Long-acting beta-adrenoceptor agonist
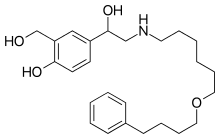
Long-acting β adrenoceptor agonists (LABAs, more specifically, long-acting β2 adrenergic receptor agonists) are usually prescribed for moderate-to-severe persistent asthma patients or patients with chronic obstructive pulmonary disease (COPD). They are designed to reduce the need for shorter-acting β2 agonists such as salbutamol (albuterol), as they have a duration of action of approximately 12 hours in comparison with the 4-to-6-hour duration of salbutamol, making them candidates for sparing high doses of corticosteroids or treating nocturnal asthma and providing symptomatic improvement in patients with COPD. With the exception of formoterol, long-acting β2 agonists are not recommended for the treatment of acute asthma exacerbations because of their slower onset of action compared to salbutamol. Their long duration of action is due to the addition of a long, lipophilic side-chain that binds to an exosite on adrenergic receptors. This allows the active portion of the molecule to continuously bind and unbind at β2 receptors in the smooth muscle in the lungs.
Medical uses
When combined with inhaled steroids, β adrenoceptor agonists can improve symptoms.[1][2] In children this benefit is uncertain and they may be potentially harmful.[2] They should not be used without an accompanying steroid due to an increased risk of severe symptoms, including exacerbation in both children and adults.[3][4][5][6] At least with formoterol, an increased risk appears to be present even when steroids are used[7] and this risk has not been ruled out for salmeterol.[8]
Agents
Some of the currently available long-acting β2 adrenoceptor agonists include:
INN: Trade (brand) name
- arformoterol: Brovana (some consider it to be an ultra-LABA)[9]
- bambuterol: Bambec, Oxeol
- clenbuterol: Dilaterol, Spiropent
- formoterol: Foradil, Oxis, Perforomist
- salmeterol: Serevent
- Protokylol
Ultra-LABAs
Several long-acting β adrenoreceptor agonists have a duration of action of 24 hours, allowing for once-daily dosing. They are considered to be ultra-long-acting β adrenoreceptor agonists (ultra-LABAs)[10] and are now approved.
- indacaterol: approved by the European Medicines Agency (EMA) on November 30, 2009,[11] and by Russian FDA-equivalent under the trade name Onbrez Breezhaler. In the United States. it was approved by the Food and Drug Administration (FDA) under the trade name Arcapta Neohaler on July 1, 2011)[12]
- olodaterol: approved in some EU countries and Russia, and by the United States FDA on July 31, 2014 under Striverdi Respimat[13]
- vilanterol is the ultra-LABA not available by itself but only as a component of combination drugs:
- with fluticasone furoate: Breo Ellipta (U.S.), Relvar Ellipta (EU, RU). This second medication in this combination is the synthetic inhaled corticosteroid fluticasone furoate. This product was approved by the FDA on May 2013 as once-daily inhaled therapy for the treatment of chronic obstructive pulmonary disease (COPD)
- with umeclidinium bromide: Anoro Ellipta. Umeclidinium bromide is a long-acting muscarinic antagonist.[14] This combination was approved by the FDA on December 18, 2013[15] for the long-term maintenance treatment of COPD. On March 28, 2014, it was approved in European countries[16] and in Russia[17] under the same trade name
Ultra-LABAs under development
- abediterol (codenamed LAS100977)[18][19]
- salmefamol (salbutamol and para-methoxyamphetamine (PMA) hybrid)
Failed agents
- carmoterol (formerly TA-2005):[19] development terminated[20]
- PF-610355: development terminated[21]
Concerns
While the use of inhaled LABAs are still recommended in asthma guidelines for the resulting improved symptom control,[22] further concerns have been raised, by a large meta-analysis of the pooled results from 19 trials with 33,826 participants, that salmeterol may increase the small risks of asthma deaths, and this additional risk is not reduced with the additional use of inhaled steroids (e.g., as with the combination product fluticasone/salmeterol).[23] This seems to occur because although LABAs relieve asthma symptoms, they also promote bronchial inflammation and sensitivity without warning.[24]
On February 18, 2011, the FDA issued a safety alert for long-acting β agonists.[25]
References
- ↑ Higashi, AS; Zhu S; Stafford RS; Alexander GC (2011). "National trends in outpatient asthma treatment, 1997-2009.". Journal of General Internal Medicine. 26 (12): 1465–70. PMC 3235617
 . PMID 21769507. doi:10.1007/s11606-011-1796-4.
. PMID 21769507. doi:10.1007/s11606-011-1796-4. - 1 2 Ducharme, Francine M; Ni Chroinin, Muireann; Greenstone, Ilana; Lasserson, Toby J (12 May 2010). "Addition of long-acting beta2-agonists to inhaled corticosteroids versus same dose inhaled corticosteroids for chronic asthma in adults and children.". The Cochrane database of systematic reviews (5): CD005535. PMID 20464739. doi:10.1002/14651858.CD005535.pub2.
- ↑ Fanta CH (March 2009). "Asthma". New England Journal of Medicine. 360 (10): 1002–14. PMID 19264689. doi:10.1056/NEJMra0804579.
- ↑ Cates CJ, Lasserson TJ, Jaeschke R (2009). Cates, Christopher J, ed. "Regular treatment with salmeterol and inhaled steroids for chronic asthma: serious adverse events". Cochrane Database Syst Rev (3): CD006922. PMID 19588410. doi:10.1002/14651858.CD006922.pub2.
