Mycoplasma
| Mycoplasma | |
|---|---|
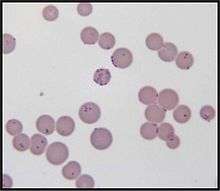 | |
| Mycoplasma haemofelis | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Tenericutes |
| Class: | Mollicutes |
| Order: | Mycoplasmatales |
| Family: | Mycoplasmataceae |
| Genus: | Mycoplasma Nowak 1929 |
| Mycoplasmosis | |
|---|---|
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | A49.3 |
| ICD-9-CM | 041.81 |
Mycoplasma is a genus of bacteria that lack a cell wall around their cell membrane.[1] Without a cell wall, they are unaffected by many common antibiotics such as penicillin or other beta-lactam antibiotics that target cell wall synthesis. They can be parasitic or saprotrophic. Several species are pathogenic in humans, including M. pneumoniae, which is an important cause of atypical pneumonia and other respiratory disorders, and M. genitalium, which is believed to be involved in pelvic inflammatory diseases. Mycoplasma species are the smallest bacterial cells yet discovered,[2] can survive without oxygen, and come in various shapes. For example, M. genitalium is flask-shaped (about 300 x 600 nm), while M. pneumoniae is more elongated (about 100 x 1000 nm). Hundreds of mycoplasma species infect animals.[3]
Origin of the name
The term mycoplasma, from the Greek μυκής, mykes (fungus) and πλάσμα, plasma (formed), was first used by Albert Bernhard Frank in 1889 to describe an altered state of plant cell cytoplasm resulting from infiltration by fungus-like microorganisms.[4] Julian Nowak later proposed the genus name Mycoplasma for certain filamentous microorganisms imagined to have both cellular and acellular stages in their lifecycles, which could explain how they were visible with a microscope, but passed through filters impermeable to bacteria.[5]
Later, the name for Mycoplasma was pleuropneumonia-like organisms (PPLO), broadly referring to organisms similar in colonial morphology and filterability to the causative agent (a mycoplasma) of contagious bovine pleuropneumonia.[6]
Species
- M. adleri
- M. agalactiae
- M. agassizii
- M. alkalesens
- M. alligatoris
- M. amphoriforme
- M. anatis
- M. anseris
- M. arginini
- M. arthritidis
- M. auris
- M. bovigenitalium
- M. bovirhinis
- M. bovis
- M. bovoculi
- M. buccale
- M. buteonis
- M. californicum
- M. canadense
- M. canis
- M. capricolum
- M. caviae
- M. cavipharyngis
- M. citelli
- M. cloacale
- M. coccoides
- M. collis
- M. columbinasale
- M. columbinum
- M. columborale
- M. conjunctivae
- M. corogypsi
- M. cottewii
- M. cricetuli
- M. crocodyli
- M. cynos
- M. dispar
- M. edwardii
- M. elephantis
- M. ellychniae
- M. equigenitalium
- M. equirhinis
- M. falconis
- M. fastidiosum
- M. faucium
- M. felifacium
- M. feliminutum
- M. feriruminatoris[7]
- M. fermentans
- M. flocculare
- M. gallinaceum
- M. gallinarum
- M. gallisepticum
- M. gallopavonis
- M. gaeteae
- M. genitalium
- M. glycophilium
- M. gypis
- M. haemocanis
- M. haemofelis
- M. haemomuris
- M. haemosuis
- M. hominis
- M. hyopneumoniae
- M. hypopharyngis
- M. hyorhinis
- M. hyosynoviae
- M. iguanae
- M. imitans
- M. indiense
- M. iners
- M. iowae
- M. laboratorium
- M. lacutcae
- M. lagogenitalium
- M. leachii
- M. leonicptivi
- M. leopharyngis
- M. lipofaciens
- M. lipophilum
- M. lucivorax
- M. luminosum
- M. maculosum
- M. melaleucae
- M. meleagridis
- M. microti
- M. moatsii
- M. mobile
- M. molare
- M. muscosicanis
- M. muris
- M. mustelae
- M. mycoides
- M. neophronis
- M. neurolyticvum
- M. opalescens
- M. orale
- M. ovipneumoniae
- M. ovis
- M. ovipneumoniae
- M. oxoniensis
- M. penetrans
- M. phocae
- M. phocicerebrale
- M. phocidae
- M. phocirhinis
- M. pirum
- M. pneumoniae
- M. primatum
- M. pullorum
- M. pulmonis
- M. putrefaciens
- M. salivarium
- M. simbae
- M. spermatophilum
- M. spumans
- M. sturni
- M. sualvi
- M. subdolum
- M. suis
- M. synoviae
- M. testudineum
- M. testudinis
- M. verecunum
