Pelvimetry

Pelvimetry is the assessment of the female pelvis[1] in relation to the birth of a baby. Traditional obstetrical services relied heavily on pelvimetry in the conduct of delivery in order to decide if natural or operative vaginal delivery was possible or if and when to use a cesarean section.[2]
Use
Pelvimetry used to be performed routinely to discern if spontaneous labour was medically advisable. Women whose pelvises were deemed too small received caesarean sections instead of birthing naturally. Research indicates that pelvimetry is not a useful diagnostic tool for CPD (see below) and that in all cases spontaneous labour and birthing should be facilitated.[3]
A woman's pelvis loosens up before birth (with the help of hormones), and an upright and/or squatting woman can birth a considerably larger baby. A woman in the lithotomy (lying on her back, legs elevated) is more than likely not going to push a larger than average baby out, due to the size of outlet that this position creates.
Cephalo-pelvic disproportion: CPD
Cephalo-pelvic disproportion exists when the capacity of the pelvis is inadequate to allow the fetus to negotiate the birth canal.
Terminology
The terms used in pelvimetry are commonly used in obstetrics. Clinical pelvimetry attempts to assess the pelvis by clinical examination. Pelvimetry can also be done by radiography and MRI.
Pelvic planes
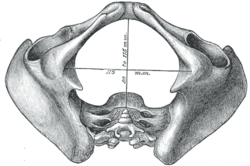
- Pelvic inlet: The line between the narrowest bony points formed by the sacral promontory and the inner pubic arch is termed obstetrical conjugate: It should be 11.5 cm or more. This anteroposterior line at the inlet is 2 cm less than the diagonal conjugate (distance from undersurface of pubic arch to sacral promontory). The transverse diameter of the pelvic inlet measures 13.5 cm.
- Interspinous distance: The line between the narrowest bone points connects the ischial spines; it typically exceeds 12 cm.
- Pelvic outlet: The distance between the ischial tuberosities (normally > 10 cm), and the angulation of the pubic arch.
Low-dose 3D-rendered CT scans can be used for estimating pelvimetry parameters:[4]
 Transverse diameter of pelvic inlet (1), and interspinous diameter (2).[4]
Transverse diameter of pelvic inlet (1), and interspinous diameter (2).[4] Obstetric conjugate (1), and pelvic outlet (2).[4]
Obstetric conjugate (1), and pelvic outlet (2).[4] Intertuberous diameter.[4]
Intertuberous diameter.[4]
Pelvic types
Traditional obstetrics characterizes four types of pelvises:
- Gynecoid: Ideal shape, with round to slightly oval (obstetrical inlet slightly less transverse) inlet: best chances for normal vaginal delivery.
- Android: triangular inlet, and prominent ischial spines, more angulated pubic arch.
- Anthropoid: the widest transverse diameter is less than the anteroposterior (obstetrical) diameter.
- Platypelloid: Flat inlet with shortened obstetrical diameter. Predispose to an occiput transverse presentation
Fetal relationship
- Engagement: The fetus is engaged if the widest leading part (typically the widest circumference of the head) is negotiating the inlet.
- Station: Relationship of the bony presenting part of the fetus to the maternal ischial spines. If at the level of the spines it is at “0 (zero)” station, if it passed it by 2cm it is at “+2” station.
- Attitude: Relationship of fetal head to spine: flexed, neutral (“military”), or extended attitudes are possible.
- Position: Relationship of presenting part to maternal pelvis, i.e. ROP=right occiput posterior, or LOA=left occiput anterior.
- Presentation: Relationship between the leading fetal part and the pelvic inlet: cephalic, breech (complete, incomplete, frank or footling), face, brow, mentum or shoulder presentation.
- Lie: Relationship between the longitudinal axis of fetus and long axis of the uterus: longitudinal, oblique, and transverse.
- Caput or Caput succedaneum: oedema typically formed by the tissue overlying the fetal skull during the vaginal birthing process.
See also
- Childbirth
- List of obstetric topics
- Pelvic Bone Width
- Human pelvis
- Pregnancy
- Pubic symphysis
- Sacroiliac joint
- Sacrum
References
- ↑ "pelvimetry" at Dorland's Medical Dictionary
- ↑ Herbert Thoms (1946). "Yale - The Pelvic Survey" (PDF).
- ↑ Blackadar CS, Viera A: "A Retrospective Review of Performance and Utility of Routine Clinical Pelvimetry", AAFP, 2003, v36:7, p505
- 1 2 3 4 Salk, Ismail; Cetin, Ali; Salk, Sultan; Cetin, Meral (2016). "Pelvimetry by Three-Dimensional Computed Tomography in Non-Pregnant Multiparous Women Who Delivered Vaginally". Polish Journal of Radiology. 81: 219–227. ISSN 0137-7183. doi:10.12659/PJR.896380.