Benign lymphoepithelial lesion
| Benign lymphoepithelial lesion | |
|---|---|
| Classification and external resources | |
| Specialty | gastroenterology |
| ICD-10 | K11.8 |
| ICD-9-CM | 527.1 |
| DiseasesDB | 8218 |
| MeSH | D008882 |
Benign lymphoepithelial lesion is a type of benign enlargement of the parotid and/or lacrimal glands. This pathologic state is sometimes, but not always, associated with Sjögren's syndrome.
Eponym
Historically, bilateral parotid and lacrimal gland enlargement was characterized by the term Mikulicz's disease if the enlargement appeared apart from other diseases. If it was secondary to another disease, such as tuberculosis, sarcoidosis, lymphoma, and Sjögren's syndrome, the term used was Mikulicz's syndrome. Both names derive from Jan Mikulicz-Radecki, the Polish surgeon best known for describing these conditions.[1][2]
In more recent times, the terms "Mikulicz's disease" and "Mikulicz's syndrome" were viewed as ambiguous and outdated by some sources.[3]
Today Mikulicz's disease is considered to be a subtype of IgG4-related disease, usually accompanied by involvement of one or more other organs in the body.[4]
Locations
In 80% of cases, the parotid gland is affected. Lacrimal glands are also affected.
Characteristic
Benign lymphoepithelial lesion is most likely to occur in adults around 50 years of age. There is a predilection for gender with 60–80% being female. The gland affected has a diffuse swelling. The swelling can be asymptomatic, but mild pain can also be associated. There is a preponderance of this disease in those who suffer from HIV infection.
Most cases of benign lymphoepithelial lesions appear in conjunction with Sjögren's syndrome. When Sjögren's syndrome is present, the swelling is usually bilateral. Otherwise, the affected glands are usually only on one side of the body.
In many cases, a biopsy is needed to distinguish benign lymphoepithelial lesions from sialadenosis (sialosis).
Histology
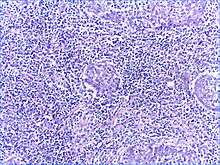
There is a marked lymphoplasmacytic infiltration. Lymphoid follicles surround solid epithelial nests, giving rise to the 'epimyoepithelial islands', that are mainly composed of ductal cells with occasional myoepithelial cells. Excess hyaline basement membrane material is deposited between cells, and there is also acinar atrophy and destruction.
Treatment
Treatment usually consists of observation unless the patient has concern, there is pain, drainage, or other symptoms related to the lesion. Surgical removal of the affected gland would be recommended in those cases. Another treatment option would be aspiration, which can be repeated multiple times. This is commonly performed in those who are debilitated or in those whose benefit from surgery would be outweighed by the risks. Prognosis is usually good; rarely this condition may devolve into lymphoma, or could actually represent 'occult' lymphoma from the outset.
See also
References
- ↑ synd/2087 at Who Named It? - "Mikulicz's disease"
- ↑ synd/2088 at Who Named It? - "Mikulicz's syndrome"
- ↑ Ihrler S, Harrison J (2005). "Mikulicz's disease and Mikulicz's syndrome: analysis of the original case report of 1892 in the light of current knowledge identifies a MALT lymphoma.". Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 100 (3): 334–9. PMID 16122662. doi:10.1016/j.tripleo.2005.01.016.
- ↑ John H. Stone; Arezou Khosroshahi; Vikram Deshpande; John K. C. Chan; J. Godfrey Heathcote; Rob Aalberse; Atsushi Azumi; Donald B. Bloch; William R. Brugge; Mollie N. Carruthers; Wah Cheuk; Lynn Cornell; Carlos Fernandez-Del Castillo; Judith A. Ferry; David Forcione; Günter Klöppe; Daniel L. Hamilos; Terumi Kamisawa; Satomi Kasashima; Shigeyuki Kawa; Mitsuhiro Kawano; Yasufumi Masaki; Kenji Notohara; Kazuichi Okazaki; Ji Kon Ryu; Takako Saeki; Dushyant Sahani; Yasuharu Sato; Thomas Smyrk; James R. Stone; Masayuki Takahira; Hisanori Umehara; George Webster; Motohisa Yamamoto; Eunhee Yi; Tadashi Yoshino; Giuseppe Zamboni; Yoh Zen; Suresh Chari (October 2012). "Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations". Arthritis & Rheumatism. 64 (10): 3061–3067. PMID 22736240. doi:10.1002/art.34593.
- Bibliography
- Kahn, Michael A. Basic Oral and Maxillofacial Pathology. Volume 1. 2001.
- Regezi, Joseph A. Oral Pathology: Clinical Pathologic Correlations. 4th ed. 2002.
Further reading
- Kahn, LB (Jan 1979). "Benign lymphoepithelial lesion (Mikulicz's disease) of the salivary gland: an ultrastructural study.". Human pathology. 10 (1): 99–104. PMID 428999. doi:10.1016/S0046-8177(79)80077-5.
- Lee S, Tsirbas A, McCann J, Goldberg R (2006). "Mikulicz's disease: a new perspective and literature review.". Eur J Ophthalmol. 16 (2): 199–203. PMID 16703534.
- Tsubota, K; Fujita, H; Tsuzaka, K; Takeuchi, T (Jun 2000). "Mikulicz's disease and Sjögren's syndrome.". Investigative Ophthalmology & Visual Science. 41 (7): 1666–73. PMID 10845583.
- Azzopardi, JG; Evans, DJ (Nov 1971). "Malignant lymphoma of parotid associated with Mikulicz disease (benign lymphoepithelial lesion)" (PDF). J Clin Pathol. 24 (8): 744–752. PMC 477147
 . PMID 4943296. doi:10.1136/jcp.24.8.744.
. PMID 4943296. doi:10.1136/jcp.24.8.744. - Yamamoto, M; Harada, S; Ohara, M; Suzuki, C; Naishiro, Y; Yamamoto, H; Takahashi, H; Imai, K (Feb 2005). "Clinical and pathological differences between Mikulicz's disease and Sjögren's syndrome.". Rheumatology (Oxford, England). 44 (2): 227–34. PMID 15509627. doi:10.1093/rheumatology/keh447.
- Delaney, William E.; Balogh, Károly. "Carcinoma of the parotid gland associated with benign lymphoepithelial lesion (Mikulicz's disease) in Sjögren's syndrome". Cancer. 19 (6): 853–860. doi:10.1002/1097-0142(196606)19:6<853::AID-CNCR2820190617>3.0.CO;2-N.
External links
- Mikulicz syndrome on The National Organization for Rare Disorders (NORD)
- Benign lymphoepithelial lesions on Radiopedia