Moyamoya disease
| Moyamoya disease | |
|---|---|
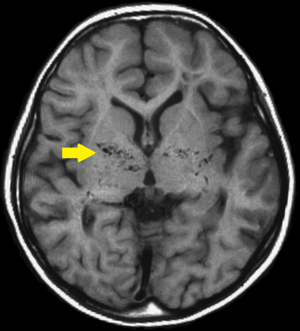 | |
| T1-weighted MR image of moyamoya disease. Flow void in the basal ganglia is indicated by the arrow. | |
| Classification and external resources | |
| Specialty | neurosurgery |
| ICD-10 | Xxx.x |
| ICD-9-CM | xxx |
| Patient UK | Moyamoya disease |
Moyamoya disease is a disease in which certain arteries in the brain are constricted. Blood flow is blocked by the constriction, and also by blood clots (thrombosis).[1]
A collateral circulation develops around the blocked vessels to compensate for the blockage, but the collateral vessels are small, weak, and prone to bleeding, aneurysm and thrombosis. On conventional X-ray angiography, these collateral vessels have the appearance of a "puff of smoke" (described as "もやもや (moyamoya)" in Japanese).[1]
When Moyamoya is diagnosed by itself, with no underlying correlational conditions, it is diagnosed as Moyamoya disease. This is also the case when the arterial constriction and collateral circulation are bilateral. Moyamoya syndrome is unilateral arterial constriction or occurs when one of the several specified conditions is also present. [2] This may also be considered as Moyamoya being secondary to the primary condition. Mainly occlusion of distal internal carotid artery occurs.On angiography "puff of smoke"appearance is seen.Treatment of choice is surgical bypass.
Cause
About 10% of cases of moyamoya disease are familial, and some cases result from specific genetic mutations. Susceptibility to moyamoya disease-2 (MYMY2; 607151) is caused by variation in the RNF213 gene (613768) on chromosome 17q25. Moyamoya disease-5 (MYMY5; 614042) is caused by mutation in the ACTA2 gene (102620) on chromosome 10q23.3; and moyamoya disease-6 with achalasia (MYMY6; 615750) is caused by mutation in the GUCY1A3 gene (139396) on chromosome 4q32. Loci for the disorder have been mapped to chromosome 3p (MYMY1) and chromosome 8q23 (MYMY3; 608796). See also MYMY4 (300845), an X-linked recessive syndromic disorder characterized by moyamoya disease, short stature, hypergonadotropic hypogonadism, and facial dysmorphism. and linked to q25.3, on chromosome 17". (Online Mendelian Inheritance in Man, omim.org/entry/252350).
In Japan the overall incidence is higher (0.35 per 100,000).[3] In North America, women in the third or fourth decade of life are most often affected, but the condition may also occur during infancy or childhood. These women frequently experience transient ischaemic attacks (TIA), cerebral hemorrhage, or may not experience any symptoms at all. They have a higher risk of recurrent stroke and may be experiencing a distinct underlying pathophysiology compared to patients from Japan.[4]
Moyamoya disease can be either congenital or acquired. Patients with Down syndrome, sickle cell anemia, neurofibromatosis type 1, congenital heart disease, fibromuscular dysplasia, activated protein C resistance, or head trauma can develop moyamoya malformations.[5] It is more common in women than in men, although about a third of those affected are male.[6]
Pathophysiology
The disease moyamoya, which is a Japanese mimetic word, gets its characteristic name due to the appearance of smoke on relevant angiographs resultant from the tangle of tiny vessels in response to stenosis. This makes the blood leak out of the arteries, causing pressure to the brain and subsequent headaches. The pathogenesis of moyamoya disease is unknown, although the gene ring finger protein 213 (RNF213) has been implicated.[7]
Once it begins, the vascular occlusion tends to continue despite any known medical management. In some people this leads do
transient ischemic attacks or repeated strokes with severe functional impairment or even death. In others, the blockage may not cause any symptoms.
