Paget's disease of bone
| Paget's disease of bone | |
|---|---|
| Synonyms | osteitis deformans, Paget's disease |
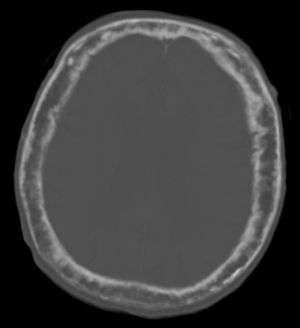 | |
| "This 92 year-old male patient presented for assessment of sudden inability to move half his body. An incidental finding was marked thickening of the calvarium. The diploic space is widened and there are ill-defined sclerotic and lucent areas throughout. The cortex is thickened and irregular. The findings probably correspond to the “cotton wool spots” seen on plain films in the later stages of Paget’s disease." | |
| Pronunciation |
|
| Classification and external resources | |
| Specialty | rheumatology |
| ICD-10 | M88 |
| ICD-9-CM | 731.0 |
| OMIM | 602080 |
| DiseasesDB | 9479 |
| MedlinePlus | 000414 |
| eMedicine | med/2998 radio/514 pmr/98 |
| Patient UK | Paget's disease of bone |
| MeSH | D010001 |
Paget's disease of bone (also termed osteitis deformans or ambiguously, just Paget's disease) is caused by the excessive breakdown and formation of bone, followed by disorganised bone remodelling. This causes affected bone to weaken, resulting in pain, misshapen bones, fractures and arthritis in the joints near the affected bones. Rarely, it can develop into a primary bone cancer known as Paget's sarcoma. Often Paget's disease is localised to only a few bones in the body. The pelvis, femur, and lower lumbar vertebrae are the most commonly affected bones. Paget's disease typically is localised, affecting just one or a few bones, as opposed to osteoporosis, for example, which usually affects all the bones in the body.
A later phase of the disease is characterised by the replacement of normal bone marrow with highly vascular fibrous tissue.[1] Because early diagnosis and treatment is important, after age 40, siblings and children of someone with Paget's disease should have an alkaline phosphatase blood test every two or three years. If the alkaline phosphatase level is above normal, other tests such as a bone-specific alkaline phosphatase test, bone scan, or X-ray can be performed.
Decisions about treating Paget's disease may be complicated as the disease often affects people differently. In addition to this, it is sometimes difficult to predict whether a person with Paget's disease, who shows no signs or symptoms of the disorder, will develop symptoms or complications (such as a bone fracture) in the future. Although there is no cure for Paget's disease, medications (bisphosphonates and calcitonin) can help control the disorder and lessen pain and other symptoms. Medications are often successful in controlling the disorder, especially when started before complications begin.
Paget's disease affects from 1.5 to 8.0 percent of the population, depending on age and country of residence. Paget's disease is rare in people less than 55 years of age.[2] Men are more commonly affected than women (3:2).[3] The disease is named after Sir James Paget.
Signs and symptoms

Many people with Paget's disease do not know they have the disease, because they have a mild case with no symptoms. In addition, when symptoms do occur, they may be confused with those of arthritis or other disorders. In other cases, the diagnosis is made only after complications have developed. About 35 percent of patients with Paget's have symptoms related to the disease when they are first diagnosed.[2]
The first manifestation of Paget's disease is usually an elevated alkaline phosphatase in the blood.[2] Overall, the most common symptom is bone pain.[2]
Loss of hearing in one or both ears may occur when Paget's disease affects the skull[2] and the bone that surrounds the inner ear. Treating the disease may slow or stop hearing loss. In rare cases, involvement of the skull may lead to compression of the nerves that supply the eye, leading to vision loss. Paget's may also cause gross deformities in the bones.[2]
Associated conditions
Paget's disease is a frequent component of multisystem proteinopathy. Paget's disease may lead to other medical conditions, including:
- Arthritis may be caused by bowing of long bones in the leg, distorting alignment and increasing pressure on nearby joints. In addition, pagetic bone may enlarge, causing joint surfaces to undergo excessive wear. In these cases, pain may be due to a combination of Paget's disease and osteoarthritis.
