Pathophysiology of asthma
| Pathophysiology of asthma | |
|---|---|
 | |
| Figure A shows the location of the lungs and airways in the body. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway during asthma symptoms. | |
| Classification and external resources | |
| Specialty | pulmonology |
| ICD-10 | J45 |
| ICD-9-CM | 493 |
| OMIM | 600807 |
| DiseasesDB | 1006 |
| MedlinePlus | 000141 |
| eMedicine | article/806890 |
| MeSH | D001249 |
Asthma is a common pulmonary condition defined by chronic inflammation of respiratory tubes, tightening of respiratory smooth muscle, and episodes of bronchoconstriction.[1] The Centers for Disease Control and Prevention estimate that 1 in 11 children and 1 in 12 adults have asthma in the United States of America.[1] According to the World Health Organization, asthma affects 235 million people worldwide.[2] There are two major categories of asthma: allergic and non-allergic. The focus of this article will be allergic asthma. In both cases, bronchoconstriction is prominent.[1]
Bronchoconstriction
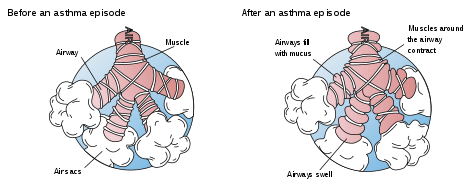
During an asthma episode, inflamed airways react to environmental triggers such as smoke, dust, or pollen. The airways narrow and produce excess mucus, making it difficult to breathe. In essence, asthma is the result of an immune response in the bronchial airways.[3]
The airways of asthma patients are "hypersensitive" to certain triggers, also known as stimuli (see below). (It is usually classified as type I hypersensitivity.)[4][5] In response to exposure to these triggers, the bronchi (large airways) contract into spasm (an "asthma attack"). Inflammation soon follows, leading to a further narrowing of the airways and excessive mucus production, which leads to coughing and other breathing difficulties. Bronchospasm may resolve spontaneously in 1–2 hours, or in about 50% of subjects, may become part of a 'late' response, where this initial insult is followed 3–12 hours later with further bronchoconstriction and inflammation.[6]
The normal caliber of the bronchus is maintained by a balanced functioning of the autonomic nervous system, which both operates reflexively. The parasympathetic reflex loop consists of afferent nerve endings which originate under the inner lining of the bronchus. Whenever these afferent nerve endings are stimulated (for example, by dust, cold air or fumes) impulses travel to the brain-stem vagal center, then down the vagal efferent pathway to again reach the bronchial small airways. Acetylcholine is released from the efferent nerve endings. This acetylcholine results in the excessive formation of inositol 1,4,5-trisphosphate (IP3) in bronchial smooth muscle cells which leads to muscle shortening and this initiates bronchoconstriction.
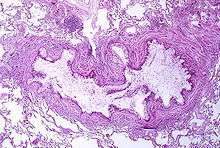
Bronchial inflammation
The mechanisms behind allergic asthma—i.e., asthma resulting from an immune response to inhaled allergens—are the best understood of the causal factors. In both people with asthma and people who are free of the disease, inhaled allergens that find their way to the inner airways are ingested by a type of cell known as antigen-presenting cells, or APCs. APCs then "present" pieces of the allergen to other immune system cells. In most people, these other immune cells (TH0 cells) "check" and usually ignore the allergen molecules. In asthma patients, however, these cells transform into a different type of cell (TH2), for reasons that are not well understood. A possible reason could be the release of Interleukin-4 by Mast cells that induce differentiation of naive helper T cells (Th0 cells) to Th2 cells.
The resultant TH2 cells activate an important arm of the immune system, known as the humoral immune system. The humoral immune system produces antibodies against the inhaled allergen. Later, when a patient inhales the same allergen, these antibodies "recognize" it and activate a humoral response. Inflammation results: chemicals are produced that cause the wall of the airway to thicken, cells which produce scarring to proliferate and contribute to further 'airway remodeling', causes mucus producing cells to grow larger and produce more and thicker mucus, and the cell-mediated arm of the immune system is activated. Inflamed airways are more hyper-reactive, and will be more prone to bronchospasm.
