Hydromorphone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Dilaudid, Hydromorph Contin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682013 |
| Pregnancy category | |
| Dependence liability | Very High |
| Routes of administration | oral, intramuscular, intravenous, subcutaneous, intranasal, rectal, sublingual, transmucosal, buccal, transdermal (experimental) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Oral: 30–35%, Intranasal: 52–58%[1] IV/IM:100% |
| Protein binding | 20% |
| Metabolism | Hepatic |
| Biological half-life | 2–3 hours[2] |
| Excretion | Renal |
| Identifiers | |
| |
| Synonyms | dihydromorphinone |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.006.713 |
| Chemical and physical data | |
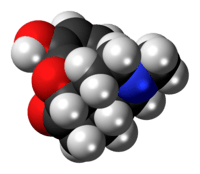
| Formula | C17H19NO3 |
| Molar mass | 285.3g/mol |
| 3D model (JSmol) | |
| Solubility in water | HCl: 333 mg/mL (20 °C) |
| |
| |
| (verify) | |
Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is a centrally acting pain medication of the opioid class. It is a derivative of morphine; to be specific, it is a hydrogenated ketone thereof. Comparatively, hydromorphone is to morphine as hydrocodone is to codeine—that is, a semi-synthetic drug. In medical terms, it is an opioid analgesic and, in legal terms, a narcotic. Hydromorphone is commonly used in the hospital setting, mostly intravenously (IV) because its bioavailability is very low orally, rectally, and intranasally. Sublingual administration (under the tongue) is usually superior to swallowing for bioavailability and effects; however, hydromorphone is bitter and hydrophilic like most opiates, not lipophilic, so it is absorbed poorly and slowly through mouth membranes.[3]
Hydromorphone is much more soluble in water than morphine and, therefore, hydromorphone solutions can be produced to deliver the drug in a smaller volume of water. The hydrochloride salt is soluble in three parts of water, whereas a gram of morphine hydrochloride dissolves in 16 ml of water; for all common purposes, the pure powder for hospital use can be used to produce solutions of virtually arbitrary concentration. When the powder has appeared on the street, this very small volume of powder needed for a dose means that overdoses are likely for those who mistake it for heroin or other powdered narcotics, especially those that have been cut or 'stepped on' already.[4]
Very small quantities of hydromorphone are detected in assays of opium on rare occasions; it appears to be produced by the plant under circumstances and by processes which are not understood at this time and may include the action of bacteria. A similar process or other metabolic processes in the plant may very well be responsible for the very low quantities of hydrocodone also found on rare occasions in opium and alkaloid mixtures derived from opium. Dihydrocodeine, oxymorphol, oxycodone, oxymorphone, metopon, and possibly other derivatives of morphine and hydromorphone also are found in trace amounts in opium.
Side effects
Adverse effects of hydromorphone are similar to those of other potent opioid analgesics, such as morphine and heroin. The major hazards of hydromorphone include dose-related respiratory depression, urinary retention, bronchospasm and sometimes circulatory depression.[5] More common side effects include light-headedness, dizziness, sedation, itching, constipation, nausea, vomiting, headache, sweating, and hallucinations.[5] These symptoms are common in ambulatory patients and in those not experiencing severe pain.
Simultaneous use of hydromorphone with other opioids, muscle relaxants, tranquilizers, sedatives, and general anesthetics can cause a significant increase in respiratory depression, progressing to coma or death. Taking benzodiazepines (such as diazepam) in conjunction with hydromorphone may increase side effects such as dizziness and difficulty concentrating.[6] If simultaneous use of these drugs is required, dose adjustment can be done.[7]
A particular problem that may occur with hydromorphone is accidental administration in place of morphine due to a mix-up between the similar names, either at the time the prescription is written or when the drug is dispensed. This has led to several deaths and calls for hydromorphone to be distributed in distinctly different packaging from morphine to avoid confusion.[8][9]
Massive overdoses are rarely observed in opioid-tolerant individuals, but when they occur, they may lead to circulatory system collapse. Symptoms of overdose include respiratory depression, drowsiness leading to coma and sometimes to death, drooping of skeletal muscles, low heart rate and decreasing blood pressure. At the hospital, individuals with hydromorphone overdose are provided supportive care such as assisted ventilation to provide oxygen, gut decontamination using activated charcoal through a nasogastric tube. Opioid antagonist such as naloxone can also be administered concurrent with oxygen supplementation. Naloxone works by reversing the effects of hydromorphone. It is only administered in the presence of significant respiratory depression and circulatory depression.[7]
The effects of overdose can be exacerbated by dose dumping if the medication is taken with alcohol.[10]
Sugar cravings associated with hydromorphone use are the result of a glucose crash after transient hyperglycemia following injection or a less profound lowering of blood sugar over a period of hours, in common with morphine, heroin, codeine, and other opiates.