- M. wenyonii
- M. yeatsii
Species that infect humans
Other species of Mycoplasma other than those listed below have been recovered from humans, but are assumed to have been contracted from animals. These use humans as the primary host:
Pathophysiology
Mycoplasma species have been isolated from women with bacterial vaginosis.[3] M. genitalium infection is associated with increased risk of cervicitis, pelvic inflammatory disease, preterm birth and spontaneous abortion, and infertility.[9] Mycoplasmae are associated with fetal respiratory distress syndrome, bronchopulmonary dysplasia, and intraventricular hemorrhage in preterm infants.[3]
Characteristics
Over 100 species have been included in the genus Mycoplasma. Microbes of the class Mollicutes, to which Mycoplasma belongs, are parasites or commensals of humans, animals, and plants. The genus Mycoplasma uses vertebrate and arthropod hosts.[10] Dietary nitrogen availability has been shown to alter codon bias and genome evolution in Mycoplasma and Phytoplasma.[11]
Cell morphology
"Due to the lack of a rigid cell wall, Mycoplasmataceae can contort into a broad range of shapes, from round to oblong. They therefore cannot be classified as rods or cocci."[12]
Laboratory contaminant
Mycoplasma species are often found in research laboratories as contaminants in cell culture. Mycoplasmal cell culture contamination occurs due to contamination from individuals or contaminated cell culture medium ingredients.[13] Mycoplasma cells are physically small – less than 1 µm, so are difficult to detect with a conventional microscope.
Mycoplasmae may induce cellular changes, including chromosome aberrations, changes in metabolism and cell growth. Severe Mycoplasma infections may destroy a cell line. Detection techniques include DNA Probe, enzyme immunoassays, PCR, plating on sensitive agar and staining with a DNA stain including DAPI or Hoechst.
An estimated 11 to 15% of U.S. laboratory cell cultures are contaminated with mycoplasma. A Corning study showed that half of U.S. scientists did not test for Mycoplasma contamination in their cell cultures. The study also stated that, in former Czechoslovakia, 100% of cell cultures that were not routinely tested were contaminated while only 2% of those routinely tested were contaminated (study page 6). Since the U.S. contamination rate was based on a study of companies that routinely checked for Mycoplasma, the actual contamination rate may be higher. European contamination rates are higher and that of other countries are higher still (up to 80% of Japanese cell cultures).[14] About 1% of published Gene Expression Omnibus data may have been compromised.[15][16] Several antibiotic-containing formulations of antimycoplasmal reagents have been developed over the years.[17]
Synthetic mycoplasma genome
A chemically synthesized genome of a mycoplasmal cell based entirely on synthetic DNA which can self-replicate has been referred to as Mycoplasma laboratorium.[18]
Pathogenicity
The P1 antigen is the primary virulence factor of mycoplasma. P1 is a membrane associated protein that allows adhesion to epithelial cells. The P1 receptor is also expressed on erythrocytes which can lead to autoantibody agglutination from mycobacteria infection.[19] Several Mycoplasma species can cause disease, including M. pneumoniae, which is an important cause of atypical pneumonia (formerly known as "walking pneumonia"), and M. genitalium, which has been associated with pelvic inflammatory diseases. Mycoplasma infections in humans are associated with skin eruptions in 17% of cases.[20]:293
Sexually transmitted infections
Mycoplasma and Ureaplasma species are not part of the normal vaginal flora. Some Mycoplasma species are spread through sexual contact.[21]
Infertility
Some mycoplasmae have a negative effect on fertility.[21] M. hominis causes male sterility/Genitals inflammation in humans.