The "hygiene hypothesis" postulates that an imbalance in the regulation of these TH cell types in early life leads to a long-term domination of the cells involved in allergic responses over those involved in fighting infection. The suggestion is that for a child being exposed to microbes early in life, taking fewer antibiotics, living in a large family, and growing up in the country stimulate the TH1 response and reduce the odds of developing asthma.[7]
Asthma is associated with a procoagulant state in the bronchoalveolar space.[8]
Stimuli
- Allergens from nature, typically inhaled, which include waste from common household pests, the house dust mite and cockroach, as well as grass pollen, mold spores, and pet epithelial cells;[9]
- Indoor air pollution from volatile organic compounds, including perfumes and perfumed products. Examples include soap, dishwashing liquid, laundry detergent, fabric softener, paper tissues, paper towels, toilet paper, shampoo, hairspray, hair gel, cosmetics, facial cream, sun cream, deodorant, cologne, shaving cream, aftershave lotion, air freshener and candles, and products such as oil-based paint.[9][10]
- Medications, including aspirin,[11] β-adrenergic antagonists (beta blockers),[12] ibuprofen, and penicillin.[13]
- Food allergies such as milk, peanuts, and eggs. However, asthma is rarely the only symptom, and not all people with food or other allergies have asthma [14]
- Sulfite sensitivity Asthma can occur in reaction to ingestion or inhalation of sulfites, which are added to foods and wine as preservatives.[15]
- Salicylate sensitivity Salicylates can trigger asthma in sensitive individuals. Salicylates occur naturally in many healthy foods. Aspirin is also a salicylate.[16]
- Use of fossil fuel related allergenic air pollution, such as ozone, smog, summer smog, nitrogen dioxide, and sulfur dioxide, which is thought to be one of the major reasons for the high prevalence of asthma in urban areas.[10]
- Various industrial compounds (e.g. toluene diisocyanate [17]) and other chemicals, notably sulfites; chlorinated swimming pools generate chloramines—monochloramine (NH2Cl), dichloramine (NHCl2) and trichloramine (NCl3)—in the air around them, which are known to induce asthma.[18]
- Early childhood infections, especially viral upper respiratory tract infections. Children who suffer from frequent respiratory infections prior to the age of six are at higher risk of developing asthma, particularly if they have a parent with the condition. However, persons of any age can have asthma triggered by colds and other respiratory infections even though their normal stimuli might be from another category (e.g. pollen) and absent at the time of infection. In many cases, significant asthma may not even occur until the respiratory infection is in its waning stage, and the person is seemingly improving.[10] In children, the most common triggers are viral illnesses such as those that cause the common cold.[19]
- Exercise or intense use of respiratory system—the effects of which differ somewhat from those of the other triggers, since they are brief. They are thought to be primarily in response to the exposure of the airway epithelium to cold, dry air.
- Hormonal changes in adolescent girls and adult women associated with their menstrual cycle can lead to a worsening of asthma. Some women also experience a worsening of their asthma during pregnancy whereas others find no significant changes, and in other women their asthma improves during their pregnancy.[10]
- Psychological stress. There is growing evidence that psychological stress is a trigger. It can modulate the immune system, causing an increased inflammatory response to allergens and pollutants.[20]
- Cold weather can make it harder for patients to breathe.[21] Whether high altitude helps or worsens asthma is debatable and may vary from person to person.[22]
Pathogenesis
The fundamental problem in asthma appears to be immunological: young children in the early stages of asthma show signs of excessive inflammation in their airways. Epidemiological findings give clues as to the pathogenesis: the incidence of asthma seems to be increasing worldwide, and asthma is now very much more common in affluent countries.
In 1968 Andor Szentivanyi first described The Beta Adrenergic Theory of Asthma; in which blockage of the Beta-2 receptors of pulmonary smooth muscle cells causes asthma.[23] Szentivanyi's Beta Adrenergic Theory is a citation classic[24] using the Science Citation Index and has been cited more times than any other article in the history of the Journal of Allergy and Clinical Immunology.
In 1995 Szentivanyi and colleagues demonstrated that IgE blocks beta-2 receptors.[25] Since overproduction of IgE is central to all atopic diseases, this was a watershed moment in the world of allergies.[26]
Asthma and sleep apnea
It is recognized with increasing frequency that patients who have both obstructive sleep apnea and asthma often improve tremendously when the sleep apnea is diagnosed and treated.[27] CPAP is not effective in patients with nocturnal asthma only.[28]
Asthma and gastro-esophageal reflux disease
If gastro-esophageal reflux disease (GERD) is present, the patient may have repetitive episodes of acid aspiration. GERD may be common in difficult-to-control asthma, but according to one study, treating it does not seem to affect the asthma.[29] When there is a clinical suspicion for GERD as the cause of the asthma, an Esophageal pH Monitoring is required to confirm the diagnosis and establish the relationship between GERD and asthma.
Asthma and exposure to air pollution during pregnancy
Asthma affects four to eight out of a hundred pregnant women.[30] This is due to the fact that during pregnancy, there is an immunological shift due to hormonal fluctuations.[31] In some cases, there is an increase in Estrogen levels which in turn reduce the activity of natural killer cells, Th1 cell production of inflammatory cytokines, and production of anti-inflammatory cytokines.[31] As we have seen, these play an important role in the pathophysiology of asthma.
