National Cancer Institute
 | |
| Agency overview | |
|---|---|
| Formed | 1937 |
| Jurisdiction | United States |
| Headquarters | Rockville, Maryland U.S. |
| Agency executive |
|
| Parent agency |
U.S. Department of Health and Human Services National Institutes of Health |
| Website | www.cancer.gov |
The National Cancer Institute (NCI) is part of the National Institutes of Health (NIH), which is one of eleven agencies that are part of the U.S. Department of Health and Human Services. The NCI coordinates the U.S. National Cancer Program and conducts and supports research, training, health information dissemination, and other activities related to the causes, prevention, diagnosis, and treatment of cancer; the supportive care of cancer patients and their families; and cancer survivorship. On April 1, 2015, Douglas Lowy, M.D.[1] was named the Acting Director of NCI.
On June 10, 2017, President Donald J. Trump announced his intent to appoint Norman Sharpless as director of the National Cancer Institute.
The National Cancer Institute mediates the majority of its mission via an extramural program that provides grants for cancer research. Additionally, the National Cancer Institute has intramural research programs, which constitutes a small fraction of the overall National Cancer Institute budget, in Bethesda, Maryland and at the Frederick National Laboratory for Cancer Research[2] at Fort Detrick, in Frederick, Maryland.
Legislative history
Congress established the NCI by the National Cancer Institute Act, August 6, 1937, as an independent research institute. Congress then made the NCI an operating division of the National Institutes of Health by the Public Health Service Act, July 1, 1944. Congress amended the Public Health Service Act with the National Cancer Act of 1971 to broaden the scope and responsibilities of the NCI "in order more effectively to carry out the national effort against cancer." Over the years, legislative amendments have maintained the NCI authorities and responsibilities and added new information dissemination mandates as well as a requirement to assess the incorporation of state-of-the-art cancer treatments into clinical practice.
Anti-cancer drug investigations
The NCI played an early role in the discovery of anti-cancer drugs in the U.S. According to a 1996 NCI analysis of drugs approved by the Food and Drug Administration (FDA), two-thirds of the anti-cancer drugs approved as of the end of 1995 were NCI-sponsored Investigational New Drugs:[3]
.
- Chlorambucil (Leukeran) (1957)
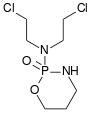
- Cyclophosphamide (Cytoxan) (1959)
- Thiotepa (1959)
- Melphalan (Alkeran) (1959) (IV in 1993)
- Streptozotocin (Zanosar) (1982)
- Ifosfamide (Ifex) (1988)
- Mercaptopurine (1953)
- Methotrexate (1953)
- Thioguanine (1966)
- Cytosine arabinoside (Ara-C) (1969)
- Floxuridine (FUDR) (1970)
- Fludarabine phosphate (1991)
- Pentostatin (1991)
- Chlorodeoxyadenosine (1992)
Plant alkaloids and antibiotics
- Vincristine (Oncovin) (1963)
- Actinomycin D (Cosmegen) (1964)
- Mithramycin (Mithracin) (1970)
- Bleomycin (Blenoxane) (1973)
- Doxorubicin (Adriamycin) (1974)
- Mitomycin C (Mutamycin) (1974)
- L-Asparaginase (Elspar) (1978)
- Daunomycin (Cerubidine) (1979)
- VP-16-213 (Etoposide) (1983)
- VM-26 (Teniposide) (1992)
- Taxol (Paclitaxel) (1992)
Synthetic drugs
- Hydroxyurea (Hydrea) (1967)
- Procarbazine (Matulane) (1969)
- O, P'-DDD (Lysodren, Mitotane) (1970)
- Dacarbazine (DTIC) (1975)
- CCNU (Lomustine) (1976)
- BCNU (Carmustine) (1977)
- Cis-diamminedichloroplatinum (Cisplatin) (1978)
- Mitoxantrone (Novantrone) (1988)
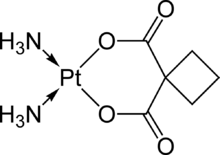
- Carboplatin (Paraplatin) (1989)
- Levamisole (Ergamisol) (1990)
- Hexamethylmelamine (Hexalen) (1990)
- All-trans retinoid acid (Vesanoid) (1995)
- Porfimer sodium (Photofrin) (1995)
- DES (1950)
- Prednisone (1953)
- Fluoxymesterone (Halotestin) (1958)
- Dromostanolone (Drolban) (1961)
- Testolactone (Teslac) (1970)
- Methyl prednisolone
- Prednisolone
- Zoladex (1989)
Biologicals
- Alpha interferon (Intron A, Roferon-A) (1986)
- BCG (TheraCys, TICE) (1990)
- G-CSF (1991)
- GM-CSF (1991)
- Interleukin 2 (Proleukin) (1992)
Imaging Agents
In addition, scientists in the NCI played an important role in the discovery and development of important AIDS drugs including zidovudine (AZT), didanosine (ddI), and zalcitabine (ddC).