The disease causes constrictions primarily in the internal carotid artery, and often extends to the middle and anterior cerebral arteries, branches of the internal carotid artery inside the skull.[1] When the internal carotid artery becomes completely blocked, the fine collateral circulation that it supplies is obliterated. Patients often survive on the collateral circulation from the back (posterior) of the circle of Willis, arising from the basilar artery.[1]
The arterial constrictions in moyamoya disease are unlike the constrictions in atherosclerosis. In atherosclerosis, the walls of arteries are damaged, leading to the deposition of fat and immune cells, and ultimately the accumulation of immune cells laden with fat. In moyamoya, the inner layer of the carotid artery proliferates within the arterial lumen. The artery also fills with blood clots, which may cause strokes.[1]
Moyamoya disease tends to affect adults in the third to fourth decade of life. In children it tends to cause strokes or seizures. In adults it tends to cause strokes or bleeding. The clinical features are strokes, recurrent transient ischemic attacks (TIAs), sensorimotor paralysis (numbness and paralysis of the extremities), convulsions and/or migraine-like headaches. Moreover, following a stroke, secondary bleeding may occur. Such bleeding, called hemorrhagic strokes, may also stem from rupture of the weak neovascular vessel walls.
Diagnosis
The diagnosis of moyamoya is suggested by CT, MRI, or angiogram results. Contrast-enhanced T1-weighted images are better than FLAIR images for depicting the leptomeningeal ivy sign in moyamoya disease. MRI and MRA should be performed for the diagnosis and follow-up of moyamoya disease. Diffusion-weighted imaging can also be used for following the clinical course of children with moyamoya disease, in whom new focal deficits are highly suspicious of new infarcts.
Proliferation of smooth muscle cells in the walls of the Moyamoya affected arteries has been found to be representative of the disease. A study of six autopsies of six patients who died from Moyamoya disease lead to the finding that there is evidence that supports the theory that there is a thickening, or proliferation, of the innermost layer of the vessels affected by Moyamoya. These vessels are the ACA (anterior cerebral artery), MCA (middle cerebral artery), and ICA (internal carotid artery). The occlusion of the ICA results in concomitant diminution of the "puff-of-smoke" collateral's, as they are supplied by the ICA.[8]
Often nuclear medicine studies such as SPECT (single photon emission computerized tomography) are used to demonstrate the decreased blood and oxygen supply to areas of the brain involved with moyamoya disease. Conventional angiography provided the conclusive diagnosis of moyamoya disease in most cases and should be performed before any surgical considerations.
Dr. Darren B. Orbach, MD, PhD explains how the disease progresses as well as the role angiography plays in detecting the progression of Moyamoya in a short video [9]
Biomarkers Associated with Moyamoya
Smith (2015) conducted a study that looked into specific biological markers that correlate to Moyamoya disease. Some of the categories of these biomarkers include phenotypes - conditions commonly related to Moyamoya, radiographical markers for the diagnosis of Moyamoya, and proteins as well as cellular changes that occur in cases of Moyamoya. [10]
Similar to Moyamoya Disease, there are conditions that are closely associated with Moyamoya Syndrome. Some of the more common medical conditions that are closely associated with Moyamoya Syndrome include trisomy 21 (Down's Syndrome), sickle cell disease, and neurofibromatosis type 1. There is also evidence that identifies hyperthyroidism and congenital dwarfing syndromes as two of the more loosely associated syndromes that correlate with the possibility of being diagnosed with Moyamoya Disease later in life. [10]
There is also research that has shown that certain radiographic biomarkers that lead to the diagnosis of Moyamoya Disease have been identified. The specific radiographic markers are now considered an acceptable key component to Moyamoya Disease and have been added to the INternational Classification of Diseases (ICD). These biomarkers of Moyamoya are "stenosis of the distal ICA's up to and including the bifurcation, along with segments of the proximal ACA and MCA...dilated basal collateral vessels must be present" [10] Some other common findings that have not been added to the classification index of those with Moyamoya Disease which are found using radiography involve very distinct changes in the vessels of the brain. These changes include newly formed vessels made to compensate for another change noted, ischemia and cerebrovascular reserve, both found on MRI. Functional changes include evidence of ischemia in vessels of the brain (ICA, ACA, MCA, specifically). It is important to also note that the radiographic biomarkers, in order to be classified as Moyamoya Disease, all findings must be bilateral. If this is not the case and the findings are unilateral, it is diagnosed as Moyamoya Syndrome. [10]
