Medicine. 16: 19 – via ProQuest.
- ↑ "OREGON DEATH WITH DIGNITY ACT: 2015 DATA SUMMARY" (PDF). Oregon.gov. Oregon Health Authority. Retrieved 4 October 2016.
- ↑ Health, Washington State Department of. "Death with Dignity Act :: Washington State Department of Health". www.doh.wa.gov. Retrieved 2016-11-12.
- ↑ "Washington v. Glucksberg | Vacco v. Quill". www.adflegal.org. Retrieved 2016-11-12.
- ↑ "Case Brief: Washington v. Glucksberg, 521 U.S. 702". www.studentjd.com. Retrieved 2016-11-12.
- ↑ linderd. "Washington v Glucksberg". law2.umkc.edu. Retrieved 2016-11-12.
- ↑ Ganzini, L; Harvath, T.A.; Jackson, A. "Experiences of Oregon nurses and social workers with hospice patients who requested assistance with suicide". The New England Journal of Medicine. 347 (8): 585. doi:10.1056/NEJMsa020562.
- 1 2 Wang, S.; Aldridge, M.D.; Gross, C.P.; Canavan, M.; Cherlin, E.; Johnson-Hurzeler, R. (2015). "Geographic Variation of Hospice Use Patterns at the End of Life.". Journal of Palliative Medicine. 18 (9): 778.
- 1 2 Washington State Department of Health
- ↑ "Living Well at the End of Life Poll" (PDF). The National Journal. February 2010. Retrieved 4 October 2016.
- ↑ Ganzini, L; Goy, E.R.; Dobscha, S.R.; Prigerson, H. (2009). "Mental health outcomes of family members of Oregonians who request physician aid in dying". Journal of Pain Symptom Management. 38, 807-815.
- ↑ Battin, M; van der Heide, A; Ganzini, L; van der Wal, G; Onwuteaka-Phillipsen, B.D. (October 2007). "Legal physician-assisted dying in Oregon and the Netherlands: evidence concerning the impact on patients in "vulnerable" groups.". Journal of Medical Ethics ((10) 591-7).
- ↑ http://www.deathwithdignity.org/news/news/willametteweek031908.asp
- ↑ "Learn - Death With Dignity". Death With Dignity. Retrieved 2016-10-28.
- ↑ Karin. "Brochure of DIGNITAS". dignitas.ch.
- ↑ "World Laws on Assisted Suicide - ERGO". finalexit.org.
- 1 2 Andorno, Roberto (2013-07-01). "Nonphysician-Assisted Suicide in Switzerland". Cambridge Quarterly of Healthcare Ethics. 22 (3): 246–253. ISSN 0963-1801. doi:10.1017/S0963180113000054.
- ↑ "Retired British art teacher ends life at Dignitas ‘because she couldn't adapt to modern world'". The Independent.
- ↑ "Home - Dignity in Dying". Dignity in Dying. 2013-03-14.
- ↑ Wotton, Sarah. "About Dignity in Dying." Dignity in Dying: your life, your choice. Dignity in Dying. 3 Apr 2009.
- ↑ "Disabled Activists for Dignity in DyingDisabled Activists for Dignity in Dying - Campaign for Assisted Dying". Disabled Activists for Dignity in Dying.
- ↑ "National Secular Society". National Secular Society.
- ↑ "Assisted Dying Bill [HL] 2014-15". parliament.uk.
- ↑ "Assisted Suicide Act". euthanasia.cc.
- ↑ McLean S., Britton A., "Sometimes a Small Victory", Institute of Law and Ethics in Medicine, University of Glasgow, 1996
- ↑ "Five Last Acts (2nd edition): expanded & revised: Chris Docker: 9781453869376: Amazon.com: Books". amazon.com.
- ↑ "Five Last Acts - The Exit Path: The arts and science of rational suicide in the face of unbearable, unrelievable suffering: Chris Docker: 9781482594096: Amazon.com: Books". amazon.com.
- ↑ "The EXIT euthanasia blog". The EXIT euthanasia blog.
- ↑ "The Last Day of Her Life". New York Times. 2015-05-14. Retrieved 2015-10-04.
