Marcus Gunn pupil
| Relative Afferent Pupillary Defect (RAPD) | |
|---|---|
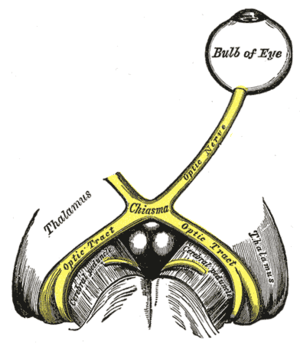 | |
| The left optic nerve and the optic tracts. A Marcus Gunn pupil indicates an afferent defect, usually at the level of the retina or optic nerve. Moving a bright light from the unaffected eye to the affected eye would cause both eyes to dilate, because the ability to perceive the bright light is diminished. | |
| Classification and external resources | |
| DiseasesDB | 29599 |
Relative afferent pupillary defect (RAPD) or Marcus Gunn pupil is a medical sign observed during the swinging-flashlight test[1] whereupon the patient's pupils constrict less (therefore appearing to dilate) when a bright light is swung from the unaffected eye to the affected eye. The affected eye still senses the light and produces pupillary sphincter constriction to some degree, albeit reduced.
The most common cause of Marcus Gunn pupil is a lesion of the optic nerve (between the retina and the optic chiasm) or severe retinal disease. It is named after Scottish ophthalmologist Robert Marcus Gunn.[2] A second common cause of Marcus Gunn pupil is a contralateral optic tract lesion, due to the different contributions of the intact nasal and temporal hemifields.[3]
Examination
The Marcus Gunn pupil is a relative afferent pupillary defect indicating a decreased pupillary response to light in the affected eye.[3]
In the swinging flashlight test, a light is alternately shone into the left and right eyes. A normal response would be equal constriction of both pupils, regardless of which eye the light is directed at. This indicates an intact direct and consensual pupillary light reflex. When the test is performed in an eye with an afferent pupillary defect, light directed in the affected eye will cause only mild constriction of both pupils (due to decreased response to light from the afferent defect), while light in the unaffected eye will cause a normal constriction of both pupils (due to an intact efferent path, and an intact consensual pupillary reflex). Thus, light shone in the affected eye will produce less pupillary constriction than light shone in the unaffected eye.
A Marcus Gunn pupil is distinguished from a total CN II lesion, in which the affected eye perceives no light. In that case, shining the light in the affected eye produces no effect.
Anisocoria is absent. A Marcus Gunn pupil is seen, among other conditions, in optic neuritis. It is also common in retrobulbar optic neuritis due to multiple sclerosis but only for 3–4 weeks, until the visual acuity begins to improve in 1–2 weeks and may return to normal.[4]
See also
- Argyll Robertson pupil
- Adie syndrome
- Anisocoria
- Cycloplegia
- Miosis
- Parinaud's syndrome
- Syphilis
- Pupillary light reflex
References
- ↑ "Pupillary Responses". Stanford University School of Medicine. Retrieved 2015-11-04.
- ↑ doctor/2687 at Who Named It?
- 1 2 Pearce J (November 1996). "The Marcus Gunn pupil". J. Neurol. Neurosurg. Psychiatr. 61 (5): 520. PMC 1074053
 . PMID 8937350. doi:10.1136/jnnp.61.5.520.
. PMID 8937350. doi:10.1136/jnnp.61.5.520. - ↑ Mumenthaler Neurology 4ed, Thieme 2004, page 486 Demyelinating diseases