Infant mortality
Low birth-weight, preterm infants are susceptible to Mycoplasma infections.[8]
Links to cancer
Several species of Mycoplasma are frequently detected in different types of cancer cells.[22][23][24] These species are:
- M. fermentans[22][23][24][25][26][27]
- M. genitalium[28]
- M. hominis[29]
- M. hyorhinis[22][28][30]
- M. penetrans[22][23][24][25][27]
- U. urealyticum[31]
The majority of these mycoplasmae have shown a strong correlation to malignant transformation in mammalian cells in vitro.
Mycoplasma infection and host cell transformation
The presence of Mycoplasma was first reported in samples of cancer tissue in the 1960s.[24] Since then, several studies tried to find and prove the connection between Mycoplasma and cancer, as well as how the bacterium might be involved in the formation of cancer.[23] Several studies have shown that cells that are chronically infected with the bacteria go through a multistep transformation. The changes caused by chronic mycoplasmal infections occur gradually and are both morphological and genetic.[23] The first visual sign of infection is when the cells gradually shift from their normal form to sickle-shaped. They also become hyperchromatic due to an increase of DNA in the nucleus of the cells. In later stages, the cells lose the need for a solid support to grow and proliferate, as well as the normal contact-dependent inhibition cells.[24]
Possible intracellular mechanisms of mycoplasmal malignant transformation
Karyotypic changes related to mycoplasma infections
Cells infected with Mycoplasma for an extended period of time show significant chromosomal abnormalities. These include the addition of chromosomes, the loss of entire chromosomes, partial loss of chromosomes, and chromosomal translocation. All of these genetic abnormalities may contribute to the process of malignant transformation. Chromosomal translocation and extra chromosomes help create abnormally high activity of certain proto-oncogenes, which caused by these genetic abnormalities and include those encoding c-myc, HRAS,[25] and vav.[23] The activity of proto-oncogenes is not the only cellular function that is affected; tumour suppressor genes are affected by the chromosomal changes induced by mycoplasma, as well. Partial or complete loss of chromosomes causes the loss of important genes involved in the regulation of cell proliferation.[24] Two genes whose activities are markedly decreased during chronic infections with mycoplasma are the Rb and the p53 tumour suppressor genes.[23] Another possible mechanism of carcinogenesis is RAC1 activation by a small GTPase-like protein fragment of Mycoplasma.[32] A major feature that differentiates mycoplasmas from other carcinogenic pathogens is that the mycoplasmas do not cause the cellular changes by insertion of their own genetic material into the host cell.[25] The exact mechanism by which the bacterium causes the changes is not yet known.
- Partial reversibility of malignant transformations
The malignant transformation induced by mycoplasmae is also different from that caused by other pathogens in that the process is reversible. The state of reversal is, however, only possible up to a certain point during the infection. The window of time when reversibility is possible varies greatly; it depends primarily on the Mycoplasma involved. In the case of M. fermentans, the transformation is reversible until around week 11 of infection and starts to become irreversible between weeks 11 and 18.[24] If the bacteria are killed using antibiotics[24] (i.e. ciprofloxacin[23] or Clarithromycin[33]) before the irreversible stage, the infected cells should return to normal.
Connections to cancer in vivo and future research
Epidemiologic, genetic, and molecular studies suggest infection and inflammation initiate certain cancers, including those of the prostate. M. genitalium and M. hyorhinis induce malignant phenotype in benign human prostate cells (BPH-1) that were not tumorigenic after 19 weeks of exposure. [28]
Types of cancer associated with Mycoplasma
Colon cancer: In a study to understand the effects of Mycoplasma contamination on the quality of cultured human colon cancer cells, a positive correlation was found between the number of M. hyorhinis cells present in the sample and the percentage of CD133-positive cells (a glycoprotein with an unknown function).[34]
Gastric cancer: Strong evidence indicates the infection of M. hyorhinis contributes to the development of cancer within the stomach and increases the likelihood of malignant cancer cell development.[35]
Lung cancer: Studies on lung cancer have supported the belief that more than a coincidental positive correlation exists between the appearance of Mycoplasma strains in patients and the infection with tumorigenesis.[36]
Prostate cancer: p37, a protein encoded for by M. hyorhinis, has been found to promote the invasiveness of prostate cancer cells. The protein also causes the growth, morphology, and the gene expression of the cells to change, causing them to become a more aggressive phenotype.[37]
Renal cancer: Patients with renal cell carcinoma (RCC) exhibited a significantly high amount of Mycoplasma sp. compared with the healthy control group. This suggests Mycoplasma may play a role in the development of RCC.[33]
See also
- International Organization for Mycoplasmology (IOM)
- Sexually transmitted disease
- Vaginal flora
- Vaginal infection
- Vaginal disease
- Vaginal health
References
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 409–12. ISBN 0-8385-8529-9.