- ↑ "Exit International, About Us". Exit International. Retrieved 2015-10-04.
- ↑ "Scottish Parliament installed cross-party committee to investigate legalising assisted suicide". worldrtd.net.
- ↑ Kass, Leon R. (1989). "Neither for love nor money: why doctors must not kill" (PDF). Public Interest. 94: 25–46.
- ↑ "The Internet Classics Archive - The Oath by Hippocrates". mit.edu.
- ↑ "Hippocratic oath". Encyclopædia Britannica.
- ↑ "Greek Medicine - The Hippocratic Oath". nih.gov.
- ↑ "WMA International Code of Medical Ethics". wma.net. 1 October 2006.
- ↑ "WMA Statement on Physician-Assisted Suicide". wma.net. 1 May 2005.
- ↑ Ross Douthat (September 6, 2009). "A More Perfect Death". New York Times.
- ↑ Mayo DJ, Gunderson M (2002). "Vitalism revitalized.... Vulnerable populations, prejudice, and physician-assisted death". Hastings Cent Rep. 32 (4): 14–21. JSTOR 3528084. PMID 12362519. doi:10.2307/3528084.
- 1 2 Donovan, Kevin G. (1997). "Decisions at the End of Life: Catholic Tradition". Christian Bioethics: Non-Ecumenical Studies in Medical Morality. 3: 188–203. doi:10.1093/cb/3.3.188.
- ↑ Harvey, Kathryn. “Mercy and Physician-Assisted Suicide”. Ethics & Medics (2016): 41- 6, p1-2.
- ↑ http://www.biography.com/people/pope-francis-21152349. Missing or empty
|title=(help) - ↑ Cherry, Mark J. (2015). "Pope Francis, Weak Theology, and the Subtle Transformation of Roman Catholic Bioethics". Christian Bioethics. 21: 84–88. doi:10.1093/cb/cbu045 – via EBSCOhost.
- ↑ "Roman Catholicism". Encyclopædia Britannica. Retrieved 2016-12-07.
- ↑ Harvey, Kathryn. “Mercy and Physician-Assisted Suicide”. Ethics & Medics (2016): 41- 6, p1-2
- ↑ Yao, Teresa. “Can We Limit a Right to Physician-Assisted Suicide?” National Catholic Bioethics Quarterly (2016):16-3.
- ↑ Samuel 1:31:4-5, Daat Zekeinim Baalei Hatosfot Genesis 9:5.
- ↑ Steinberg, Dr. Abraham (1988). Encyclopedia Hilchatit Refuit. Jerusalem: Shaarei Zedek Hospital. p. Vol. 1 Pg. 15.
- ↑ "The Right to Die with Dignity: 1988 General Resolution". Unitarian Universalist Association. Retrieved 4 October 2016.
- ↑ "Handbook 2: Administering the Church – 21.3 Medical and Health Policies". Church of Jesus Christ of Latter-day Saints.
- ↑ "Euthanasia and Prolonging Life". LDS News.
- ↑ "ADAPT and Not Dead Yet File Brief: Physician Assisted Suicide Violates ADA". ADAPT. 1997.
- ↑ "The Yeshiva World Agudath Israel of America Testifies Against Assisted Suicide Bill to New Jersey Senate Health Committee " " Frum Jewish News". theyeshivaworld.com.
- ↑ "Care Not Killing". bmj.com.
- ↑ "Assisted Suicide Laws". Disability Rights Education & Defense Fund.
- ↑ "Family First NZ". Family First NZ.
- ↑ "Conn. Lawmakers Revisit Assisted Suicide Issue". cbslocal.com.
- ↑ "Not Dead Yet Disability Activists Oppose Assisted Suicide As A Deadly Form of Discrimination". Not Dead Yet.
- ↑ http://www.njleg.state.nj.us/MEDIA/OLS_MEDIA_PLAYER.HTM?wma=!{A}http://rmserver.njleg.state.nj.us/internet/2015/SHH/1210-0100PM-M0-1.wma!
- ↑ "Royal College of Physicians". rcplondon.ac.uk.