Cancer Imaging Program
The NCI Cancer Imaging Program fosters advances in in vivo medical imaging sciences through support of basic and applied research in cancer imaging as well as promotion of imaging in clinical trials in order to gain greater understanding of the pathways of cancer biology for the benefit of cancer patients and people at cancer risk.
Developmental Therapeutics Program
The evolution of strategies at the National Cancer Institute (NCI) illustrates the changes in screening that have resulted from advances in cancer biology. The Developmental Therapeutics Program (DTP) operates a tiered anti-cancer compound screening program with the goal of identifying novel chemical leads and biological mechanisms. The DTP screen is a three phase screen which includes: an initial screen which first involves a single dose cytotoxicity screen with the 60 cell line assay. Those passing certain thresholds are subjected to a 5 dose screen of the same 60 cell-line panel to determine a more detailed picture of the biological activity. A second phase screen establishes the Maximum Tolerable Dosage and involves in vivo examination of tumor regression using the Hollow fiber assay. The third phase of the study is the human tumor xenograft evaluation.[1]
Active compounds are selected for testing based on several criteria: disease type specificity in the in vitro assay, unique structure, potency, and demonstration of a unique pattern of cellular cytotoxicity or cytostasis, indicating a unique mechanism of action or intracellular target.
Some of the approved cancer treatment drugs developed with DTP involvement are: Fluorouracil (1962, NSC-19893), Bleomycin (1973, NSC-125066), Doxorubicin (1974, NSC-123127), cis-Platinum (1978, NSC-119875), Carboplatin (1989, NSC-241240), Taxol (1992, NSC-192573) and Erbitux (2004, NSC-632307).
Drug testing data are represented as a mean graph that displays growth inhibition in a standard bar graph representation. The mean graph is constructed by projecting bars to the right or left of the mean, depending on whether an individual cell line is more or less sensitive than the average line in the panel. Further the length of each bar is proportional to the relative sensitivity of the cell lines. Thus, each agent can be represented by a characteristic fingerprint of cell-line responsiveness, indicated by the bar graph presentation.
These data are presented and analyzed in this section. The broad screen provides a basis for comparison with other compounds, many of which have a known mechanism of action. The NCI COMPARE program is an online database and comparison tool which analyzes both one-dose and five-dose data cytotoxicity data for the 60 cell line panel for similar activity profiles with all the compounds screened previously by the DTP.
A compound is entered into the program as a seed, and the computer database elicits a list of those agents that have similar patterns of cellular cytotoxicity. A correlation coefficient is also expressed relating the closeness of the seed to those agents listed by the computer program. Close correlations between agents demonstrates biological and pharmacological importance and implies a common intracellular target despite dissimilarity in structure.
A high correlation of cytotoxicity with compounds of known biological mechanism is often predictive of the drugs mechanism of action and thus a tool to aid in the drug development and testing. It also tells if there is any unique response of the drug which is not similar to any of the standard prototype compounds in the NCI database.