- ↑ Richard L. Sweet; Ronald S. Gibbs. Infectious Diseases of the Female Genital Tract. Lippincott Williams & Wilkins, 2009.
- 1 2 3 Larsen, Bryan; Hwang, Joseph (2010). "Mycoplasma, Ureaplasma, and Adverse Pregnancy Outcomes: A Fresh Look". Infectious Diseases in Obstetrics and Gynecology. 2010: 1–7. ISSN 1064-7449. doi:10.1155/2010/521921.
- ↑ Krass CJ, Gardner MW (January 1973). "Etymology of the Term Mycoplasma" (PDF). Int. J. Of Syst. Bact. 23 (1): 62–64. doi:10.1099/00207713-23-1-62.
- ↑ Browning GF, Citti C (editors) (2014). Mollicutes Molecular Biology and Pathogenesis (1st ed.). Caister Academic Press. pp. 1–14. ISBN 978-1-908230-30-0.
- ↑ Edward DG, Freundt EA (February 1956). "The classification and nomenclature of organisms of the pleuropneumonia group" (PDF). J. Gen. Microbiol. 14 (1): 197–207. PMID 13306904. doi:10.1099/00221287-14-1-197.
- ↑ LPSN bacterio.net
- 1 2 Waites, K. B.; Katz, B.; Schelonka, R. L. (2005). "Mycoplasmas and Ureaplasmas as Neonatal Pathogens". Clinical Microbiology Reviews. 18 (4): 757–789. ISSN 0893-8512. doi:10.1128/CMR.18.4.757-789.2005.
- ↑ Lis, R.; Rowhani-Rahbar, A.; Manhart, L. E. (2015). "Mycoplasma genitalium Infection and Female Reproductive Tract Disease: A Meta-Analysis". Clinical Infectious Diseases. 61 (3): 418–426. ISSN 1058-4838. PMID 25900174. doi:10.1093/cid/civ312.
- ↑ Maggi, Ricardo G.; Compton, Sarah M.; Trull, Chelsea L.; Mascarelli, Patricia E.; Mozayeni, B. Robert; Breitschwerdt, Edward B. (1 October 2013). "Infection with Hemotropic Mycoplasma Species in Patients with or without Extensive Arthropod or Animal Contact". Journal of Clinical Microbiology. pp. 3237–3241. PMC 3811635
 . doi:10.1128/JCM.01125-13.
. doi:10.1128/JCM.01125-13. - ↑ Seward, Emily; Kelly, Steve (2016). "Dietary nitrogen alters codon bias and genome composition in parasitic microorganisms". Genome Biology. 17 (226): 3–15. PMC 5109750
 . PMID 27842572. doi:10.1186/s13059-016-1087-9.
. PMID 27842572. doi:10.1186/s13059-016-1087-9. - ↑ Gladwin, MD, Mark; Trattler, MD, William; Mahan, MD, C. Scott (2014). Clinical Microbiology made ridiculously simple. Miami, Fl: MedMaster, Inc. p. 156. ISBN 978-1935660156.
- ↑ Drexler HG; Uphoff CC (2002). "Mycoplasma contamination of cell cultures: Incidence, sources, effects, detection, elimination, prevention". Cytotechnology. 39 (2): 75–90. PMC 3463982
 . PMID 19003295. doi:10.1023/A:1022913015916.
. PMID 19003295. doi:10.1023/A:1022913015916. - ↑ John Ryan (2008). "Understanding and Managing Cell Culture Contamination" (PDF). Corning Incorporated. p. 24.
- ↑ Aldecoa-Otalora E, Langdon W, Cunningham P, Arno MJ (December 2009). "Unexpected presence of mycoplasma probes on human microarrays". BioTechniques. 47 (6): 1013–5. PMID 20047202. doi:10.2144/000113271.