Researchers found a link between the preterm birth and exposure to air pollution in asthmatic pregnant women.[32] Results suggested that women with asthma have a higher risk of preterm birth.[32] Researchers suggested that asthmatic episodes in pregnant women were associated with ongoing exposure to nitrogen dioxide and carbon monoxide - types of air pollutants.[32]
Researchers also studied when women were most susceptible to develop asthma. Data indicated that women were at a higher risk of developing asthma when exposed to pollutants before conception and during pregnancy.[32] In particular, "an increase of 30 parts per billion (ppb) in nitrogen oxide exposure in the three months prior to pregnancy increased preterm birth risk by nearly 30 percent for women with asthma, compared to 8 percent for women without asthma."[32]
In other studies, Scientists have found a link between asthma in children and prenatal exposure to air pollution. Results from a study that consisted of 65, 000 Canadian children suggested that children of mothers who lived near highways during pregnancy had a 25% increased risk of developing asthma before the age of five when compared with children of mothers who did not live near highways.[33] Highways are a major source of traffic-related air pollution such that there is an accumulation of air pollutants such as nitrogen dioxide and carbon monoxide (emitted from vehicles) in the vicinity of highways.[33]
In another study, researchers collected data from 6,000 children attending public schools in California. The results suggested that a high exposure to prenatal air pollution was strongly correlated with increased susceptibility to asthma during childhood.[34]
References
- 1 2 3 Jiang, Lan; Diaz, Philip T.; Best, Thomas M.; Stimpfl, Julia N.; He, Feng; Zuo, Li. "Molecular characterization of redox mechanisms in allergic asthma". Annals of Allergy, Asthma & Immunology. 113 (2): 137–142. doi:10.1016/j.anai.2014.05.030.

- ↑ "Asthma". World Health Organization. Archived from the original on June 29, 2011. Retrieved 2016-03-29.
- ↑ Maddox L, Schwartz DA (2002). "The pathophysiology of asthma". Annu. Rev. Med. 53: 477–98. PMID 11818486. doi:10.1146/annurev.med.53.082901.103921.
- ↑ "Lecture 14: Hypersensitivity". Archived from the original on 2009-07-21. Retrieved 2008-09-18.
- ↑ "Allergy & Asthma Disease Management Center: Ask the Expert". Archived from the original on 2007-02-16. Retrieved 2008-09-18.
- ↑ Murray and Nadel's Textbook of Respiratory Medicine, 4th Ed. Robert J. Mason, John F. Murray, Jay A. Nadel, 2005, Elsevier pp. 334
- ↑ Tippets B, Guilbert TW (2009). "Managing Asthma in Children: Part 1: Making the Diagnosis, Assessing Severity". Consultant for Pediatricians. 8 (5).
- ↑ de Boer JD, Majoor CJ, van 't Veer C, Bel EH, van der Poll T (April 2012). "Asthma and coagulation". Blood. 119 (14): 3236–44. PMID 22262775. doi:10.1182/blood-2011-11-391532.
- 1 2 Middleton's Allergy Principles & Practice, N. F. Adkinson, B. S. Bochner, W. W. Busse, S. T. Holgate, R. F. Lemanske, F. E. R. Simons. Chapter 33: "Indoor Allergens." 2008. Elsevier.
- 1 2 3 4 Saunders (2005). "Asthma". Mason: Murray & Nadel's Textbook of Respiratory Medicine (Homer A. Boushey Jr. M.D. David B. Corry M.D. John V. Fahy M.D. Esteban G. Burchard M.D. Prescott G. Woodruff M.D. et al. (eds)) (4th ed.). Elsevier.
- ↑ Jenkins C, Costello J, Hodge L (2004). "Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice". BMJ. 328 (7437): 434. PMC 344260
 . PMID 14976098. doi:10.1136/bmj.328.7437.434.
. PMID 14976098. doi:10.1136/bmj.328.7437.434. - ↑ Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 8th ed. John M. Miller, Douglas P. Zipes. "CHAPTER 33 - Therapy for Cardiac Arrhythmias." 2007. Elsevier.
- ↑ Middleton's Allergy Principles & Practice, N. F. Adkinson, B. S. Bochner, W. W. Busse, S. T. Holgate, R. F. Lemanske, F. E. R. Simons. "Chapter 42 - Epidemiology of Asthma and Allergic Diseases — Risk factors for Asthma" 2008. Elsevier.
- ↑ Middleton's Allergy Principles & Practice, N. F. Adkinson, B. S. Bochner, W. W. Busse, S. T. Holgate, R. F. Lemanske, F. E. R. Simons. "Chapter 65 – Adverse Reactions to Foods: Respiratory Food Hypersensitivity Reactions" 2008. Elsevier.
- ↑ The Australasian Society of Clinical Immunology and Allergy (3 May 2010). "Sulfite Allergy". ASCIA. Archived from the original on 2012-03-04.