- ↑ "XII. Problems of bioethics - The Russian Orthodox Church". mospat.ru.
- ↑ "To Live Each Day with Dignity: A Statement on Physician-Assisted Suicide" (PDF). United States Conference of Catholic Bishops. 2011. Retrieved March 10, 2014.
- ↑ "Voice for Life New Zealand - to value and protect human life". voiceforlife.org.nz.
- ↑ "WMA Resolution on Euthanasia". wma.net. 6 October 2002.
- ↑ Kane, MA, Leslie. "Medscape Ethics Report 2014, Part 1: Life, Death, and Pain". Medscape. Retrieved 4 October 2016.
- ↑ Cohen, Jonathan (1994). "Attitudes toward Assisted Suicide and Euthanasia among Physicians in Washington State". The New England Journal of Medicine. 331: 89–94. doi:10.1056/NEJM199407143310206.
- ↑ Seale C (April 2009). "Legalisation of euthanasia or physician-assisted suicide: survey of doctors' attitudes". Palliat Med. 23 (3): 205–12. PMID 19318460. doi:10.1177/0269216308102041.
- ↑ Seale C (April 2009). "End-of-life decisions in the UK involving medical practitioners". Palliat Med. 23 (3): 198–204. PMID 19318459. doi:10.1177/0269216308102042.
- ↑ "Euthanasia regularly practiced in Colombia". NBC News. July 31, 2005.
- ↑ Julien Ponthus (February 20, 2008). "Luxembourg parliament adopts euthanasia law". Reuters.
- ↑ "Supreme court gives Parliament 4-month extension on doctor-assisted dying law". January 15, 2016. Retrieved 28 February 2016.
- ↑
- 1 2 "Frequently Asked Questions – About the Death With Dignity Act". Oregon Health Authority.
- ↑ "Moniteur Belge - Belgisch Staatsblad". fgov.be.
- ↑ "Moniteur Belge - Belgisch Staatsblad". fgov.be.
- ↑ Adams M, Nys H (2003). "Comparative reflections on the Belgian Euthanasia Act 2002". Med Law Rev. 11 (3): 353–76. PMID 16733879. doi:10.1093/medlaw/11.3.353.
- ↑ McDougall & Gorman 2008, p. 93
- 1 2 McDougall & Gorman 2008
- ↑ "24 & ready to die". The Economist. Economist Group. 10 November 2015. Retrieved 11 April 2016.
- ↑ "Right to die: terminal divide in state of euthanasia in Europe - BizNews.com". BizNews.com. 2014-12-12. Retrieved 2016-11-04.
- ↑ Hamilton, Graeme (December 10, 2015). "Is it euthanasia or assisted suicide? Quebec's end-of-life care law explained". National Post. Toronto, Ontario. Retrieved January 5, 2016.
- ↑ "Euthanasia & Physician-Assisted Suicide (PAS) around the World - Euthanasia - ProCon.org". euthanasia.procon.org. Retrieved 2016-12-07.
- ↑ "China: Case of Assisted Suicide Stirs Euthanasia Debate | Global Legal Monitor". www.loc.gov. 2011-08-17. Retrieved 2016-12-07.
- ↑ Whiting, Raymond (2002). A Natural Right to Die: Twenty-Three Centuries of Debate. Westport, Connecticut. p. 41.
- ↑ Martin, Sabrina. "Colombia to Finalize Euthanasia Law in March". PanAm Post. Retrieved 22 July 2015.
- ↑ Nielsen, Morten Ebbe Juul; Andersen, Martin Marchman (2014-07-01). "Bioethics in Denmark: Moving from First- to Second-Order Analysis?". Cambridge Quarterly of Healthcare Ethics. 23 (3): 326–333. ISSN 0963-1801. doi:10.1017/S0963180113000935.
- 1 2 McDougall & Gorman 2008, p. 84
- ↑ McDougall & Gorman 2008, p. 86
- ↑ Heneghan, Tom (1 July 2013). "Francois Hollande Pledges To Legalize Voluntary Euthanasia In France". Huffington Post.
- ↑ "France set to reject Swiss-style euthanasia". thelocal.fr.