Hormone imbalance
As with other opioids, hydromorphone (particularly during heavy chronic use) often causes temporary hypogonadism or hormone imbalance.[11]
Neurotoxicity
In the setting of prolonged use, high dosage, and/or kidney dysfunction, hydromorphone has been associated with neuroexcitatory symptoms such as tremor, myoclonus, agitation, and cognitive dysfunction.[12][13][14] This toxicity is less than that associated with other classes of opioids such as the pethidine class of synthetics in particular.
Withdrawal
Users of hydromorphone can experience painful symptoms if the drug is suspended.[15] Some people can not tolerate the symptoms which result in continuous drug use[15] Symptoms of opioid withdrawal are not easy to decipher. There are differences between drug-seeking behaviors and true withdrawal effects.[16] Symptoms associated with hydromorphone withdrawal include:[15][16][17]
- Nausea
- Vomiting
- Abdominal pain
- Inability to enjoy daily activities
- Muscle and joint pain
- Runny nose and excessive secretion of tears
- Goose bump skin
- Sweating
- Depression
- Anxiety/Panic Attacks
In the clinical setting excessive secretion of tears, yawning and dilation of pupils are helpful presentations in diagnosing opioid withdrawal.[18] Hydromorphone is a rapid acting pain killer, however some formulations can last up to several hours, patients who stop taking this drug abruptly might experience withdrawal symptoms.[17][19] These can start within hours of taking the last dose of hydromorphone and can last up to several weeks.[15] Withdrawal symptoms in people who stopped taking the opioid can be managed by using opioids or non-opioid adjuncts.[20] Methadone is an opioid commonly used for this kind of therapy. However, the selection of therapy should be tailored to each specific person.[21] Methadone is also used for detoxification in people who have opioid addiction such as heroin or drugs similar to morphine.[21] It can be given orally or intramuscularly. There is controversy regarding the use of opioids for people experiencing withdrawal symptoms since these agents can themselves cause relapse on patients when they suspend therapy[15] Clonidine is a non-opioid adjunct that can be used in situations where opioid use is not desired such as in patients with high blood pressure.[22]
Interactions
CNS depressants may enhance the depressant effects of hydromorphone, such as other opioids, anesthetics, sedatives, hypnotics, barbiturates, benzodiazepines, phenothiazines, chloral hydrate, dimenhydrinate, and glutethimide. The depressant effect of hydromorphone may also be enhanced by MAO inhibitors (including procarbazine), first-generation antihistamines (brompheniramine, promethazine, diphenhydramine, chlorpheniramine), beta-blockers, and alcohol. When combined therapy is contemplated, the dose should be reduced of one or both agents.[12]
Pharmacology
Hydromorphone is a semi-synthetic μ-opioid agonist. As a hydrogenated ketone of morphine, it shares the pharmacologic properties typical of opioid analgesics. Hydromorphone and related opioids produce their major effects on the central nervous system and gastrointestinal tract. These include analgesia, drowsiness, mental clouding, changes in mood, euphoria or dysphoria, respiratory depression, cough suppression, decreased gastrointestinal motility, nausea, vomiting, increased cerebrospinal fluid pressure, increased biliary pressure, and increased pinpoint constriction of the pupils.[23]
Formulations


Hydromorphone is available in parenteral, rectal, subcutaneous, and oral formulations. It can also be administered via epidural or intrathecal injection.[24] Hydromorphone has also been administered via nebulization to treat shortness of breath, but it is not used as a route for pain control due to low bioavailability.[25]
Battery-powered intrathecal drug delivery systems are implanted for chronic pain when other options are ruled out, such as surgery and traditional pharmacotherapy, provided that the patient is considered a suitable fit in terms of any contraindications, both physiological and psychological.[26]
An extended-release (once-daily) version of hydromorphone is available in the United States.[27] Previously, an extended-release version of hydromorphone, Palladone, was available before being voluntarily withdrawn from the market after a July 2005 FDA advisory warned of a high overdose potential when taken with alcohol. As of March 2010, it is still available in the United Kingdom under the brand name Palladone SR, Nepal under the brand name Opidol, and in most other European countries.[28][29]
Pharmacokinetics
The chemical modification of the morphine molecule to hydromorphone results in higher lipid solubility and greater ability to cross the blood–brain barrier to produce more rapid and complete central nervous system penetration. On a per milligram basis, hydromorphone is considered to be five times as potent as morphine; although the conversion ratio can vary from 4–8 times, five times is in typical clinical usage.[30][31] The development of tolerance also can vary in among individuals.