- Cardiovascular disease can result from severe Paget's disease (i.e. with more than 40% skeletal involvement). Arteriovenous connections can often form in the bone, and so the heart has to work harder (pump more blood) to ensure adequate oxygen supply to the tissues. This increase in cardiac output can lead to calcification of the aortic valve, and the resulting aortic stenosis causes left ventricular hypertrophy and eventually high-output congestive failure.
- Kidney stones are somewhat more common in patients with Paget's disease.
- Nervous system problems may occur in Paget's disease, resulting from increased pressure on the brain, spinal cord, or nerves, and reduced blood flow to the brain and spinal cord.
- When Paget's disease affects the facial bones, the teeth may become loose. Disturbance in chewing may occur.
- Angioid streaks may develop, possibly as a result of calcification of collagen or other pathological deposition.
Paget's disease is not associated with osteoporosis. Although Paget's disease and osteoporosis can occur in the same patient, they are different disorders. Despite their marked differences, several treatments for Paget's disease are also used to treat osteoporosis.
Causes
Viral
Paget's disease may be caused by a slow virus infection (i.e., paramyxoviridae) present for many years before symptoms appear. Associated viral infections include respiratory syncytial virus,[5] canine distemper virus,[6][7] and the measles virus.[8][9] However, recent evidence has cast some doubt upon the measles association.[10] Laboratory contamination may have played a role in past studies linking paramyxovirus (e.g. measles) to Paget's disease.[11]
Genetic
There is a hereditary factor in the development of Paget's disease of bone.[12][13] Two genes, SQSTM1 and RANK, and specific regions of chromosome 5 and 6 are associated with Paget's disease of bone. Genetic causes may or may not involve a family history of Paget's disease.
About 40–50% of people with the inherited version of Paget's disease have a mutation in the gene SQSTM1, which encodes a protein, called p62, that is involved in regulating the function of osteoclasts (bone cells).[2] However, about 10-15 percent of people that develop the disease without any family history also have a mutation in the SQSTM1 gene.[2]
Paget's disease of bone is associated with mutations in RANK. Receptor Activator of Nuclear Factor κ B (RANK), which is a type I membrane protein that is expressed on the surface of osteoclasts and is involved in their activation upon ligand binding[14] Additional genetic associations include:
| Name | OMIM | Locus | Gene |
|---|---|---|---|
| PDB1 | 167250 | 6p | ? |
| PDB2 | 18q22.1 | RANK | |
| PDB3 | 5q35 | SQSTM1 | |
| PDB4 | 606263 | 5q31[15] | ? |
Environmental factor
Studies showed that air pollution may play an important role in the pathogenesis of Paget's disease of bone.[16]
Pathogenesis
The pathogenesis of Paget's disease is described in 4 stages[17]
- Osteoclastic activity
- Mixed osteoclastic – osteoblastic activity
- Osteoblastic activity
- Malignant degeneration
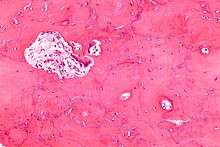
Initially, there is a marked increase in the rate of bone resorption in localized areas, caused by large and numerous osteoclasts. These localized areas of pathological destruction of bone tissue (osteolysis) are seen radiologically as an advancing lytic wedge in long bones or the skull. When this occurs in the skull, it is called osteoporosis circumscripta. The osteolysis is followed by a compensatory increase in bone formation induced by the bone forming cells, called osteoblasts, that are recruited to the area. This is associated with accelerated deposition of lamellar bone in a disorganized fashion. This intense cellular activity produces a chaotic picture of trabecular bone ("mosaic" pattern), rather than the normal linear lamellar pattern. The resorbed bone is replaced and the marrow spaces are filled by an excess of fibrous connective tissue with a marked increase in blood vessels, causing the bone to become hypervascular. The bone hypercellularity may then diminish, leaving a dense "pagetic bone", also known as burned-out Paget's disease.