- ↑ "German Criminal Code". German Federal Ministry of Justice. Retrieved 9 July 2013.
- 1 2 Wolfslast, Gabriele (2008). ""Physician-Assisted Suicide and the German Criminal Law."". In Birnbacher, Dieter; Dahl, Edgar. Giving Death a Helping Hand: Physician Assisted Suicide and Public Policy. An international Perspective. Germany: Springer. p. 88.
- ↑ "German Criminal Code". German Federal Ministry of Justice. Retrieved 9 July 2013.
- ↑ "BGH Urteil vom 05.07.1983 (1 StR 168/83)". ejura-examensexpress.de.
- ↑ Wolfslast, Gabriele (2008). ""Physician-Assisted Suicide and the German Criminal Law."". In Birnbacher, Dieter; Dahl, Edgar. Giving Death a Helping Hand: Physician Assisted Suicide and Public Policy. An international Perspective. Germany: Springer. p. 90.
- ↑ "German Criminal Code". German Federal Ministry of Justice. Retrieved 9 July 2013.
- ↑ Wolfslast, Gabriele (2008). ""Physician-Assisted Suicide and the German Criminal Law."". In Birnbacher, Dieter; Dahl, Edgar. Giving Death a Helping Hand: Physician Assisted Suicide and Public Policy. An international Perspective. Germany: Springer. p. 92.
- ↑ Wolfslast, Gabriele (2008). ""Physician-Assisted Suicide and the German Criminal Law."". In Birnbacher, Dieter; Dahl, Edgar. Giving Death a Helping Hand: Physician Assisted Suicide and Public Policy. An international Perspective. Germany: Springer. pp. 87–95.
- ↑ "Iceland". alzheimer-europe.org.
- ↑ Humphry, Derek. "Tread Carefully When You Help to Die, Assisted Suicide Laws Around the World". Assisted Suicide. Retrieved 22 July 2015.
- ↑ "Luxembourg strips monarch of legislative role". The Guardian. London. 2008-12-12. Retrieved 9 July 2013.
- ↑ "Luxembourg becomes third EU country to legalize euthanasia". Tehran Times. Archived from the original on June 13, 2011.
- 1 2 McDougall & Gorman 2008, p. 80
- ↑ "SCA overturns right-to-die ruling". News24. 2015-12-06. Retrieved 2015-12-06.
- ↑ Schwarzenegger, Christian; Summers, Sarah J. (2005-02-03). "Hearing with the Select Committee on the Assisted Dying for the Terminally Ill Bill" (PDF). House of Lords Hearings. Zürich: University of Zürich Faculty of Law. (PDF)
- ↑ "Inciting and assisting someone to commit suicide (Verleitung und Beihilfe zum Selbstmord)". Swiss Criminal Code (in German). Zürich: Süisse: Article 115. 1989-06-23.
- ↑ Whiting, Raymond (2002). A Natural Right to Die: Twenty-Three Centuries of Debate. Westport, Connecticut. p. 46.
- ↑ Christian Schwarzenegger and Sarah Summers of the University of Zurich's Faculty of Law (3 February 2005). "Hearing with the Select Committee on the Assisted Dying for the Terminally Ill Bill" (PDF). House of Lords, Zurich.
- ↑ Lundin, Leigh (2009-08-02). "YOUthanasia". Criminal Brief. Retrieved 9 July 2013.
- ↑ "The Suicide Tourist - FRONTLINE - PBS". pbs.org.
- ↑ "BBC News - Switzerland: Zurich votes to keep assisted suicide". BBC News.
- ↑ del Uruguay, Republica Oriental. "Penal Code of Uruguay". Parliament of Uruguay. Retrieved 12 August 2015.
- ↑ Huxtable, RichardHuxtable, Richard (2007). Euthanasia, Ethics and the Law: From Conflict to Compromise. Abingdon, UK; New York: Routledge Cavendish. ISBN 9781844721061.
- ↑ "Assisted Dying Bill - latest". BBC News Online.