There are also several protein biomarkers that have been linked to the Moyamoya Disease diagnosis. Although the sample size of the studies performed are small due to the rarity of the disease, the findings are indicative of a correlation between the disease and several specific protein biomarkers. [10] Other studies have confirmed the correlation of Moyamoya and adhesion molecule 1 (ICAM-1) being increased as compared to normal vascular function counterparts [11] [12] Furthermore, it has been concluded that the localization of inflammatory cells suggests that the inflammation stimulus iteself may be responsible for the proliferation and occlusion in the ICA, ACA, and MCA found in those with Moyamoya Disease. [2]
Treatment
There is no cure for this disease. Drugs such as antiplatelet agents (including aspirin) are usually given to prevent clots, but surgery is usually recommended. Since moyamoya tends to affect only the internal carotid artery and nearby sections of the adjacent anterior and middle cerebral arteries, surgeons can direct other arteries, such as the external carotid artery or the superficial temporal artery to replace its circulation. The arteries are either sewn directly into the brain circulation, or placed on the surface of the brain to reestablish new circulation after a few weeks.[1]
There are many operations that have been developed for the condition, but currently the most favored are the in-direct procedures EDAS, EMS, and multiple burr holes and the direct procedure STA-MCA. Direct superficial temporal artery (STA) to middle cerebral artery (MCA) bypass is considered the treatment of choice, although its efficacy, particularly for hemorrhagic disease, remains uncertain. Multiple burr holes have been used in frontal and parietal lobes with good neovascularisation achieved.
The EDAS (encephaloduroarteriosynangiosis) procedure is a synangiosis procedure that requires dissection of a scalp artery over a course of several centimeters and then making a small temporary opening in the skull directly beneath the artery. The artery is then sutured to a branch of the middle cerebral artery on the surface of the brain and the bone is replaced.
In the EMS (encephalomyosynangiosis) procedure, the temporalis muscle, which is in the temple region of the forehead, is dissected and through an opening in the skull placed onto the surface of the brain.
In the multiple burr holes procedure, multiple small holes (burr holes) are placed in the skull to allow for growth of new vessels into the brain from the scalp.
In the STA-MCA procedure, the scalp artery (superficial temporal artery or STA) is directly sutured to an artery on the surface of the brain (middle cerebral artery or MCA). This procedure is also commonly referred to as an EC-IC (External Carotid-Internal Carotid) bypass.
All of these operations have in common the concept of a blood and oxygen "starved" brain reaching out to grasp and develop new and more efficient means of bringing blood to the brain and bypassing the areas of blockage. The modified direct anastomosis and encephalo-myo-arterio-synangiosis play a role in this improvement by increasing cerebral blood flow (CBF) after the operation. A significant correlation is found between the postoperative effect and the stages of preoperative angiograms. It is crucial for surgery that the anesthesiologist have experience in managing children being treated for moyamoya, as the type of anesthesia they require is very different from the standard anesthetic children get for almost any other type of neurosurgical procedure.
Some of the most up to date treatments for Moyamoya are explained by top rated surgeons at Boston Children's Hospital in Massachusetts in these [9]
Prognosis
The natural history of this disorder is not well known. The long term outlook for patients with treated moyamoya seems to be good. While symptoms may seem to improve almost immediately after the in-direct EDAS, EMS, and multiple burr holes surgeries, it will take probably 6–12 months before new vessels can develop to give a sufficient blood supply. With the direct STA-MCA surgery, increased blood supply is immediate.
Once major stroke or bleeding take place, even with treatment, the patient may be left with permanent loss of function so it is very important to treat this condition promptly.