- ↑ Link into RNAnet showing contamination of GEO. Press plot and drag blue crosshairs to expose links to description of experiments on human RNA samples
- ↑ BM-Cyclin by Roche, MRA by ICN, Plasmocin by Invivogen and more recently De-Plasma by TOKU-E.
- ↑ Gibson DG, Glass JI, Lartigue C, Noskov VN, Chuang RY, Algire MA, Benders GA, Montague MG, Ma L, Moodie MM, Merryman C, Vashee S, Krishnakumar R, Assad-Garcia N, Andrews-Pfannkoch C, Denisova EA, Young L, Qi ZQ, Segall-Shapiro TH, Calvey CH, Parmar PP, Hutchison CA, Smith HO, Venter JC (July 2010). "Creation of a bacterial cell controlled by a chemically synthesized genome". Science. 329 (5987): 52–6. PMID 20488990. doi:10.1126/science.1190719.
- ↑ Parija, Subhash Chandra (2014). Textbook of Microbiology & Immunology. Elsevier Health Sciences. ISBN 9788131236246.
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- 1 2 Ljubin-Sternak, Suncanica; Mestrovic, Tomislav (2014). "Review: Clamydia trachonmatis and Genital Mycoplasmias: Pathogens with an Impact on Human Reproductive Health". Journal of Pathogens. 2014 (183167): 1–15. PMC 4295611
 . PMID 25614838. doi:10.1155/2014/183167.
. PMID 25614838. doi:10.1155/2014/183167. - 1 2 3 4 Huang S, Li JY, Wu J, Meng L, Shou CC (April 2001). "Mycoplasma infections and different human carcinomas". World Journal of Gastroenterology. 7 (2): 266–269. PMC 4723534
 . PMID 11819772. doi:10.3748/wjg.v7.i2.266.
. PMID 11819772. doi:10.3748/wjg.v7.i2.266. - 1 2 3 4 5 6 7 8 Sinkovics JG (February 2012). "Molecular biology of oncogenic inflammatory processes. I. Non-oncogenic and oncogenic pathogens, intrinsic inflammatory reactions without pathogens, and microRNA/DNA interactions (Review)". International Journal of Oncology. 40 (2): 305–349. PMID 22076306. doi:10.3892/ijo.2011.1248.
- 1 2 3 4 5 6 7 8 Tsai S, Wear DJ, Shih JW, Lo SC (October 1995). "Mycoplasmas and oncogenesis: Persistent infection and multistage malignant transformation". Proceedings of the National Academy of Sciences of the United States of America. 92 (22): 10197–10201. PMC 40763
 . PMID 7479753. doi:10.1073/pnas.92.22.10197.
. PMID 7479753. doi:10.1073/pnas.92.22.10197. - 1 2 3 4 Cimolai N (August 2001). "Do mycoplasmas cause human cancer?". Canadian Journal of Microbiology. 47 (8): 691–697. PMID 11575494. doi:10.1139/w01-053.
- ↑ Jiang S, Zhang S, Langenfeld J, Lo SC, Rogers MB (May 2008). "Mycoplasma infection transforms normal lung cells and induces bone morphogenetic protein 2 expression by post-transcriptional mechanisms". Journal of Cellular Biochemistry. 104 (2): 580–594. PMID 18059017. doi:10.1002/jcb.21647.
- 1 2 Zhang S, Tsai S, Lo SC (May 2006). "Alteration of gene expression profiles during mycoplasma-induced malignant cell transformation". BMC Cancer. 6: 116. PMC 1559712
 . PMID 16674811. doi:10.1186/1471-2407-6-116.
. PMID 16674811. doi:10.1186/1471-2407-6-116. - 1 2 3 Namiki K, Goodison S, Porvasnik S, Allan RW, Iczkowski KA, Urbanek C, Reyes L, Sakamoto N, Rosser CJ (September 2009). "Persistent exposure to mycoplasma induces malignant transformation of human prostate cells". PLoS ONE. 4 (9): 1–9. PMC 2730529
 . PMID 19721714. doi:10.1371/journal.pone.0006872.
