Nortriptyline
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Allegron, Aventyl, Pamelor |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682620 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | High |
| Metabolism | Hepatic |
| Biological half-life | 16 and 90 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.000.717 |
| Chemical and physical data | |
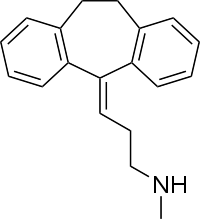
| Formula | C19H21N |
| Molar mass | 263.38 g/mol |
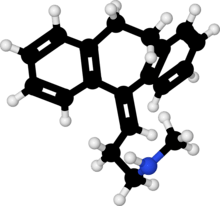
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Nortriptyline[note 1] is an antidepressant medication used to treat clinical depression. Chemically it is a secondary amine dibenzocycloheptene and pharmacologically it is classed as a second-generation tricyclic antidepressant (TCA). This is because it has less anticholinergic (like dry mouth, constipation, blurred vision, etc.), antihistaminergic (like drowsiness and weight gain), antiadrenergic (like a drop in blood pressure upon standing up) and cardiotoxic (heart-toxic, namely the capacity of these drugs to interfere with normal heart rhythm) effects than the older first-generation TCAs. Another licensed use for it is in the treatment of childhood bedwetting. Off-label uses include chronic pain and migraine and labile affect in some neurological disorders.[1]
It is the chief active metabolite of amitriptyline, a first-generation TCA. It is the N-desmethyl metabolite of amitriptyline. Like amitriptyline it works by inhibiting the reuptake of serotonin and norepinephrine into the synapse, thereby enhancing signalling via these neurotransmitters. It preferentially inhibits the reuptake of norepinephrine over serotonin, which is the opposite to amitriptyline.[1]
Medical uses
In the United Kingdom, it may also be used for treating nocturnal enuresis, with courses of treatment lasting no more than three months. It is also used off-label for the treatment of panic disorder, irritable bowel syndrome, migraine prophylaxis and chronic pain or neuralgia modification, particularly temporomandibular joint disorder.[2]
Neuropathic pain
Although not approved by the FDA for neuropathic pain, many randomized controlled trials have demonstrated the efficacy of tricyclic antidepressants for the treatment of this condition in both depressed and non-depressed individuals. Recently, an evidence-based guideline sponsored by the International Association for the Study of Pain recommends nortriptyline as a first-line medication for neuropathic pain.[3]
Side effects
The most common side effects include dry mouth, sedation, constipation, increased appetite, blurred vision and tinnitus.[1][4] An occasional side effect is a rapid or irregular heartbeat. Alcohol may exacerbate some of its side effects.[1]
Warnings
Closer monitoring is required for those with a history of cardiovascular disease, stroke, glaucoma, or seizures, as well as in persons with hyperthyroidism or receiving thyroid hormones.
Excessive consumption of alcohol in combination with nortriptyline therapy may have a potentiating effect, which may lead to the danger of increased suicidal attempts or overdosage, especially in patients with histories of emotional disturbances or suicidal ideation.
Contraindications
Nortriptyline should not be used in the acute recovery phase after myocardial infarction (viz, heart attack). Unlike the TCAs clomipramine and imipramine, concurrent use of nortriptyline with MAO inhibitors is safe within recommended dosage ranges.
Overdose
The symptoms and the treatment of an overdose are generally the same as for the other tricyclic antidepressants, including serotonin syndrome and adverse cardiac effects. Because tricyclic antidepressants have a relatively narrow therapeutic index, the likelihood of serious overdose (both accidental and intentional) is fairly high. A nortriptyline overdose is considered a medical emergency and frequently results in death.
Pharmacogenetics
Nortriptyline is metabolized in the liver by the hepatic enzyme CYP2D6, and genetic variations within the gene coding for this enzyme can affect its metabolism, leading to changes in the concentrations of the drug in the body.[5] Increased concentrations of nortriptyline may increase the risk for side effects, including anticholinergic and nervous system adverse effects, while decreased concentrations may reduce the drug's efficacy.[6][7][8]
Individuals can be categorized into different types of CYP2D6 metabolizers depending on which genetic variations they carry. These metabolizer types include poor, intermediate, extensive, and ultrarapid metabolizers. Most individuals (about 77-92%) are extensive metabolizers,[8] and have "normal" metabolism of nortriptyline. Poor and intermediate metabolizers have reduced metabolism of the drug as compared to extensive metabolizers; patients with these metabolizer types may have an increased probability of experiencing side effects. Ultrarapid metabolizers use nortriptyline much faster than extensive metabolizers; patients with this metabolizer type may have a greater chance of experiencing pharmacological failure.[6][7][8]
The Clinical Pharmacogenetics Implementation Consortium recommends avoiding nortriptyline in persons who are CYP2D6 ultrarapid or poor metabolizers, due to the risk of a lack of efficacy and side effects, respectively. A reduction in starting dose is recommended for patients who are CYP2D6 intermediate metabolizers. If use of nortriptyline is warranted, therapeutic drug monitoring is recommended to guide dose adjustments.[8] The Dutch Pharmacogenetics Working Group recommends reducing the dose of nortriptyline in CYP2D6 poor or intermediate metabolizers, and selecting an alternative drug or increasing the dose in ultrarapid metabolizers.[9]
Pharmacology
Nortriptyline is an active metabolite of amitriptyline by demethylation in the liver. Its pharmacologic profile is as follows:[10][11]
| Receptor/Transporter Protein | Binding Affinity (Ki[nM]) | Receptor location and species |
|---|---|---|
| SERT | 16.5 | Human, cloned |
| NET | 4.37 | Human, cloned |
| DAT | 3100 | Human, cloned |
| 5-HT1A | 294 | Human, brain |
| 5-HT2A | 5 | Rat, cloned |
| 5-HT2C | 8.5 | Rat, cloned |
| 5-HT6 | 148 | Rat, cloned |
| α1 | 55 | Human, brain |
| α2 | 2030 | Human, brain |
| β | >10000 | Mammalian, brain |
| M1 | 40 | Human, cloned |
| M2 | 110 | Human, cloned |
| M3 | 50 | Human, cloned |
| M4 | 84 | Human, cloned |
| M5 | 97 | Human, cloned |
| D2 | 2570 | Human, brain |
| H1 | 15.1 | Human, cloned |
| Sigma receptor | 2000 | Guinea pig, brain |
These effects account for some therapeutic actions as well as for most side effects such as sedation, hypotension, anticholinergic effects, etc. Nortriptyline may also have a sleep-improving effect due to its affinity for 5HT2A and histaminergic receptors.[12] In the short term; however, nortriptyline may disturb sleep due to its activating effect.
