Pharyngitis
| Pharyngitis | |
|---|---|
| Synonyms | Acute sore throat |
 | |
| Viral pharyngitis. Note the redness. | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Symptoms | Sore throat, fever, runny nose, cough, headache, hoarse voice[1][2] |
| Complications | Sinusitis, acute otitis media[2] |
| Duration | 3–5 days[2] |
| Causes | Usually viral infection[2] |
| Diagnostic method | Based on symptoms, rapid antigen detection test, throat swab[2] |
| Similar conditions | Epiglottitis, thyroiditis, retropharyngeal abscess[2] |
| Treatment | NSAIDs, lidocaine[3][2] |
| Frequency | ~7.5% of people in any 3-month period[4] |
Pharyngitis is inflammation of the back of the throat, known as the pharynx.[2] It typically results in a sore throat and fever.[2] Other symptoms may include a runny nose, cough, headache, a hoarse voice.[1] Symptoms usually last three to five days. Complications can include sinusitis and acute otitis media.[2] Pharyngitis is typically a type of respiratory tract infection.[5]
Most cases are caused by a viral infection. Strep throat is the cause in about 25% of children and 10% of adults.[2] Uncommon causes include other bacteria such as gonorrhea, fungus, irritants such as smoke, allergies, and gastroesophageal reflux disease.[2][3] Specific testing is not recommended in people who have clear symptoms of a viral infection such as a cold. Otherwise a rapid antigen detection test (RAPD) or throat swab is recommended. Other conditions that can produce similar symptoms include epiglottitis, thyroiditis, retropharyngeal abscess, and occasionally heart disease.[2]
NSAIDs, such as ibuprofen, can be used to help with the pain.[2] Topical lidocaine may also help.[3] Strep throat is typically treated with antibiotics, such as either penicillin or amoxicillin.[2] It is unclear if steroids are useful in acute pharyngitis, other than possibly in severe cases.[6][7]
About 7.5% of people have a sore throat in any three-month period.[4] Two to three episodes in a year is not uncommon.[1] This resulted in 15 million physician visits in the United States in 2007.[3] Pharyngitis is the most common cause of a sore throat.[8] The word comes from the Greek word pharynx meaning "throat" and the suffix -itis meaning "inflammation".[9][10]
Classification
.jpg)
Pharyngitis is a type of inflammation, most commonly caused by an upper respiratory tract infection. It may be classified as acute or chronic. Acute pharyngitis may be catarrhal, purulent or ulcerative, depending on the causative agent and the immune capacity of the affected individual. Chronic pharyngitis may be catarrhal, hypertrophic or atrophic.
Tonsillitis is a sub type of pharyngitis.[11] If the inflammation includes both the tonsils and other parts of the throat, it may be called pharyngotonsillitis.[12] Another sub classification is nasopharyngitis (the common cold).[13]
Cause
The majority of cases are due to an infectious organism acquired from close contact with an infected individual.
Viral
These comprise about 40–80% of all infectious cases and can be a feature of many different types of viral infections.[8][14]
- Adenovirus – the most common of the viral causes. Typically the degree of neck lymph node enlargement is modest and the throat often does not appear red, although it is painful.
- Orthomyxoviridae which cause influenza – present with rapid onset high temperature, headache and generalized ache. A sore throat may be associated.
- Infectious mononucleosis ("glandular fever") caused by the Epstein–Barr virus. This may cause significant lymph gland swelling and an exudative tonsillitis with marked redness and swelling of the throat. The heterophile test can be used if this is suspected.
- Herpes simplex virus can cause multiple mouth ulcers.
- Measles
- Common cold: rhinovirus, coronavirus, respiratory syncytial virus, parainfluenza virus can cause infection of the throat, ear, and lungs causing standard cold-like symptoms and often pain.