. PMID 19721714. doi:10.1371/journal.pone.0006872. - ↑ Barykova YA, Logunov DY, Shmarov MM, Vinarov AZ, Fiev DN, Vinarova NA, Rakovskaya IV, Baker PS, Shyshynova I, Stephenson AJ, Klein EA, Naroditsky BS, Gintsburg AL, Gudkov AV (2011). "Association of Mycoplasma hominis infection with prostate cancer". Oncotarget. 2: 289–97. PMC 3248169
 . PMID 21471611. doi:10.18632/oncotarget.256.
. PMID 21471611. doi:10.18632/oncotarget.256. - ↑ Chan PJ, Seraj IM, Kalugdan TH, King A (November 1996). "Prevalence of mycoplasma conserved DNA in malignant ovarian cancer detected using sensitive PCR–ELISA". Gynecologic Oncology. 63 (2): 258–260. PMID 8910637. doi:10.1006/gyno.1996.0316.
- ↑ Xiaolei C, Taot H, Zongli S, Hongying Y (2014). "The role of ureaplasma urealyticum infection in cervical intraepithelial neoplasia and cervical cancer". European Journal of Gynaecological Oncology. 35 (5): 571–5. PMID 25423707.
- ↑ Hu X, Yu J, Zhou X, Li Z, Xia Y, Luo Z, Wu Y (Jan 2014). "A small GTPase-like protein fragment of Mycoplasma promotes tumor cell migration and proliferation in vitro via interaction with Rac1 and Stat3.". J Mol Med Rep. 9 (1): 173–179. PMID 24172987. doi:10.3892/mmr.2013.1766.
- 1 2 Pehlivan M, Pehlivan S, Onay H, Koyuncuoglu M, Kirkali Z (February 2005). "Can mycoplasma-mediated oncogenesis be responsible for formation of conventional renal cell carcinoma?". Urology. 65 (2): 411–414. PMID 15708077. doi:10.1016/j.urology.2004.10.015.
- ↑ Mariotti E, Gemei M, Mirabelli P, D'Alessio F, Di Noto R, Fortunato G, Del Vecchio L (March 2010). "The percentage of CD133+ cells in human colorectal cancer cell lines is influenced by Mycoplasma hyorhinis infection". BMC Cancer. 10: 120–125. PMC 2854114
 . PMID 20353562. doi:10.1186/1471-2407-10-120.
. PMID 20353562. doi:10.1186/1471-2407-10-120. - ↑ Yang H, Qu L, Ma H, Chen L, Liu W, Liu C, Meng L, Wu J, Shou C (November 2010). "Mycoplasma hyorhinis infection in gastric carcinoma and its effects on the malignant phenotypes of gastric cancer cells". BMC Gastroenterology. 10: 132–140. PMC 2993648
 . PMID 21062494. doi:10.1186/1471-230X-10-132.
. PMID 21062494. doi:10.1186/1471-230X-10-132. - ↑ Apostolou P, Tsantsaridou A, Papasotiriou I, Toloudi M, Chatziioannou M, Giamouzis G (October 2011). "Bacterial and fungal microflora in surgically removed lung cancer samples". Journal of Cardiothoracic Surgery. 6: 137. PMC 3212932
 . PMID 21999143. doi:10.1186/1749-8090-6-137.
. PMID 21999143. doi:10.1186/1749-8090-6-137. - ↑ Urbanek C, Goodison S, Chang M, Porvasnik S, Sakamoto N, Li CZ, Boehlein SK, Rosser CJ (June 2011). "Detection of antibodies directed at M. hyorhinis p37 in the serum of men with newly diagnosed prostate cancer". BMC Cancer. 11 (1): 233–238. PMC 3129326
 . PMID 21663671. doi:10.1186/1471-2407-11-233.
. PMID 21663671. doi:10.1186/1471-2407-11-233.
External links
- Compare the size of these small bacteria to the sizes of other cells and viruses.
- MedPix(r)Images Mycoplasma Pneumonia
- Ureaplasma Infection: eMedicine Infectious Diseases
- Antibiotics formulation for eradication of mycoplasma in cell culture media
- Mycoplasma elimination and prevention in cell culture
- Mycoplasma at BacDive - the Bacterial Diversity Metadatabase