Dr. Michael Scott, MD discusses the success rate for Moyamoya surgery in [9]
Research
Recent investigations have established that both moyamoya disease and arteriovenous fistulas (AVFs) of the lining of the brain, the dura, are associated with dural angiogenesis. These factors may represent a mechanism for ischemia contributing to the formation of dural AVFs. At least one case of simultaneous unilateral moyamoya syndrome and ipsilateral dural arteriovenous fistula has been reported at the Barrow Neurological Institute. In this case a 44-year-old man presented with headache, tinnitus, and an intraventricular hemorrhage, as seen on computed tomographic scans. Cerebral angiography showed a right moyamoya pattern and an ipsilateral dural AVF fed by branches of the external carotid artery and draining into the transverse sinus. This extremely rare coincidental presentation may have deeper pathogenic implications.[13]
References
- 1 2 3 4 5 6 Moyamoya Disease and Moyamoya Syndrome, R. Michael Scott and Edward R. Smith, New England Journal of Medicine, 360:1226-1237, March 19, 2009
- 1 2 13. Ganesan, V., & Smith, E. R. (2015). Moyamoya: defining current knowledge gaps. Developmental Medicine & Child Neurology, 57(9), 786-787. doi:10.1111/dmcn.12708
- ↑ Wakai K, Tamakoshi A, Ikezaki K, et al. (1997). "Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey". Clin Neurol Neurosurg. 99 Suppl 2: S1–5. PMID 9409395. doi:10.1016/S0303-8467(97)00031-0.
- ↑ Hallemeier C, Rich K, Brubb R, Chicoine M, Moran C, Cross D, Zipfel G, Dacey R, Derdeyn CP (2006). "Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey". Stroke. 37 (6): 1490–1496. PMID 16645133. doi:10.1161/01.STR.0000221787.70503.ca.
- ↑ Janda, Paul; Bellew, Jonathan; Veerappan, Venkatachalam (2009). "Moyamoya disease: case report and literature review". The Journal of the American Osteopathic Association. 109 (10): 547–553. PMID 19861596.
- ↑ Kuriyama S, Kusaka Y, Fujimura M, et al. (2008). "Prevalence and clinicoepidemiological features of moyamoya disease in Japan: findings from a nationwide epidemiological survey". Stroke. 39 (1): 42–7. PMID 18048855. doi:10.1161/STROKEAHA.107.490714.
- ↑ Ma J, Liu Y, Ma L, Huang S, Li H, You C (2013) RNF213 polymorphism and Moyamoya disease: A systematic review and meta-analysis. Neurol India 61(1):35-9. doi:10.4103/0028-3886.107927
- ↑ Smith, E. R. (2012). Moyamoya arteriopathy. Current Treatment Options in Neurology, 14(6), 549-556. doi:10.1007/s11940-012-0195-4
- 1 2 3 Moyamoya disease program: Moyamoya treatment videos | Boston Children's Hospital [Video file]. (n.d.). Retrieved from http://www.childrenshospital.org/centers-and-services/programs/f-_-n/moyamoya-disease-program/patient-resources/videos-about-moyamoya/moyamoya-treatment-videos
- 1 2 3 4 5 Smith, E. R. (2015). Moyamoya biomarkers. Journal of Korean Neurosurgical Society, 57(6), 415. doi:10.3340/jkns.2015.57.6.415
- ↑ 10. Koh, E.-J., Kim, H.-N., Ma, T.-Z., Choi, H.-Y., & Kwak, Y.-G. (2010). Comparative Analysis of Serum Proteomes of Moyamoya Disease and Normal Controls. Journal of Korean Neurosurgical Society, 48(1), 8–13. http://doi.org/10.3340/jkns.2010.48.1.8
- ↑ Kawakami A, Aikawa M, Alcaide P, Luscinskas FW, Libby P, Sacks FM. Apolipoprotein CIII induces expression of vascular cell adhesion molecule-1 in vascular endothelial cells and increases adhesion of monocytic cells. Circulation. 2006;114:681–687.
- ↑ Killory BD, Gonzalez LF, Wait SD, Ponce FA, Albuquerque FC, Spetzler RF (Jun 2008). "Simultaneous unilateral moyamoya disease and ipsilateral dural arteriovenous fistula: case report". Neurosurgery. 62 (6): E1375–6; discussion E1376. PMID 18824958. doi:10.1227/01.neu.0000333311.87554.9c.
External links
- https://stanfordhealthcare.org/medical-clinics/moyamoya-center.html
- http://www.moyamoya.com
- http://www.mir.wustl.edu/research/internal.asp?NavID=707
- http://www.kispi.uzh.ch/Kinderspital/Chirurgie/Chirurgie-1/Neurochirurgie/Moyamoya_en.html
- Orphanet's disease page on Moyamoya disease
- http://www.childrenshospital.org/moyamoya