- ↑ Towns SJ, Mellis CM (1984). "Role of acetyl salicylic acid and sodium metabisulfite in chronic childhood asthma". Pediatrics. 73 (5): 631–7.
- ↑ Mapp CE, Boschetto P, Maestrelli P, Fabbri LM (2005). "Occupational Asthma". American Journal of Respiratory and Critical Care Medicine. 172 (1): 280–305. PMID 15860754. doi:10.1164/rccm.200311-1575SO.
- ↑ Nemery B, Hoet PH, Nowak D (2002). "Indoor swimming pools, water chlorination and respiratory health". Eur. Respir. J. 19 (5): 790–3. PMID 12030714. doi:10.1183/09031936.02.00308602.
- ↑ Zhao J, Takamura M, Yamaoka A, Odajima Y, Iikura Y (February 2002). "Altered eosinophil levels as a result of viral infection in asthma exacerbation in childhood". Pediatr Allergy Immunol. 13 (1): 47–50. PMID 12000498. doi:10.1034/j.1399-3038.2002.00051.x.
- ↑ Chen E, Miller GE (2007). "Stress and inflammation in exacerbations of asthma". Brain Behav Immun. 21 (8): 993–9. PMC 2077080
 . PMID 17493786. doi:10.1016/j.bbi.2007.03.009.
. PMID 17493786. doi:10.1016/j.bbi.2007.03.009. - ↑ Lloyd, Stacey (2006-11-08). "Why Cold Air Causes Breathing Difficulty in Lung Disease Patients". About: Lung Diseases. Archived from the original on 2007-01-02.
- ↑ "Asthma and Altitude". Body Results.
- ↑ Szentivanyi, Andor (1968). "The Beta Adrenergic Theory of the Atopic Abnormality in Asthma". J.Allergy. 42: 203–232. doi:10.1016/S0021-8707(68)90117-2.
- ↑ Lockey, Richard, In lasting tribute: Andor Szentivanyi, MD. J. Allergy and Clinical Immunology, January, 2006
- ↑ Szentivanyi A.; Ali K.; Calderon EG.; Brooks SM.; Coffey RG.; Lockey RF. (1993). "The in vitro effect of Immunoglobulin E {IgE} on cyclic AMP concentrations in A549 human pulmonary epithelial cells with or without beta adrenergic stimulation". The Journal of Allergy and Clinical Immunology. 91: 379. - Part of Abstracts from:
"50th Anniversary of the American Academy of Allergy and Immunology. 49th Annual Meeting. Chicago, Illinois, March 12–17, 1993. Abstracts". The Journal of Allergy and Clinical Immunology. 91 (1 Pt 2): 141–379. 1993. PMID 8421135. doi:10.1016/0091-6749(93)90360-R. - ↑ Kowalak JP; Hughes AS; et al., eds. (2001). Professional Guide To Diseases (7th ed.). Springhouse.
- ↑ "Breathing disorders during sleep are common among asthma patients, may help predict severe asthma" (Press release). University of Michigan Health System. May 25, 2005. Archived from the original on 2006-01-18. Retrieved September 23, 2006.
- ↑ Basner RC (July 25, 2006). "Asthma and OSA". American Sleep Apnea Association. Archived from the original on 2011-06-15. Retrieved September 23, 2006.
- ↑ Leggett JJ, Johnston BT, Mills M, Gamble J, Heaney LG (2005). "Prevalence of gastroesophageal reflux in difficult asthma: relationship to asthma outcome". Chest. 127 (4): 1227–31. PMID 15821199. doi:10.1378/chest.127.4.1227. Archived from the original on 2007-09-27.
- ↑ "Asthma during pregnancy". www.marchofdimes.org. Retrieved 2016-03-29.
- 1 2 Robinson, Dionne P.; Klein, Sabra L. (2012-08-01). "Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis". Hormones and Behavior. 62 (3): 263–271. ISSN 0018-506X. PMC 3376705
 . PMID 22406114. doi:10.1016/j.yhbeh.2012.02.023.
. PMID 22406114. doi:10.1016/j.yhbeh.2012.02.023. - 1 2 3 4 5 "AIR POLLUTION INCREASES PRETERM BIRTH RISK FOR WOMEN WITH ASTHMA". March 1, 2016. Retrieved 2016-03-29.
- 1 2 Sbihi, Hind; Tamburic, Lillian; Koehoorn, Mieke; Brauer, Michael (2016-02-09). "Perinatal air pollution exposure and development of asthma from birth to age 10 years". European Respiratory Journal. 47: ERJ–00746–2015. ISSN 0903-1936. PMID 26862123. doi:10.1183/13993003.00746-2015.
- ↑ "Air Pollution Impacts on Infants and Children, UCLA Institute of the Environment and Sustainability". www.environment.ucla.edu. Retrieved 2016-03-29.