Methodology of the in-vitro Cancer Screen
The protocol for the NCI-60 screen is as follows. The human tumor cell lines are grown in RPMI 1640 medium containing 5% fetal bovine serum and 2 mM L-glutamine. For a typical screening experiment, cells are inoculated into 96 well microtiter plates in 100 µL at plating densities ranging from 5,000 to 40,000 cells/well depending on the doubling time of individual cell lines. After cell inoculation, the microtiter plates are incubated at 37 °C, 5% CO2, 95% air and 100% relative humidity for 24 h prior to addition of experimental drugs.
After 24 h, two plates of each cell line are fixed in situ with TCA, to represent a measurement of the cell population for each cell line at the time of drug addition (Tz). Experimental drugs are solubilized in dimethyl sulfoxide at 400-fold the desired final maximum test concentration and stored frozen prior to use. At the time of drug addition, an aliquot of frozen concentrate is thawed and diluted to twice the desired final maximum test concentration with complete medium containing 50 µg/mL gentamicin. Additional four, 10-fold or ½log serial dilutions are made to provide a total of five drug concentrations plus control. Aliquots of 100 µl of these different drug dilutions are added to the appropriate microtiter wells already containing 100 µl of medium, resulting in the required final drug concentrations.
Following drug addition, the plates are incubated for an additional 48 h at 37 °C, 5% CO2, 95% air, and 100% relative humidity. For adherent cells, the assay is terminated by the addition of cold TCA. Cells are fixed in situ by the gentle addition of 50 µl of cold 50% (w/v) TCA (final concentration, 10% TCA) and incubated for 60 minutes at 4 °C. The supernatant is discarded, and the plates are washed five times with tap water and air dried. Sulforhodamine B (SRB) solution (100 µl) at 0.4% (w/v) in 1% acetic acid is added to each well, and plates are incubated for 10 minutes at room temperature. After staining, unbound dye is removed by washing five times with 1% acetic acid and the plates are air dried. Bound stain is subsequently solubilized with 10 mM trizma base, and the absorbance is read on an automated plate reader at a wavelength of 515 nm. For suspension cells, the methodology is the same except that the assay is terminated by fixing settled cells at the bottom of the wells by gently adding 50 µl of 80% TCA (final concentration, 16% TCA). Using the seven absorbance measurements [time zero, (Tz), control growth, (C), and test growth in the presence of drug at the five concentration levels (Ti)], the percentage growth is calculated at each of the drug concentrations levels. Percentage growth inhibition is calculated as: [(Ti-Tz)/(C-Tz)] x 100 for concentrations for which Ti>/=Tz [(Ti-Tz)/Tz] x 100 for concentrations for which Ti<Tz.
Three dose response parameters are calculated for each experimental agent.
- GI50
Growth inhibition of 50% (GI50) is calculated from [(Ti-Tz)/(C-Tz)] x 100 = 50, which is the drug concentration resulting in a 50% reduction in the net protein increase (as measured by SRB staining) in control cells during the drug incubation.
- TGI
The drug concentration resulting in total growth inhibition (TGI) is calculated from Ti = Tz.
- LC50
The LC50 (concentration of drug resulting in a 50% reduction in the measured protein at the end of the drug treatment as compared to that at the beginning) indicating a net loss of cells following treatment is calculated from [(Ti-Tz)/Tz] x 100 = -50.
Values are calculated for each of these three parameters if the level of activity is reached; however, if the effect is not reached or is exceeded, the value for that parameter is expressed as greater or less than the maximum or minimum concentration tested.[2]
Quality assurance
The NCI provides funding for numerous cancer research endeavors. Two of its largest known grants include the Radiological Physics Center (RPC) in Houston, Texas and the Quality Assurance Review Center (QARC) in Providence, Rhode Island. The RPC assures the NCI of proper participation in the physics-related aspects of its studies and QARC provides radiotherapy quality assurance and diagnostic imaging data management to all of the NCI sponsored cooperative groups. The RPC essentially guides all participating institutions as to how radiation is to be applied in a radiotherapy protocol. QARC on the other hand performs thousands of radiotherapy reviews per year and receives radiotherapy data from around 1,000 hospitals in both the United States and abroad. In all, over 30,000 cases have been reviewed at QARC since its inception in 1977. QARC also maintains a strategic affiliation with the University of Massachusetts Medical School in Worcester, Massachusetts. The RPC has been consistently funded by the NCI since 1968, and QARC has received support from the NCI since 1980.