Bacterial
A number of different bacteria can infect the human throat. The most common is Group A streptococcus, but others include Streptococcus pneumoniae, Haemophilus influenzae, Bordetella pertussis, Bacillus anthracis, Corynebacterium diphtheriae, Neisseria gonorrhoeae, Chlamydophila pneumoniae, and Mycoplasma pneumoniae.[15]
- Streptococcal pharyngitis
Streptococcal pharyngitis or strep throat is caused by group A beta-hemolytic streptococcus (GAS).[16] It is the most common bacterial cause of cases of pharyngitis (15–30%).[15] Common symptoms include fever, sore throat, and large lymph nodes. It is a contagious infection, spread by close contact with an infected individual. A definitive diagnosis is made based on the results of a throat culture. Antibiotics are useful to both prevent complications and speed recovery.[17]
- Fusobacterium necrophorum
Fusobacterium necrophorum is a normal inhabitant of the oropharyngeal flora and can occasionally create a peritonsillar abscess. In 1 out of 400 untreated cases, Lemierre's syndrome occurs.[18]
- Diphtheria
Diphtheria is a potentially life-threatening upper respiratory infection caused by Corynebacterium diphtheriae which has been largely eradicated in developed nations since the introduction of childhood vaccination programs, but is still reported in the Third World and increasingly in some areas in Eastern Europe. Antibiotics are effective in the early stages, but recovery is generally slow.
- Others
A few other causes are rare, but possibly fatal, and include parapharyngeal space infections: peritonsillar abscess ("quinsy"), submandibular space infection (Ludwig's angina), and epiglottitis.[19][20][21]
Fungal
Some cases of pharyngitis are caused by fungal infection such as Candida albicans causing oral thrush.
Non-infectious
Pharyngitis may also be caused by mechanical, chemical or thermal irritation, for example cold air or acid reflux. Some medications may produce pharyngitis such as pramipexole and antipsychotics.[22][23]
Diagnostic approach
| Points | Probability of Strep | Management |
|---|---|---|
| 1 or less | <10% | No antibiotic or culture needed |
| 2 | 11–17% | Antibiotic based on culture or RAPD |
| 3 | 28–35% | |
| 4 or 5 | 52% | Empiric antibiotics |
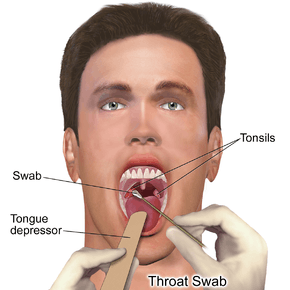
It is hard to differentiate a viral and a bacterial cause of a sore throat based on symptoms alone.[24] Thus often a throat swab is done to rule out a bacterial cause.[25]
The modified Centor criteria may be used to determine the management of people with pharyngitis. Based on 5 clinical criteria, it indicates the probability of a streptococcal infection.[17]
One point is given for each of the criteria:[17]
- Absence of a cough
- Swollen and tender cervical lymph nodes
- Temperature >38.0 °C (100.4 °F)
- Tonsillar exudate or swelling
- Age less than 15 (a point is subtracted if age >44)
The McIsaac criteria adds to the Centor:[26]
- Age less than 15: add one point
- Age greater than 45: subtract one point
The Infectious Disease Society of America however recommends against empirical treatment and considers antibiotics only appropriate following positive testing.[24] Testing is not needed in children under three as both group A strep and rheumatic fever are rare, except if they have a sibling with the disease.[24]
Management
The majority of time treatment is symptomatic. Specific treatments are effective for bacterial, fungal, and herpes simplex infections.