- ↑ "DPP publishes interim policy on prosecuting assisted suicide: The Crown Prosecution Service". cps.gov.uk. 23 September 2009. Archived from the original on September 27, 2009.
- ↑ "A Critical Consideration of the Director of Public Prosecutions Guidelines in Relation to Assisted Suicide Prosecutions and their Application to the Law". halsburyslawexchange.co.uk.
- ↑ "Dignity in Dying Poll" (PDF). Populus. 2015. Archived from the original (PDF) on June 17, 2015.
- ↑ James Gallagher & Philippa Roxby (11 September 2015). "Assisted Dying Bill: MPs reject 'right to die' law". BBC News.
- ↑ "End of Life Assistance (Scotland) Bill (SP Bill 38)". The Scottish Parliament. 21 January 2010. Retrieved 12 June 2011.
- ↑ "Margo MacDonald's End of Life Assistance Bill rejected". BBC News Online. 2010-12-01.
- ↑ Lisa Aliferis (March 10, 2016). "California To Permit Medically Assisted Suicide As Of June 9". NPR.
- ↑ http://egov.oregon.gov/DHS/ph/pas/ors.shtml
- 1 2 "State-by-State Guide to Physician-Assisted Suicide - Euthanasia - ProCon.org". procon.org.
- 1 2 "Oregon Public Health Division – 2013 DWDA Report" (PDF). Oregon Health Authority. Retrieved 28 November 2014.
- ↑ Sullivan, Nora. "Vermont Legislature Passes Assisted Suicide Bill." Charlotte Lozier Institute RSS. Charlotte Lozier Institute, 15 May 2013. Web. 04 Dec. 2013.
- ↑ https://newmexico.tylerhost.net/ServeDocument.ashx?SID=0730da82-c2ce-4331-9d34-98fe74190124&RID=001664dd-e045-4d6c-b5ce-1294189b0a7a
- ↑ Richardson, Valerie. "New Mexico court strikes down ruling that allowed assisted suicide". Washington Times. Retrieved 12 August 2015.
- ↑ "The Brittany Fund | About". thebrittanyfund.org. Retrieved 2016-11-04.
- ↑ Groenewoud JH, van der Heide A, Onwuteaka-Philipsen BD, Willems DL, van der Maas PJ, van der Wal G (2000). "Clinical Problems with the Performance of Euthanasia and Physician-Assisted Suicide in the Netherlands". New England Journal of Medicine. 342 (8): 551–6. PMID 10684914. doi:10.1056/NEJM200002243420805.
- ↑ Ganzini L, Goy ER, Dobscha SK (2008). "Prevalence of depression and anxiety in patients requesting physicians' aid in dying: cross sectional survey". BMJ. 337: a1682. PMC 2562435
 . PMID 18842645. doi:10.1136/bmj.a1682.
. PMID 18842645. doi:10.1136/bmj.a1682. - ↑ Rietjens J, van Delden J, Onwuteaka-Philipsen B, Buiting H, van der Maas P, van der Heide A (2008). "Continuous deep sedation for patients nearing death in the Netherlands: descriptive study". BMJ. 336 (7648): 810–3. PMC 2292332
 . PMID 18344245. doi:10.1136/bmj.39504.531505.25.
. PMID 18344245. doi:10.1136/bmj.39504.531505.25. - ↑ "Living and Dying Well". livinganddyingwell.org.uk.
References
- Asch DA, DeKay ML (September 1997). "Euthanasia among US critical care nurses. Practices, attitudes, and social and professional correlates". Med Care. 35 (9): 890–900. JSTOR 3767454. PMID 9298078. doi:10.1097/00005650-199709000-00002.
- McDougall, Jennifer Fecio; Gorman, Martha (2008). Contemporary World Issues: Euthanasia. Santa Barbara, California: ABC-CLIO.
- "What is Physician-Assisted Suicide?". Northwestern University. 17 July 2014.
- "Who Has the Right to a Dignified Death? / The Death Treatment (When should people with a non-terminal illness be helped to die?) Letter from Belgium - RACHEL AVIV". New Yorker. 22 June 2015.
- "The Last Day Of Her Life". New York Times Magazine. 17 May 2015.