Physical Sciences-Oncology Centers
The NCI has set up a network of 12 Physical Sciences-Oncology Centers (PS-OCs) linking the physical sciences to the study of cancer.
Recalcitrant Cancer Research Act
On January 2, 2013, President Barack Obama signed the Recalcitrant Cancer Research Act of 2012 (H.R. 733) into law. This bill, which was included in the National Defense Authorization Act of 2013, requires the NCI to develop scientific frameworks for addressing cancers with survival rates of less than 50 percent. Within this act, lung cancer and pancreatic cancer were given priority status. The NCI framework must be submitted to the United States Congress within 18 months.
Leadership
- Norman Sharpless is Director of the NCI.
- Harold Varmus,[4] M.D. was the 14th Director of the NCI. Co-winner of the Nobel Prize for studies of the genetic basis of cancer, Dr. Varmus was nominated by President Barack Obama to the position on May 17, 2010 and left the NCI on March 31, 2015.
- John E. Niederhuber, MD, 13th Director of the NCI, was nominated by President George W. Bush, serving in the role from 2006 to July 2010.[5]
- Andrew von Eschenbach, the 12th Director, served from 2001 to 2006 before transitioning to a role as Commissioner of Food and Drugs.[6][7] He is now an adjunct professor at the University of Texas MD Anderson Cancer Center and serves on the board of directors of BioTime, a biotechnology company.[8]
- Richard D. Klausner, the 11th Director, served from 1995 to 2001 before leaving to become President of the Case Institute of Health, Science, and Technology and later Executive Director of Global Health for the Bill & Melinda Gates Foundation.[9]
- Kathryn Zoon, Principal Deputy Director, 2002 to 2004.
- Michael B. Sporn was the Chief of the Laboratory of Chemoprevention, 1978 to 1995.
See also
- American Cancer Society Cancer Action Network
- American Cancer Society Center
- caBIG, the Cancer BioInformatics Grid, a National Cancer Institute (USA) initiative to link cancer researchers and their data
- Canadian Cancer Society
- Cancer Information Service (CIS)
- Discovery and development of mTOR inhibitors
- European Organisation for Research and Treatment of Cancer (EORTC)
- Journal of the National Cancer Institute
- National Comprehensive Cancer Network
- NCI-designated Cancer Center
- NSC, the National Service Center
- Oncology
- Programme of Action for Cancer Therapy A close partner in dealing with cancer care in developing world
Notes and references
- 1 2 "Director's Page - National Cancer Institute". Cancer.gov. Retrieved 2015-04-01.
- ↑ "NCI-Frederick: NCI-Frederick Home Page". Ncifcrf.gov. Retrieved 2011-12-18.
- ↑ "Affidavit of James Love". www.cptech.org. Retrieved 2017-05-09.
- ↑ "Director's Page - National Cancer Institute (Archive)". Cancer.gov. Retrieved 2015-04-02.
- ↑ "Emergent Biosolutions - Board of Directors bio". Retrieved 2013-12-06.
- ↑ U.S. Congress (7 December 2006). "Executive Session". Congressional Record. 152 (134): S11404–29, S11447–51. Retrieved 2006-12-12.
- ↑ Senate Vote No. 274
- ↑ "Milken Institute Non-Resident Fellows".
- ↑ "Dr. Richard D. Klausner Named Executive Director of Global Health for Bill & Melinda Gates Foundation".
General references
- National Cancer Institute Retrieved 11 June 2010.
- "NCI MISSION STATEMENT." National Cancer Institute. Retrieved 18 August 2004.
- "THE NATIONAL CANCER ACT OF 1971." National Cancer Institute. Retrieved 18 August 2004.
- Developmental Therapeutics Program (DTP)
- NCI-60 DTP Human Tumor Cell Line Screen