Medications
- Pain medication such as NSAIDs and acetaminophen (paracetamol) can help reduce the pain associated with a sore throat. Aspirin may be used in adults but is not recommended in children due to the risk of Reye syndrome.[27]
- Steroids (such as dexamethasone) may be useful for severe pharyngitis.[28][7] Their general use however is poorly supported.[6]
- Viscous lidocaine relieves pain by numbing the mucus membranes.[29]
- Antibiotics are useful if a bacterial infection is the cause of the sore throat.[30][31] For viral infections, antibiotics have no effect. In the United States they are used in 25% of people before a bacterial infection has been detected.[32]
- Oral analgesic solutions, the active ingredient usually being phenol, but also less commonly benzocaine, cetylpyridinium chloride and/or menthol. Chloraseptic and Cēpacol are two examples of brands of these kinds of analgesics.
Alternative
Gargling salt water is often suggested but evidence looking at its usefulness is lacking.[3] Alternative medicines are promoted and used for the treatment of sore throats.[33] However, they are poorly supported by evidence.[33]
Epidemiology
Acute pharyngitis is the most common cause of a sore throat and, together with cough, it is diagnosed in more than 1.9 million people a year in the United States.[8]
References
- 1 2 3 Rutter, Paul Professor; Newby, David (2015). Community Pharmacy ANZ: Symptoms, Diagnosis and Treatment. Elsevier Health Sciences. p. 19. ISBN 9780729583459.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Hildreth, AF; Takhar, S; Clark, MA; Hatten, B (September 2015). "Evidence-Based Evaluation And Management Of Patients With Pharyngitis In The Emergency Department.". Emergency medicine practice. 17 (9): 1–16; quiz 16–7. PMID 26276908.
- 1 2 3 4 5 Weber, R (March 2014). "Pharyngitis.". Primary care. 41 (1): 91–8. PMID 24439883. doi:10.1016/j.pop.2013.10.010.
- 1 2 Jones, Roger (2004). Oxford Textbook of Primary Medical Care. Oxford University Press. p. 674. ISBN 9780198567820. Retrieved 4 August 2016.
- ↑ "Pharyngitis". National Library of Medicine. Retrieved 4 August 2016.
- 1 2 Principi, N; Bianchini, S; Baggi, E; Esposito, S (February 2013). "No evidence for the effectiveness of systemic corticosteroids in acute pharyngitis, community-acquired pneumonia and acute otitis media.". European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 32 (2): 151–60. PMID 22993127. doi:10.1007/s10096-012-1747-y.
- 1 2 Hayward, G; Thompson, MJ; Perera, R; Glasziou, PP; Del Mar, CB; Heneghan, CJ (17 October 2012). "Corticosteroids as standalone or add-on treatment for sore throat.". The Cochrane database of systematic reviews. 10: CD008268. PMID 23076943. doi:10.1002/14651858.CD008268.pub2.
- 1 2 3 Marx, John (2010). Rosen's emergency medicine: concepts and clinical practice (7th ed.). Philadelphia, Pennsylvania: Mosby/Elsevier. Chapter 30. ISBN 978-0-323-05472-0.
- ↑ Beachey, Will (2013). Respiratory Care Anatomy and Physiology, Foundations for Clinical Practice,3: Respiratory Care Anatomy and Physiology. Elsevier Health Sciences. p. 5. ISBN 0323078664.
- ↑ Hegner, Barbara; Acello, Barbara; Caldwell, Esther (2009). Nursing Assistant: A Nursing Process Approach - Basics. Cengage Learning. p. 45. ISBN 9781111780500.
- ↑ "Tonsillitis". Retrieved 4 August 2016.
- ↑ Rafei K, Lichenstein R (2006). "Airway Infectious Disease Emergencies". Pediatric Clinics of North America. 53 (2): 215–242. PMID 16574523. doi:10.1016/j.pcl.2005.10.001.
- ↑ "www.nlm.nih.gov".
- ↑ Acerra JR. "Pharyngitis". eMedicine. Retrieved 28 April 2010.
- 1 2 Bisno AL (January 2001). "Acute pharyngitis". N Engl J Med. 344 (3): 205–11. PMID 11172144. doi:10.1056/NEJM200101183440308.