Patients with renal abnormalities must exercise caution when dosing hydromorphone. In those with renal impairment, the half-life of hydromorphone can increase to as much as 40 hours. The typical half-life of intravenous hydromorphone is 2.3 hours.[32] Peak plasma levels usually occur between 30 and 60 minutes after oral dosing.[33]
The onset of action for hydromorphone administered intravenously is less than 5 minutes and within 30 minutes of oral administration (immediate release).[25]
Metabolism
While other opioids in its class such as codeine or oxycodone are metabolized via CYP450 enzymes, hydromorphone is not.[34] Hydromorphone is extensively metabolized in the liver to hydromorphone-3-glucoronide, which has no analgesic effects. As similarly seen with the morphine metabolite, morphine-3-glucoronide, a build-up in levels of hydromorphone-3-glucoronide can produce excitatory neurotoxic effects such as restlessness, myoclonus and hyperalgesia. Patients with compromised kidney function and older patients are at higher risk for metabolite accumulation.[35][36]
Chemistry
Hydromorphone is made from morphine either by direct re-arrangement (made by reflux heating of alcoholic or acidic aqueous solution of morphine in the presence of platinum or palladium catalyst) or reduction to dihydromorphine (usually via catalytic hydrogenation), followed by oxidation with benzophenone in presence of potassium tert butoxide or aluminium tert butoxide (Oppenauer oxidation). The 6 ketone group can be replaced with a methylene group via the Wittig reaction to produce 6-Methylenedihydrodesoxymorphine, which is 80× stronger than morphine.[37]
Changing morphine into hydromorphone increases its activity and, therefore, makes hydromorphone about eight times stronger than morphine on a weight basis, all other things being equal. Changed also is lipid solubility, contributing to hydromorphone's having a more rapid onset of action and alterations to the overall absorption, distribution, metabolism, and elimination profile as well as the side effect profile (in general, less nausea and itching) versus that of morphine. The semi-synthetic opiates, of which hydromorphone and its codeine analogue hydrocodone are among the best-known and oldest, include a huge number of drugs of varying strengths and with differences among themselves both subtle and stark, allowing for many different options for treatment.
Endogenous production
Hydromorphone is made from morphine via catalytic hydrogenation and is also produced in trace amounts by human and other mammalian metabolism of morphine and occasionally appears in assays of opium latex in very small quantities, apparently forming in the plant in an unknown percentage of cases under poorly understood conditions.
Bacteria
Some bacteria have been shown to be able to turn morphine into closely related drugs including hydromorphone and dihydromorphine among others. The bacterium Pseudomonas putida serotype M10 produces a naturally occurring NADH-dependent morphinone reductase that can work on unsaturated 7,8 bonds, with result that, when these bacteria are living in an aqueous solution containing morphine, significant amounts of hydromorphone form, as it is an intermediary metabolite in this process; the same goes for codeine being turned into hydrocodone.[38]
The process gave rise to various concentrations of hydromorphone, dihydromorphine, hydromorphinol, and oxymorphone during the experiments. Three paths were found: from morphine to hydromorphone with dihydromorphine as the penultimate step, from morphine to hydromorphone with morphinone as the penultimate step, and from morphine to hydromorphinol to hydromorphone.
History
Hydromorphone was first synthesized and researched in Germany in 1924; Knoll introduced it to the mass market in 1926 under the brand name Dilaudid,[39] indicating its derivation and degree of similarity to morphine (by way of laudanum)—compare Dicodid (hydrocodone), Dihydrin (dihydrocodeine), and Dinarkon (oxycodone). The brand name Dilaudid is more widely known than the generic term hydromorphone and, because of this, Dilaudid is often used generically to mean any form of hydromorphone.