Sir James Paget first suggested the disease was due to an inflammatory process. Some evidence suggests that a paramyxovirus infection is the underlying cause of Paget's disease,[2] which may support the possible role of inflammation in the pathogenesis. However, no infectious virus has yet been isolated as a causative agent, and other evidence suggests an intrinsic hyperresponsive reaction to vitamin D and RANK ligand is the cause. Further research is therefore necessary.[18]
Diagnosis


Paget's disease may be diagnosed using one or more of the following tests:
- Pagetic bone has a characteristic appearance on X-rays. A skeletal survey is therefore indicated.
- An elevated level of alkaline phosphatase in the blood in combination with normal calcium, phosphate, and aminotransferase levels in an elderly patient are suggestive of Paget's disease.
- Markers of bone turnover in urine eg. Pyridinoline
- Elevated levels of serum and urinary hydroxyproline are also found.
- Bone scans are useful in determining the extent and activity of the condition. If a bone scan suggests Paget's disease, the affected bone(s) should be X-rayed to confirm the diagnosis.
| Condition | Calcium | Phosphate | Alkaline phosphatase | Parathyroid hormone | Comments |
|---|---|---|---|---|---|
| Osteopenia | unaffected | unaffected | normal | unaffected | decreased bone mass |
| Osteopetrosis | unaffected | unaffected | elevated | unaffected | thick dense bones also known as marble bone |
| Osteomalacia and rickets | decreased | decreased | elevated | elevated | soft bones |
| Osteitis fibrosa cystica | elevated | decreased | elevated | elevated | brown tumors |
| Paget's disease of bone | unaffected | unaffected | variable (depending on stage of disease) | unaffected | abnormal bone architecture |
Treatment
Although initially diagnosed by a primary care physician, Endocrinologists (internal medicine physicians who specialize in hormonal and metabolic disorders), rheumatologists (internal medicine physicians who specialize in joint and muscle disorders), orthopedic surgeons, neurosurgeons, neurologists, oral and maxillofacial surgeons, podiatrists, and otolaryngologists are generally knowledgeable about treating Paget's disease, and may be called upon to evaluate specialized symptoms.
Medication
The goal of treatment is to relieve bone pain and prevent the progression of the disease. These medications are usually recommended for people with Paget's disease who:
- have bone pain, headache, back pain, or a nerve-related symptom (such as "shooting" pains in the leg) that is directly associated with the disease;
- have elevated levels of serum alkaline phosphatase (ALP) in their blood;
- display evidence that a bone fracture will occur;
- require pretreatment therapy for affected bones that require surgery;
- have active symptoms in the skull, long bones, or vertebrae (spine);
- have the disease in bones located next to major joints, placing them at risk of developing osteoarthritis;
- develop hypercalcemia that occurs when a person with several bones affected by Paget's disease and a high serum alkaline phosphatase level is immobilized.
Bisphosphonates
Five bisphosphonates are currently available. In general, the most commonly prescribed are risedronic acid, alendronic acid , and pamidronic acid. Etidronic acid and other bisphosphonates may be appropriate therapies for selected patients but are less commonly used. None of these drugs should be used by people with severe kidney disease.
- Etidronate disodium The approved regimen is once daily for six months; a higher dose is more commonly used. No food, beverage, or medications should be consumed for two hours before and after taking. The course should not exceed six months, but repeat courses can be given after rest periods, preferably of three to six months duration.
- Pamidronate disodium in intravenous form: the approved regimen uses an infusion over four hours on each of three consecutive days, but a more commonly used regimen is over two to four hours for two or more consecutive or nonconsecutive days.
- Alendronate sodium is given as tablets once daily for six months; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
- Tiludronate disodium are taken once daily for three months; they may be taken any time of day, as long as there is a period of two hours before and after resuming food, beverages, and medications.