Like other tricyclic antidepressants, nortriptyline also blocks sodium channels, possibly accounting in part for its analgesic action.
In one study of long-term efficacy, nortriptyline showed a higher relapse rate in comparison with phenelzine in individuals being treated for depression, possibly due to the metabolite 10-hydroxynortriptyline being produced.[13] The authors of a review noted that the nortriptyline group had more episodes prior to treatment.[13]
Notes
- ↑ Brand names include: Sensoval, Aventyl, Pamelor, Norpress, Allegron, Noritren and Nortrilen
References
- 1 2 3 4 Brayfield, A, ed. (9 January 2017). "Nortriptyline Hydrochloride - Martindale: The Complete Drug Reference". MedicinesComplete. Pharmaceutical Press. Retrieved 11 August 2017.
- ↑ Sweetman SC, ed. (2002). Martindale. The complete drug reference (33 ed.). Pharmaceutical Press. ISBN 0-85369-499-0.
- ↑ Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, Lebel AA, Levy RM, Mackey SC, Mayer J, Miaskowski C, Raja SN, Rice AS, Schmader KE, Stacey B, Stanos S, Treede RD, Turk DC, Walco GA, Wells CD (Mar 2010). "Recommendations for the pharmacological management of neuropathic pain: an overview and literature update". Mayo Clinic Proceedings. 85 (3 Suppl): S3–14. PMC 2844007
 . PMID 20194146. doi:10.4065/mcp.2009.0649.
. PMID 20194146. doi:10.4065/mcp.2009.0649. - ↑ "ALLEGRON". TGA eBusiness Services. Arrow Pharma Pty Ltd. 13 October 2016. Retrieved 11 August 2017.
- ↑ Rudorfer MV, Potter WZ (Jun 1999). "Metabolism of tricyclic antidepressants". Cellular and Molecular Neurobiology. 19 (3): 373–409. PMID 10319193.
- 1 2 Stingl JC, Brockmöller J, Viviani R (Mar 2013). "Genetic variability of drug-metabolizing enzymes: the dual impact on psychiatric therapy and regulation of brain function". Molecular Psychiatry. 18 (3): 273–87. PMID 22565785. doi:10.1038/mp.2012.42.
- 1 2 Kirchheiner J, Seeringer A (Mar 2007). "Clinical implications of pharmacogenetics of cytochrome P450 drug metabolizing enzymes". Biochimica et Biophysica Acta. 1770 (3): 489–94. PMID 17113714. doi:10.1016/j.bbagen.2006.09.019.
- 1 2 3 4 Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Müller DJ, Gaedigk A, Stingl JC (May 2013). "Clinical Pharmacogenetics Implementation Consortium guideline for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants". Clinical Pharmacology and Therapeutics. 93 (5): 402–8. PMC 3689226
 . PMID 23486447. doi:10.1038/clpt.2013.2.
. PMID 23486447. doi:10.1038/clpt.2013.2. - ↑ Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, Rongen GA, van Schaik RH, Schalekamp T, Touw DJ, van der Weide J, Wilffert B, Deneer VH, Guchelaar HJ (May 2011). "Pharmacogenetics: from bench to byte--an update of guidelines". Clinical Pharmacology and Therapeutics. 89 (5): 662–73. PMID 21412232. doi:10.1038/clpt.2011.34.
- ↑ National Institute of Mental Health. PDSD Ki Database (Internet) [cited 2013 Oct 3]. Chapel Hill (NC): University of North Carolina. 1998-2013. Available from: http://pdsp.med.unc.edu/pdsp.php
- ↑ Brunton L, Chabner B, Knollman B. Goodman and Gilman’s The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional; 2010.
- ↑ Thase ME (2006). "Depression and sleep: pathophysiology and treatment". Dialogues in Clinical Neuroscience. 8 (2): 217–26. PMC 3181772
 . PMID 16889107.
. PMID 16889107. - 1 2 Kennedy SH (Mar 1997). "Continuation and maintenance treatments in major depression: the neglected role of monoamine oxidase inhibitors". Journal of Psychiatry & Neuroscience. 22 (2): 127–31. PMC 1188835
 . PMID 9074307.
. PMID 9074307.
External links
- Drugs.com - Nortriptyline