Society and culture
Recreational use
Like other opiates, hydromorphone can be used recreationally. Its reinforcing effects are mediated via its strong affinity for the μ-opioid receptor, inducing euphoria, sedation, reduced anxiety, respiratory depression, and other prototypical morphinian effects. Such effects make it particularly susceptible to abuse, although many patients using it for analgesia are able to use it for extended periods of time without developing drug-seeking behavior. In abusers, there can be a strong psychological dependence, thus creating an addiction with repeated use. Physical dependence causes withdrawal, while psychological dependence can create strong compulsions to use the drug, which can persist for days or weeks after the physical dependence is broken, and has been known to induce anxiety, insomnia, depression, and a range of other persistent mental illnesses. For this reason, psychotherapy is often included in detox programs, sometimes augmented with pharmacological therapies. Hydromorphone is more expensive on the illicit market than heroin, despite producing similar effects, thus causing the abuse rates of hydromorphone to be lower than heroin and similar opioids in many areas.
Names
Hydromorphone is known in various countries around the world by the brand names Hydal, Dimorphone, Sophidone LP, Dilaudid, Hydrostat, Hydromorfan, Hydromorphan, Hymorphan, Laudicon, Opidol, Palladone, Hydromorph Contin and others. An extended-release version of hydromorphone called Palladone was available for a short time in the United States before being voluntarily withdrawn from the market after a July 2005 FDA advisory warned of a high overdose potential when taken with alcohol.[40] As of March 2010, it is still available in the United Kingdom under the brand name Palladone SR, Nepal under the brand name Opidol, and in most other European countries.
There is an extended-release (once-daily) version of Hydromorphone available (in the United States).[28][41]
Detection
Hydromorphone is most commonly detected via blood and urine testing. Hydromorphone is usually detectable via blood screen for up to 24 hours and via urine screen from 3 to 8 days. Urine screen depends on several factors such as age, frequency of use, weight and duration of use. Extremes: a 20-year-old patient with a normal BMI, who is administered a small dosage would screen positive for up to 3 days in 95% of tests. Conversely, people who are >35 years of age and have been administered a heavy dosage with an overweight to obese BMI tend to test positive up to 7 to 8 days in 85% of cases.
Legal status
In the United States, the main drug control agency, the Drug Enforcement Administration, reports an increase in annual aggregate production quotas of hydromorphone from 766 kilograms in 1998 to 3,300 kilograms in 2006, and an increase in prescriptions in this time of 289%, from about 470,000 to 1,830,000. The 2013 production quota was 5968.75 kilograms.[42]
Like all opioids used for analgesia, hydromorphone is potentially habit-forming and is listed in Schedule II of the United States' Controlled Substances Act of 1970 as well as in similar levels under the drugs laws of practically all other countries and is listed in the Single Convention On Narcotic Drugs. The DEA ACSCN for hydromorphone is 9150.
Hydromorphone is listed under the German Betäubungsmittelgesetz as a Suchtgift in the most restricted schedule for medicinal drugs; it is similarly controlled in Austria under the SMG and the Swiss BetmG. The Misuse of Drugs Act 1971 (UK) and its French, Canadian, Australian, Italian, Czech, Croatian, Slovenian, Swedish, Polish, Spanish, Greek, Russian, and other laws similarly control it, as do virtually all other countries.
Use in executions
In 2009, Ohio approved the use of an intramuscular injection of 500 mg of hydromorphone and a supratherapeutic dose of midazolam as a backup means of carrying out executions when a suitable vein cannot be found for intravenous injection.[43]
Hydromorphone and midazolam was injected intravenously to execute double-murderer Joseph Wood in Arizona on July 24, 2014. Wood was heavily sedated (Stage 3 "Surgical anasthesia") within 4 minutes from start but took almost two hours to transition to stage 4 (cessation of respiration) and death.[44]
See also
- 6-MDDM—substitution derivative of hydromorphone's 6-ketone for 6-methylene that is extremely potent and of high efficacy
- Acetylmorphone—an acetyl ester of hydromorphone
- Chronic pain
- Dihydromorphine
- Dose dumping
- Hydrocodone—a hepatic prodrug of hydromorphone
- Hydromorphinol
- Morphine
- Opioids
- Oxymorphol—a metabolite of oxymorphone and an intermediate in the creation of hydromorphone
- Oxymorphone
- Patient-controlled analgesia
- Recreational drug use
References
- ↑ Coda BA, Rudy AC, Archer SM, Wermeling DP (July 2003). "Pharmacokinetics and bioavailability of single-dose intranasal hydromorphone hydrochloride in healthy volunteers". Anesth. Analg. 97 (1): 117–23, table of contents. PMID 12818953. doi:10.1213/01.ANE.0000066311.40978.4F.
