Mandibular advancement splint

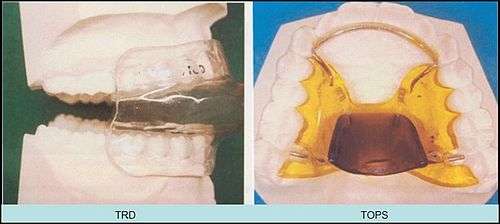

A mandibular splint or mandibular advancement splint (MAS) is a device worn in the mouth that is used to treat orofacial disorders including: obstructive sleep apnea (OSA), snoring, and TMJ disorders. These devices are also known as mandibular advancement devices, sleep apnea oral appliances, oral airway dilators and sleep apnea mouth guards.
Usage
The splint treats snoring and sleep apnea by moving the lower jaw forward slightly, which tightens the soft tissue and muscles of the upper airway to prevent obstruction of the airway during sleep. The tightening created by the device also prevents the tissues of the upper airway from vibrating as air passes over them—the most common cause of snoring.
Mandibular advancement splints are widely used in the United States and are beginning to be used in the UK. Where appropriate, they are considered a good therapy choice as they are non-invasive, easily reversible, quiet, and generally well accepted by the patient. The focus of improvement in appliance design is in reducing bulk, permitting free jaw movement (permitting yawning, speaking, and drinking), and allowing the user to breathe through the mouth (early "welded gum shield"-type devices prevented oral breathing).
Evidence is accumulating to support the use of oral devices in the treatment of OSA, and studies demonstrating their efficacy[1] have been underpinned by increasing recognition of the importance of upper airway anatomy in the pathophysiology of OSA.[2] Oral devices have been shown to have beneficial effects relating to several areas. These include the polysomnographic indexes of OSA, subjective and objective measures of sleepiness, blood pressure, aspects of neuropsychological functioning, and quality of life. Elucidation of the mechanism of action of oral devices has provided insight into the factors that predict treatment response and may improve the selection of patients for this treatment modality.[2]
A 2008 study published in Sleep on the influence of nasal resistance (NAR) on oral device treatment outcome in OSA demonstrates the need for an interdisciplinary approach between ENT surgeons and sleep physicians to treating OSA. The study suggests that higher levels of NAR may negatively affect outcome with MAS[3] and subsequently methods to lower nasal resistance may improve the outcome of oral device treatment.
A meta-analysis of 51 randomized controlled trials investigating the effects of CPAP and oral devices on blood pressure found that oral devices were equally effective as continuous positive airway pressure (CPAP) devices in lowering the blood pressure of patients suffering from OSA.[4] The medical dental sleep appliance, or MDSA, was clinically proven to conclusively show in a large and complex randomized controlled study that CPAP and MAS are effective in treating sleep-disordered breathing in subjects with AHI 5–30. CPAP was thought to be more effective, but randomised control evidence (such as that reviewed in 2013) suggests splints may be as effective in patients with a range of severities of obstructive sleep apnoea.[5] Both methods appear effective in alleviating symptoms, improving daytime sleepiness, quality of life and some aspects of neurobehavioral function, with CPAP usage being less than self-reported MAS usage. More test subjects and their domestic partners felt that CPAP was the most effective treatment, although MAS was easier to use. Nocturnal systemic hypertension was shown to improve with MAS but not CPAP, although the changes are small.[6]
Drawbacks
In a survey study of patients, many discontinued use because of discomfort, lack of efficacy or switching to CPAP and frequent side-effects included dry mouth, tooth pain, and jaw pain.[7] Long term use is not associated with temporamandibular disorders but was associated with permanent changes in how the upper and lower teeth meet and the appliances needed about 0.8 repairs/relines per year.[8] Some patients can find these devices somewhat uncomfortable, although many patients find them less bothersome than CPAP mask treatment. CPAP manufacturers claim that improperly fitted devices may cause teeth to shift over time, like with CPAP, but cite no evidence to support these claims Patients may pay around $1900 out of pocket to secure these devices,[9] and some health plans do not cover these costs.[10] The high price for prescription devices has led to a proliferation of lower cost non-prescription devices that are unproven and some sleep specialists suggest may be dangerous.[11]
See also
- Dental braces
- Oral and maxillofacial surgery
- Orthognathic surgery
- Prosthodontics
- Trismus
References
- ↑ Rose E. (2004). "Identifying the Ideal Oral Appliance Candidate". Journal of Orofacial Orthopedics. 65: 6.
- 1 2 Chan AS, Lee RW, Cistulli PA; Lee; Cistulli (August 2007). "Dental appliance treatment for obstructive sleep apnea". Chest. 132 (2): 693–9. PMID 17699143. doi:10.1378/chest.06-2038.
- ↑ Zeng B, Ng AT, Qian J, Petocz P, Darendeliler MA, Cistulli PA (2008). "Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea". Sleep. 31 (4): 543–547.
- ↑ Daniel, Bratton J; Gaisl, Thomas; Wons, Anette M.; Kohler, Malcolm (2015-12-01). "Cpap vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: A systematic review and meta-analysis". JAMA. 314 (21): 2280–2293. ISSN 0098-7484. PMID 26624827. doi:10.1001/jama.2015.16303.
- ↑ Phillips, C. L.; Grunstein, R. R.; Darendeliler, M. A.; Mihailidou, A. S.; Srinivasan, V. K.; Yee, B. J.; Marks, G. B.; Cistulli, P. A. (2013). "Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial". American Journal of Respiratory and Critical Care Medicine. 187 (8): 879–87. PMID 23413266. doi:10.1164/rccm.201212-2223OC.
- ↑ Barnes M, McEvoy RD, Banks S, et al. (September 2004). "Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea". American Journal of Respiratory and Critical Care Medicine. 170 (6): 656–64. PMID 15201136. doi:10.1164/rccm.200311-1571OC.
- ↑ FR, de Almeida; AA, Lowe; S, Tsuiki; R, Otsuka; M, Wong; S, Fastlicht; F, Ryan (2005-04-01). "Long-term compliance and side effects of oral appliances used for the treatment of snoring and obstructive sleep apnea syndrome.". Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 1 (2). ISSN 1550-9389.
- ↑ Martínez-Gomis, Jordi; Willaert, Eva; Nogues, Lluis; Pascual, Maribel; Somoza, Maria; Monasterio, Carmen (2009-10-05). "Five Years of Sleep Apnea Treatment with a Mandibular Advancement Device". The Angle Orthodontist. 80 (1): 30–36. ISSN 0003-3219. doi:10.2319/030309-122.1.
- ↑ "Oral Appliance for Sleep Apnea". sleepassociation.org. Retrieved 28 June 2016.
- ↑ "Managing a Sleep Disorder Long-Term: Will Insurance Cover Your Expenses?". Health.com. Retrieved 28 June 2016.
- ↑ Woolston, Chris (2011-02-28). "Over-the-counter devices probably won't help sleep apnea". Los Angeles Times. ISSN 0458-3035. Retrieved 2016-08-06.
External links
| Wikimedia Commons has media related to Anti-snore prostheses. |