- Risedronate sodium tablet taken once daily for 2 months is the prescribed regimen; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
- Zoledronic acid is given as an intravenous infusion; a single dose is effective for two years. This is recommended for most people at high risk with active disease.[19]
Calcitonin
Calcitonin, also called calcitonin-salmon, is a synthetic copy of a polypeptide hormone secreted by the ultimobranchial gland of salmon. Miacalcin is administered by injection, three times per week or daily, for 6–18 months. Repeat courses can be given after brief rest periods. Miacalcin may be appropriate for certain patients, but is seldom used. Calcitonin is also linked to increased chance of cancer. Due to the increased risk of cancer, the European Medicines Agency (EMA) recommended that calcitonin be used only on a short-term basis for 3 conditions for which it had previously been approved in the European Union: Paget's disease, acute bone loss resulting from sudden immobilization, and hypercalcemia caused by cancer.
The EMA said it based its recommendations on a review of the benefits and risks of calcitonin-containing medicines. Conducted by the agency's Committee for Medicinal Products for Human Use (CHMP), the review encompassed available data from the companies that market these drugs, postmarketing safety data, randomized controlled studies, 2 studies of unlicensed oral calcitonin drugs, and experimental cancer studies, among other sources.
CHMP found that "a higher proportion of patients treated with calcitonin for long periods of time develop cancer of various types, compared with patients taking placebo." The increase in cancer rates ranged from 0.7% for oral formulations to 2.4% for the nasal formulation. CHMP concluded that the benefits of calcitonin for osteoporosis did not exceed the risks. The nasal spray's only indication is for osteoporosis, thus justifying the drug's removal from the market.
As a solution for injection or infusion, calcitonin should be administered for no more than 4 weeks to prevent acute bone loss resulting from sudden immobilization, and normally for no more than 3 months to treat Paget's disease, the EMA said. The agency did not specify a time frame for the short-term use of calcitonin for treating hypercalcemia caused by cancer.
Surgery
Medical therapy prior to surgery helps to decrease bleeding and other complications. Patients who are having surgery should discuss treatment with their physician. There are generally three major complications of Paget's disease for which surgery may be recommended.
- Fractures — Surgery may allow fractures to heal in a better position.
- Severe degenerative arthritis — If disability is severe and medication and physical therapy are no longer helpful, joint replacement of the hips and knees may be considered.
- Bone deformity — Cutting and realignment of pagetic bone (osteotomy) may help painful weight bearing joints, especially the knees.
Complications resulting from enlargement of the skull or spine may injure the nervous system. However, most neurologic symptoms, even those that are moderately severe, can be treated with medication and do not require neurosurgery.
Diet and exercise
In general, patients with Paget's disease should receive 1000–1500 mg of calcium, adequate sunshine, and at least 400 units of vitamin D daily. This is especially important in patients being treated with bisphosphonates; however, taking oral bisphosphonates should be separated from taking calcium by at least two hours, because the calcium can inhibit the absorption of the bisphosphonate. Patients with a history of kidney stones should discuss calcium and vitamin D intake with their physicians.
Exercise is very important in maintaining skeletal health, avoiding weight gain, and maintaining joint mobility. Since undue stress on affected bones should be avoided, patients should discuss any exercise program with their physicians or physical therapists before beginning.
Prognosis
The outlook is generally good, particularly if treatment is given before major changes in the affected bones have occurred. Any bone or bones can be affected, but Paget's disease occurs most frequently in the spine, skull, pelvis, femur, and lower legs. In general, symptoms progress slowly, and the disease does not spread to normal bones. Treatment can control Paget's disease and lessen symptoms, but is not a cure.
Osteogenic sarcoma, a form of bone cancer, is a rare adult-onset complication of Paget's disease that mainly occurs in children and adolescents between the ages of 10 and 19 years who do not have Paget's disease. The development of osteosarcoma may be suggested by the sudden onset or worsening of pain, and it occurs in less than one percent of patients with Paget's disease.
Epidemiology
The overall prevalence and severity of Paget's disease are decreasing; the cause for these changes is unclear.[20] Paget's disease is rare in people less than 55 years of age,[2] and the prevalence increases with age.[20] Evidence from studies of autopsy results have demonstrated Paget's disease in about 3 percent of people older than 40 years of age.[20] Paget's disease is more common in males than females.[3] Rates of Paget's disease are about 50 percent higher in men than in women.