- ↑ Vallner JJ, Stewart JT, Kotzan JA, Kirsten EB, Honigberg IL (April 1981). "Pharmacokinetics and bioavailability of hydromorphone following intravenous and oral administration to human subjects". J Clin Pharmacol. 21 (4): 152–6. PMID 6165742. doi:10.1002/j.1552-4604.1981.tb05693.x.
- ↑ http://www.drugs.com/pro/hydromorphone.html
- ↑ Hydromorphone Hydrochloride; MSDS No. 71681; Purdue Pharma L.P.: Stamford, CT, October 13, 2009. http://www.purduepharma.com/msdss/Dilaudid_2_4_8mgTablets_OralLiquid_MSDS.pdf (accessed November 5, 2015)
- 1 2 Hydromorphone Monograph (Side Effects & Drug Interactions)
- ↑ "Drug interactions between Dilaudid and Valium". Retrieved 19 November 2014.
- 1 2 "Dilaudid (hydromorphone hydrochloride) Oral LiquidDilaudid (hydromorphone hydrochloride) Tablets". app.purduepharma.com. Retrieved 2015-11-05.
- ↑ Cohen, MR (June 1992). "Doctor was thinking of the wrong drug". Nursing. 22 (6): 25. PMID 1377371.
- ↑ Tuohy, N; Paparella, S (December 2005). "Look-alike and sound-alike drugs: errors just waiting to happen". J Emerg Nurs. 31 (6): 569–71. PMID 16308048. doi:10.1016/j.jen.2005.07.012.
- ↑ Palladone Pain Drug Pulled Off the Market.
- ↑ Brennan, MJ (2013). "The effect of opioid therapy on endocrine function". The American Journal of Medicine. 126 (3 Suppl 1): S12–8. PMID 23414717. doi:10.1016/j.amjmed.2012.12.001.
- 1 2 Thwaites, D; McCann, S; Broderick, P (Aug 2004). "Hydromorphone neuroexcitation.". Journal of palliative medicine. 7 (4): 545–50. PMID 15353098. doi:10.1089/1096621041838362.
- ↑ Gagnon, DJ; Jwo, K (2013). "Tremors and agitation following low-dose intravenous hydromorphone administration in a patient with kidney dysfunction". Annals of Pharmacotherapy. 47 (7-8): e34. PMID 23715067. doi:10.1345/aph.1R784.
- ↑ Rapp, SE; Egan, KJ; Ross, BK; et al. (May 1996). "A multidimensional comparison of morphine and hydromorphone patient-controlled analgesia.". Anesth Analg. 82 (5): 1043–8. PMID 8610865. doi:10.1213/00000539-199605000-00029.
- 1 2 3 4 5 "Hydromorphone / Dilaudid Detox". Rapid Drug Detox. Retrieved 2015-11-05.
- 1 2 "Dilaudid Abuse & Addiction Withdrawals, Signs, Symptoms & Effects - Acadiana Addiction Center". www.acadianaaddiction.com. Retrieved 2015-11-05.
- 1 2 "Hydromorphone Drug Information". Narconon International. Retrieved 2015-11-05.
- ↑ "Withdrawal Syndromes: Practice Essentials, Background, Pathophysiology".
- ↑ "DILAUDID® ORAL LIQUID and DILAUDID® TABLETS Package Insert" (PDF). FDA. 2007. Retrieved November 5, 2015.
- ↑ "Opiod withdrawal protocol" (PDF). www.saskatoonhealthregion.ca. Retrieved 2015-11-05.
- 1 2 Treatment, Center for Substance Abuse (2004-01-01). "4 Treatment Protocols".
- ↑ Bell CC (1983). "Simultaneous treatment of hypertension and opiate withdrawal using an alpha 2 adrenergic agonist" (PDF). J Natl Med Assoc. 75: 89–93. PMC 2561435
 . PMID 6131140.