- ↑ Baltimore RS (February 2010). "Re-evaluation of antibiotic treatment of streptococcal pharyngitis". Curr. Opin. Pediatr. 22 (1): 77–82. PMID 19996970. doi:10.1097/MOP.0b013e32833502e7.
- 1 2 3 Choby BA (March 2009). "Diagnosis and treatment of streptococcal pharyngitis". Am Fam Physician. 79 (5): 383–90. PMID 19275067.
- ↑ Centor RM (2009-12-01). "Expand the pharyngitis paradigm for adolescents and young adults". Ann Intern Med. 151 (11): 812–5. PMID 19949147. doi:10.7326/0003-4819-151-11-200912010-00011.
- ↑ "UpToDate Inc.". (registration required)
- ↑ Reynolds SC, Chow AW (Sep–Oct 2009). "Severe soft tissue infections of the head and neck: a primer for critical care physicians". Lung. 187 (5): 271–9. PMID 19653038. doi:10.1007/s00408-009-9153-7.
- ↑ Bansal A, Miskoff J, Lis RJ (January 2003). "Otolaryngologic critical care". Crit Care Clin. 19 (1): 55–72. PMID 12688577. doi:10.1016/S0749-0704(02)00062-3.
- ↑ "Mirapex product insert" (PDF). Boehringer Ingelheim. 2009. Retrieved 2010-06-30.
- ↑ "Mosby's Medical Dictionary, 8th edition". Elsevier. 2009. Retrieved 2010-06-30.
- 1 2 3 Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C (Sep 9, 2012). "Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the Infectious Diseases Society of America.". Clinical Infectious Diseases. 55 (10): e86–102. PMID 22965026. doi:10.1093/cid/cis629.
- ↑ Del Mar C (1992). "Managing sore throat: a literature review. I. Making the diagnosis". Med J Aust. 156 (8): 572–5. PMID 1565052.
- ↑ Fine AM, Nizet V, Mandl KD (2012). "Large-Scale Validation of the Centor and McIsaac Scores to Predict Group A Streptococcal Pharyngitis.". Arch Intern Med. 172. PMID 22566485. doi:10.1001/archinternmed.2012.950.
- ↑ Baltimore RS (February 2010). "Re-evaluation of antibiotic treatment of streptococcal pharyngitis". Current Opinion in Pediatrics. 22 (Curr. Opin. Pediatr. 22 (1)): 77–82. PMID 19996970. doi:10.1097/MOP.0b013e32833502e7.
- ↑ Hayward G, Thompson M, Heneghan C, Perera R, Del Mar C, Glasziou P (2009). "Corticosteroids for pain relief in sore throat: systematic review and meta-analysis". BMJ. 339: b2976. PMC 2722696
 . PMID 19661138. doi:10.1136/bmj.b2976.
. PMID 19661138. doi:10.1136/bmj.b2976. - ↑ "LIDOCAINE VISCOUS (Xylocaine Viscous) side effects, medical uses, and drug interactions.".
- ↑ Kocher, JJ; Selby, TD (1 July 2014). "Antibiotics for sore throat.". American family physician. 90 (1): 23–4. PMID 25077497.
- ↑ Spinks, A; Glasziou, PP; Del Mar, CB (5 November 2013). "Antibiotics for sore throat.". The Cochrane database of systematic reviews. 11: CD000023. PMID 24190439. doi:10.1002/14651858.CD000023.pub4.
- ↑ Urkin, J; Allenbogen, M; Friger, M; Vinker, S; Reuveni, H; Elahayani, A (November 2013). "Acute pharyngitis: low adherence to guidelines highlights need for greater flexibility in managing paediatric cases.". Acta paediatrica (Oslo, Norway : 1992). 102 (11): 1075–80. PMID 23879261. doi:10.1111/apa.12364.
- 1 2 "Sore throat: Self-care". Mayo Clinic. Retrieved 2007-09-17.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
| Wikimedia Commons has media related to Pharyngitis. |