About 15 percent of people with Paget's disease also have a family member with the disease.[2] In cases where the disease is familial, it is inherited in an autosomal dominant fashion, although not all people that inherit the affected version of the genes will express the disease (incomplete penetrance).[2]
The incidence of Paget's disease varies considerably with geographic location.[20] Paget's predominantly affects people of European descent, whereas people of African, Asian, or Indian descent are less commonly affected.[2] Paget's disease is less common in Switzerland and Scandinavia than in the rest of Western Europe.[20] Paget's disease is uncommon in the native populations of North and South America, Africa, Asia, and the Middle East. When an individual from these regions does develop Paget's disease, there is typically some European ancestry present.
Etymology
Paget's disease of bone was originally termed osteitis deformans, because it was thought to involve an inflammatory process, which is implied by the suffix -itis. Now, that term is considered technically incorrect, and the preferred term is osteodystrophia deformans.[21]
Society and culture
- C.S.I.: NY: A murder victim in Season 2 episode "Youngblood" was afflicted with Paget's disease.
- Retired Boston Red Sox center fielder Dom DiMaggio suffered from Paget's disease and served as a member of the board of directors of the Paget Foundation.[22]
- Egill Skallagrímsson, the main character in Egils Saga, may have suffered from this disease.
- The X-Files: Fox Mulder's mother commits suicide in Season 7, Episode 10 "Sein und Zeit", after being diagnosed with Paget's disease.
References
- ↑ Tamparo, Carol; Lewis, Marcia (2011). Diseases of the Human Body. Philadelphia, PA: F.A. Davis Company. p. 221. ISBN 9780803625051.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Ralston, Stuart H. (Feb 14, 2013). "Paget's Disease of Bone". New England Journal of Medicine. 368 (7): 644–650. PMID 23406029. doi:10.1056/NEJMcp1204713.
- 1 2 Kumar and Clark, Parveen and Micheal (2009). Welcome to Kumar and Clark's Clinical Medicine 7E. Elsiver. p. 565. ISBN 978-0-7020-2993-6.
- ↑ Brown, Mark (2008-10-11). "Solved: mystery of The Ugly Duchess - and the Da Vinci connection". The Guardian. Retrieved 2012-04-30.
- ↑ Mills BG, Singer FR, Weiner LP, Holst PA (February 1981). "Immunohistological demonstration of respiratory syncytial virus antigens in Paget disease of bone". Proc. Natl. Acad. Sci. U.S.A. 78 (2): 1209–13. PMC 319977
 . PMID 6940136. doi:10.1073/pnas.78.2.1209.
. PMID 6940136. doi:10.1073/pnas.78.2.1209. - ↑ Hoyland JA, Dixon JA, Berry JL, Davies M, Selby PL, Mee AP (May 2003). "A comparison of in situ hybridisation, reverse transcriptase-polymerase chain reaction (RT-PCR) and in situ-RT-PCR for the detection of canine distemper virus RNA in Paget disease". J. Virol. Methods. 109 (2): 253–9. PMID 12711070. doi:10.1016/S0166-0934(03)00079-X.
- ↑ Gordon MT, Anderson DC, Sharpe PT (1991). "Canine distemper virus localised in bone cells of patients with Paget disease". Bone. 12 (3): 195–201. PMID 1910961. doi:10.1016/8756-3282(91)90042-H.
- ↑ Friedrichs WE, Reddy SV, Bruder JM, et al. (January 2002). "Sequence analysis of measles virus nucleocapsid transcripts in patients with Paget's disease". J. Bone Miner. Res. 17 (1): 145–51. PMID 11771661. doi:10.1359/jbmr.2002.17.1.145.
- ↑ Baslé MF, Fournier JG, Rozenblatt S, Rebel A, Bouteille M (May 1986). "Measles virus RNA detected in Paget disease bone tissue by in situ hybridization". J. Gen. Virol. 67 (5): 907–13. PMID 3701300. doi:10.1099/0022-1317-67-5-907.
- ↑ Matthews BG, Afzal MA, Minor PD, et al. (April 2008). "Failure to detect measles virus ribonucleic acid in bone cells from patients with Paget's disease". J. Clin. Endocrinol. Metab. 93 (4): 1398–401. PMID 18230662. doi:10.1210/jc.2007-1978.