. PMID 6131140. - ↑ "DILAUDID® ORAL LIQUID and DILAUDID® TABLETS Package Insert" (PDF). FDA. 2007. Retrieved November 5, 2015.
- ↑ Nersesyan, Hrachya; Slavin, Konstantin V (2007-06-01). "Current aproach [sic] to cancer pain management: Availability and implications of different treatment options". Therapeutics and Clinical Risk Management. 3 (3): 381–400. ISSN 1176-6336. PMC 2386360
 . PMID 18488078.
. PMID 18488078. - 1 2 Sarhill, Nabeel; Walsh, Declan; Nelson, Kristine A. (2014-02-09). "Hydromorphone: pharmacology and clinical applications in cancer patients". Supportive Care in Cancer. 9 (2): 84–96. ISSN 0941-4355. doi:10.1007/s005200000183.
- ↑ Knight, Karen H. (Feb 2007). "Implantable Intrathecal Pumps for Chronic Pain: Highlights and Updates" (PDF). Croatian Medical Journal. 48: 22–34. PMC 2080496
 . PMID 17309136. Retrieved 2015-03-19.
. PMID 17309136. Retrieved 2015-03-19. - ↑ "EXALGO (hydromorphone hydrochloride) extended release tablets Package Insert" (PDF). FDA. 2010. Retrieved November 5, 2015.
- 1 2 Exalgo | Zalicus
- ↑ EXALGO safety profile
- ↑ Opioid Conversion Guidelines
- ↑ Switching Opioids
- ↑ "Hydromorphone". That's Poppycock!. 19 Feb 2009.
- ↑ Dilaudid Clinical Pharmacology
- ↑ Gregory, Thomas B. "Hydromorphone: Evolving to Meet the Challenges of Today’s Health Care Environment". Clinical Therapeutics. 35 (12): 2007–2027. doi:10.1016/j.clinthera.2013.09.027.
- ↑ http://www.painweek.org/../292-50.pdf
- ↑ Buck, Marcia (July 2008). "Use of Hydromorphone in Children and Adolescents" (PDF). University of Virginia Children's Hospital. Retrieved November 5, 2015.
- ↑ PHA 4220 - Neurology Pharmacotherapeutics Archived July 16, 2007, at the Wayback Machine.
- ↑ Long, MT; Hailes, AM; Kirby, GW; Bruce, NC (October 1995). "Transformations of morphine alkaloids by Pseudomonas putida M10". Appl. Environ. Microbiol. 61 (10): 3645–9. PMC 167664
 . PMID 7487001.
. PMID 7487001. - ↑ Felden, L; Walter, C; Harder, S; et al. (22 September 2011). "Comparative Clinical Effects of Hydromorphone and Morphine". British Journal of Anaesthesia. 107 (3): 319–328. PMID 21841049. doi:10.1093/bja/aer232. Retrieved 10 March 2012.
- ↑ "Information for Healthcare Professionals: Hydromorphone Hydrochloride Extended-Release Capsules (marketed as Palladone)". Center for Drug Evaluation and Research. 2005-07-15. Retrieved 2016-08-16.
- ↑ EXALGO safety profile
- ↑ "Proposed Adjustments to the Aggregate Production Quotas for Schedule I and II Controlled Substances and Assessment of Annual Needs for the List I Chemicals Ephedrine, Pseudoephedrine, and Phenylpropanolamine for 2013". Drug Enforcement Administration (DEA), Department of Justice. 20 June 2014. Retrieved 2014-07-26.
- ↑ "Ohio Prisons Director Announces Changes to Ohio’s Execution Process". Ohio Department of Rehabilitation and Correction. November 13, 2009. Retrieved 2014-01-17.
- ↑ "Arizona execution takes two hours". BBC News. July 24, 2014. Retrieved 2014-07-24.
External links
- Hydromorphone consumer drug information Drugs.com.
- Exalgo: full prescribing information
- Article discussing withdrawal of extended-release hydromorphone from the U.S. market
- painCare.ca and Patient Information about Opioid Analgesics (access restricted to professionals)
- Dihydromorphinones from morphine & analogues
- United States DEA's perspective, including statistics on manufacture and prescription levels from 1998 to 2006
- "When is a pain doctor a drug pusher?", The New York Times, 6-17-2007