Ovarian torsion
| Ovarian torsion | |
|---|---|
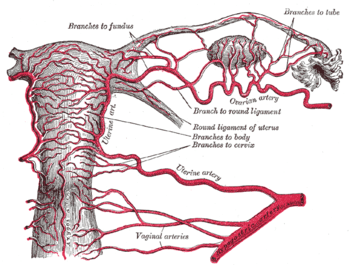 | |
| Arteries of the female reproductive tract: uterine artery, ovarian artery and vaginal arteries. (Ovary and ovarian artery visible in upper right.) |
Ovarian torsion (OT) is the rotation of the ovary at its pedicle to such a degree as to occlude the ovarian artery and/or vein.
Signs and symptoms
Patients with ovarian torsion often present with sudden onset of sharp and usually unilateral lower abdominal pain, in 70% of cases accompanied by nausea and vomiting.[1]
Pathophysiology
The development of an ovarian mass is related to the development of torsion. In the reproductive years, regular growth of large corpus luteal cysts are a risk factor for rotation. The mass effect of ovarian tumors is also a common cause of torsion. Torsion of the ovary usually occurs with torsion of the fallopian tube as well on their shared vascular pedicle around the broad ligament, although in rare cases the ovary rotates around the mesovarium or the fallopian tube rotates around the mesosalpinx. In 80%, torsion happens unilaterally, with slight predominance on the right.
Diagnosis
Ovarian torsion is difficult to diagnose accurately, and operation is often performed before certain diagnosis is made. A study at an obstetrics and gynaecology department found that preoperative diagnosis of ovarian torsion was confirmed in only 46% of people.[2]
Ultrasound
Gynecologic ultrasonography is the imaging modality of choice.[3] Use of doppler ultrasound in the diagnosis has been suggested.[4][5] However, doppler flow is not always absent in torsion – the definitive diagnosis is often made in the operating room.[6]
Lack of ovarian blood flow on doppler sonography seems to be a good predictor of ovarian torsion. Women with pathologically low flow are more likely to have OT (77% vs. 29% in a study).[2] The sensitivity and specificity of abnormal ovarian flow for OT are 44% and 92%, respectively, with a positive and negative predictive value of 78% and 71%, respectively.[2] Specific flow features on Doppler sonography include:[3]
- Little or no intra-ovarian venous flow. This is commonly seen in ovarian torsion.
- Absent arterial flow. This is a less common finding in ovarian torsion
- Absent or reversed diastolic flow
Normal vascularity does not exclude intermittent torsion. There may occasionally be normal Doppler flow because of the ovary's dual blood supply from both the ovarian arteries and uterine arteries.
Other ultrasonographic features include:[3]
- Enlarged hypoechogenic or hyperechogenic ovary
- Peripherally displaced ovarian follicles
- Free pelvic fluid. This may be seen in more than 80% of cases
- Whirlpool sign of twisted vascular pedicle
- Underlying ovarian lesion can often be found
- Uterus may be slightly deviated towards the torted ovary.
Treatment
Surgical treatment of ovarian torsion includes laparoscopy to uncoil the torsed ovary and possibly oophoropexy to fixate the ovary which is likely to twist again.[7] In severe cases, where blood flow is cut off to the ovary for an extended period of time, necrosis of the ovary can occur. In these cases the ovary must be surgically removed.[8][9]
Epidemiology
Ovarian torsion accounts for about 3% of gynecologic emergencies. The incidence of ovarian torsion among women of all ages is 5.9 per 100,000 women, and the incidence among women of reproductive age (15–45 years) is 9.9 per 100,000 women.[10] In 70% of cases, it is diagnosed in women between 20 and 39 years of age. The risk is greater during pregnancy and in menopause. Risk factors include increased length of the ovarian ligaments, pathologically enlarged ovaries (more than 6 cm), ovarian masses or cysts, and enlarged corpus luteum in pregnancy.
See also
- Testicular torsion – equivalent condition of the male reproductive system
References
- ↑ Ovarian Torsion at eMedicine
- 1 2 3 Bar-On, Shikma; Mashiach, Roy; Stockheim, David; Soriano, David; Goldenberg, Motti; Schiff, Eyal; Seidman, Daniel S. (2010). "Emergency laparoscopy for suspected ovarian torsion: are we too hasty to operate?". Fertility and Sterility. 93 (6): 2012–5. PMID 19159873. doi:10.1016/j.fertnstert.2008.12.022.
- 1 2 3 Weerakkody, Yuranga; Dixon, Andrew. "Ovarian torsion". Radiopaedia.
- ↑ Peña, Joseph E; Ufberg, David; Cooney, Nancy; Denis, André L (2000). "Usefulness of Doppler sonography in the diagnosis of ovarian torsion". Fertility and Sterility. 73 (5): 1047–50. PMID 10785237. doi:10.1016/S0015-0282(00)00487-8.
- ↑ Zanforlin Filho SM, Araujo Júnior E, Serafini P, et al. (April 2008). "Diagnosis of ovarian torsion by three-dimensional power Doppler in first trimester of pregnancy". J. Obstet. Gynaecol. Res. 34 (2): 266–70. PMID 18412795. doi:10.1111/j.1447-0756.2008.00768.x.
- ↑ Tintinalli, Judith (2004). Emergency Medicine. McGraw Hill Professional. p. 904. ISBN 978-0-07-138875-7.
- ↑ "oophoropexy". Repropedia.
- ↑ "Ovarian torsion: to pex or not to pex? case report and review of the literature". Journal of Pediatric and Adolescent Gynecology. 16: 381–384. doi:10.1016/j.jpag.2003.09.017.
- ↑ "Conservative management of bilateral asynchronous adnexal torsion with necrosis in a prepubescent girl". Journal of Pediatric Surgery. 35: 1248–1251. doi:10.1053/jpsu.2000.8764.
- ↑ Yuk, Jin-Sung; Kim, Log Young; Shin, Ji-Yeon; Choi, Do Young; Kim, Tae Yoon; Lee, Jung Hun (2015). "A national population-based study of the incidence of adnexal torsion in the Republic of Korea". International Journal of Gynecology & Obstetrics. 129 (2): 169–70. PMID 25721499. doi:10.1016/j.ijgo.2014.11.027.
External links
| Classification |
V · T · D |
|---|---|
| External resources |