- ↑ Ralston SH, Afzal MA, Helfrich MH, et al. (April 2007). "Multicenter blinded analysis of RT-PCR detection methods for paramyxoviruses in relation to Paget disease of bone". J. Bone Miner. Res. 22 (4): 569–77. PMID 17227218. doi:10.1359/jbmr.070103.
- ↑ Ralston SH, Langston AL, Reid IR (July 2008). "Pathogenesis and management of Paget disease of bone". Lancet. 372 (9633): 155–63. PMID 18620951. doi:10.1016/S0140-6736(08)61035-1.
- ↑ Whyte MP (2006). "Paget's disease of bone and genetic disorders of RANKL/OPG/RANK/NF-kappaB signaling". Annals of the New York Academy of Sciences. 1068: 143–64. PMID 16831914. doi:10.1196/annals.1346.016.
- ↑ Haslam SI, Van Hul W, Morales-Piga A, Balemans W, San-Millan JL, Nakatsuka K, Willems P, Haites NE, Ralston SH (1998). "Paget's disease of bone: evidence for a susceptibility locus on chromosome 18q and for genetic heterogeneity". Journal of Bone and Mineral Research. 13 (6): 911–7. PMID 9626621. doi:10.1359/jbmr.1998.13.6.911.
- ↑ Laurin N, Brown JP, Lemainque A, et al. (September 2001). "Paget Disease of Bone: Mapping of Two Loci at 5q35-qter and 5q31". Am. J. Hum. Genet. 69 (3): 528–43. PMC 1235483
 . PMID 11473345. doi:10.1086/322975.
. PMID 11473345. doi:10.1086/322975. - ↑ Numan MS, Brown JP, Michou L (2015). "Impact of air pollutants on oxidative stress in common autophagy-mediated aging diseases". International Journal of Environmental Research and Public Health. 12 (2): 2289–305. PMC 4344726
 . PMID 25690002. doi:10.3390/ijerph120202289.
. PMID 25690002. doi:10.3390/ijerph120202289. - ↑ Numan MS, Amiable N, Brown JP, Michou L (2015). "Paget's disease of bone: an osteoimmunological disorder?". Drug Design, Development and Therapy. 9: 4695–707. PMC 4544727
 . PMID 26316708. doi:10.2147/DDDT.S88845.
. PMID 26316708. doi:10.2147/DDDT.S88845. - ↑ Basic Pathology, Kumar Abbas Fausto Mitchell, Saunders Elsevier
- ↑ Singer FR, Bone HG, Hosking DJ, Lyles KW, Murad MH, Reid IR, Siris ES (2014). "Paget's disease of bone: an endocrine society clinical practice guideline". The Journal of Clinical Endocrinology and Metabolism. 99 (12): 4408–22. PMID 25406796. doi:10.1210/jc.2014-2910.
- 1 2 3 4 5 Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine:Chapter 355. Paget's Disease and Other Dysplasias of Bone (18th ed.). New York: McGraw-Hill. ISBN 007174889X.
- ↑ Rhodes B, Jawad AS (2005). "Paget's disease of bone: osteitis deformans or osteodystrophia deformans?". Rheumatology. 44 (2): 261–2; author reply 262. PMID 15637095. doi:10.1093/rheumatology/keh448.
- ↑ "Paid Notice: Deaths DIMAGGIO, DOMINIC P". The New York Times. May 10, 2009.
Further reading
- Singer, FR; Bone HG, 3rd; Hosking, DJ; Lyles, KW; Hassan Murad, M; Reid, IR; Siris, ES (19 November 2014). "Paget's Disease of Bone: An Endocrine Society Clinical Practice Guideline.". The Journal of Clinical Endocrinology and Metabolism. 99: jc20142910. PMID 25406796. doi:10.1210/jc.2014-2910.
External links
- The Paget's Association
- Paget's Disease of Bone Overview - NIH Osteoporosis and Related Bone Diseases ~ National Resource Center