- ↑ Cates CJ, Cates MJ (2008). Cates, Christopher J, ed. "Regular treatment with salmeterol for chronic asthma: serious adverse events". Cochrane Database Syst Rev (3): CD006363. PMID 18646149. doi:10.1002/14651858.CD006363.pub2.
- ↑ "FDA Drug Safety Communication: New safety requirements for long-acting inhaled asthma medications called Long-Acting Beta-Agonists (LABAs)". FDA. Feb 2010.
Based on the available information, FDA concludes there is an increased risk for severe exacerbation of asthma symptoms, leading to hospitalizations in pediatric and adult patients as well as death in some patients using LABAs for the treatment of asthma. The agency is requiring the REMS and class-labeling changes to improve the safe use of these products.
- ↑ Cates, CJ; Cates, MJ (Apr 18, 2012). "Regular treatment with formoterol for chronic asthma: serious adverse events.". Cochrane database of systematic reviews (Online). 4: CD006923. PMID 22513944. doi:10.1002/14651858.CD006923.pub3.
- ↑ Cates, CJ; Cates, MJ (Jul 16, 2008). "Regular treatment with salmeterol for chronic asthma: serious adverse events.". Cochrane database of systematic reviews (Online) (3): CD006363. PMID 18646149. doi:10.1002/14651858.CD006363.pub2.
- ↑ Matera, MG; Cazzola, M (2007). "Ultra-Long-Acting β2-Adrenoceptor Agonists: An Emerging Therapeutic Option for Asthma and COPD?". Drugs. 67 (4): 503–15. PMID 17352511. doi:10.2165/00003495-200767040-00002. Retrieved 7 March 2016.
- ↑ Cazzola M, Matera MG, Lötvall J (July 2005). "Ultra long-acting beta 2-agonists in development for asthma and chronic obstructive pulmonary disease". Expert Opin Investig Drugs. 14 (7): 775–83. PMID 16022567. doi:10.1517/13543784.14.7.775.
- ↑ European Public Assessment Report for Onbrez Breezhaler
- ↑ "FDA approves Arcapta Neohaler to treat chronic obstructive pulmonary disease" (Press release). U.S. Food and Drug Administration. 2011-07-01. Retrieved 2011-07-02.
- ↑ "New once-daily Striverdi (olodaterol) Respimat gains approval in first EU countries". Boehringer-Ingelheim. 18 October 2013.
- ↑ "Incruse Ellipta (umeclidinium inhalation powder) for Oral Inhalation Use. Full Prescribing Information" (PDF). GlaxoSmithKline, Research Triangle Park, NC 27709. Retrieved 22 February 2016.
- ↑ "FDA approves Anoro Ellipta to treat chronic obstructive pulmonary disease". U.S. Food and Drug Administration. Retrieved 25 March 2016.
- ↑ "Assessment report: Anoro. INN: umeclidinium bromide/vilanterol" (PDF). European Medicines Agency. Retrieved 25 March 2016.
- ↑ "State Register of Nedicines: Anoro Ellipta (vilanterol + umeclidinium bromide)". Russian State Register of Medicinal Products (in Russian). Retrieved 25 March 2016.
- ↑ Beier, J; Fuhr, R; Massana, E; Jiménez, E; Seoane, B; de Miquel, G; Ruiz, S (October 2014). "Abediterol (LAS100977), a novel long-acting β2-agonist: Efficacy, safety and tolerability in persistent asthma". Respiratory Medicine. 108 (10): 1424–1429. PMID 25256258. doi:10.1016/j.rmed.2014.08.005. Retrieved 25 March 2016.
- 1 2 Cazzola, Mario; Luigino Calzetta; Maria Gabriella Matera3 (May 2011). "β2-adrenoceptor agonists: current and future direction". Br J Pharmacol. 163 (1): 4–17. PMC 3085864
 . PMID 21232045. doi:10.1111/j.1476-5381.2011.01216.x.
. PMID 21232045. doi:10.1111/j.1476-5381.2011.01216.x. - ↑ "Chiesi: Annual Report 2010" (PDF). Chiesi Farmaceutici S.p.A. p. 20. Retrieved 27 March 2016.
- ↑ "AdisInsight: PF 610355". Springer International Publishing AG. Retrieved 25 March 2016.
- ↑ British Thoracic Society & Scottish Intercollegiate Guidelines Network (SIGN). British Guideline on the Management of Asthma. Guideline No. 63. Edinburgh:SIGN; 2004. (HTML, Full PDF, Summary PDF)
- ↑ Salpeter S, Buckley N, Ormiston T, Salpeter E (2006). "Meta-analysis: effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths". Ann Intern Med. 144 (12): 904–12. PMID 16754916. doi:10.7326/0003-4819-144-12-200606200-00126.
- ↑ Krishna Ramanujan (June 9, 2006). "Common asthma inhalers cause up to 80 percent of asthma-related deaths, Cornell and Stanford researchers assert". ChronicalOnline - Cornell University.
- ↑ "Safety Alerts for Human Medical Products > Long-Acting Beta-Agonists (LABAs): New Safe Use Requirements". U.S. Food and Drug Administration. Retrieved 25 March 2016.