Ascaris suum
| Ascaris suum | |
|---|---|
 | |
| Scientific classification | |
| Kingdom: | Animalia |
| Phylum: | Nematoda |
| Class: | Chromadorea |
| Order: | Ascaridida |
| Family: | Ascarididae |
| Genus: | Ascaris |
| Species: | A. suum |
| Binomial name | |
| Ascaris suum (Goeze, 1782) | |
Ascaris suum, also known as large roundworm of pigs, is a parasitic nematode that causes ascariasis in pigs. While roundworms in pigs and humans are today considered as two species, A. suum and A. lumbricoides, with different hosts, cross infection between humans and pigs is possible, so researchers have argued they are the same species.[1] Ascariasis is associated with contact to pigs and pig manure in Denmark.[2]
A. suum is distributed worldwide and grows up to 40 cm (16 in) in length. Ascaris infections are treated with ascaricides. A. suum is in the family Ascarididae, and is one of the oldest associations to mankind.
Life cycle
Pigs get infected with A. suum by ingesting infectious parasite eggs that are present in the environment. The larvae of Ascaris complete two moults within the egg and therefore, the larvae emerging from the egg is not a second stage larva (L2) as was previously presumed, but rather a third stage larva (L3) covered by a loosened L2 cuticle.[3] The larvae hatch from the egg inside the intestines and subsequently start their migration through the body of the pig. First they penetrate the intestinal wall at the level of the caecum/colon [4] and use the mesenterial blood veins to migrate to the liver. After borrowing their way through the liver tissue, they again use the efferent blood stream to carry them to the lungs. There, they get stuck in the capillaries surrounding the lungs and they penetrate the lung alveoli. It takes approximately 7 days to reach the lungs. Once the larvae are inside the lung, they migrate up the respiratory tree and are eventually coughed up and swallowed by the host to reach the small intestine again as soon as 10 days after infection. There, the larvae undergo their first molt inside the host to reach the L4 stage by day 14 post infection. Around day 25 post infection they develop into the L5 stage. Worms reach adulthood 6 weeks after infection and when both female and male worms are present in the same host, fertilized eggs are produced and secreted by the female worm. These eggs are then excreted together with the faeces. After an incubation period, infective stage larvae develop in the eggs and are ready to cause infection in a new host.
Paratenic hosts ingest the eggs and the L3 larvae remain in the tissues of the paratenic host until a pig eats them. These may include beetles and earthworms, as well as large to jumbo chicken eggs from at-risk fowl.
Morphology
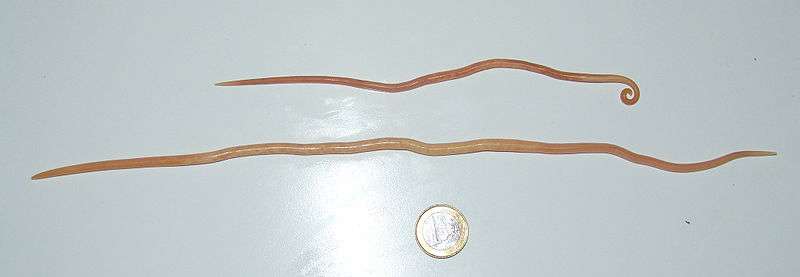
Males are about 15–31 cm (6–12 in) long, and 2–4 mm (0.1–0.2 in) wide. The posterior end is curved toward the ventral side with a pointed tail. They have simple spicules that measure 2.0–3.5 mm (0.08–0.14 in) long. Females are larger than males, measuring 20–49 cm (8–19 in) long and 3–6 mm (0.12–0.24 in) in diameter. From the anterior end, the vulva occupies about one-third of the body length. In addition to their large size, these species also have the three prominent lips. Each lip contains a dentigerous ridge, and no interlabia or alae. Females can lay up to 200,000 eggs per day, and their uteri can contain up to 27 million eggs at a time. Fertilized eggs are ovoid, ranging from 45 to 75 µm length and 35 to 50 µm in diameter. The uterine wall contributes to the lumpy and thick outer layer of the egg. The mammillated layer is stained golden-brown by the bile when the eggs are passed in faeces. Females can also deposit unfertilized eggs that are narrower and longer than normal fertilized eggs, ranging from 88 to 94 µm in length, and 44 µm diameter. Only the proteinaceous layer can be seen in unfertilized eggs, because after fertilization, the vitelline, chitinous, and lipid layers form.[5]
Epidemiology

Presumably, A. suum infections are present in pig farms all over the world. However, few countries have up-to-date information on its prevalence. In a Swedish study it appeared that the pens of sows and fatteners are the heaviest infected environments.[6] This was shown by the presence of eggs in old faecal deposits collected from the pens. These findings were supported by studies from China and Denmark where the highest prevalence of A. suum was also found in breeding sows and fatteners.[7][8] The prevalence in breeding boars is usually lower than in sows or fatteners. Nevertheless, infected boars could also be an important source of transmission of parasite eggs on the farm since they are often located in more traditional pens than the sows (e.g. with solid floor and/or bedding). Moreover, boars are regularly used for contact stimulation of the sows, which allows them to spread the infection by defecating in areas other than their own pen. Strong evidence exists that under indoor conditions, massive infection of piglets with A. suum usually occurs shortly after arrival in the highly infectious fattening units and not in the farrowing pens.[6][8][9] Several studies have shown that A. suum egg excretion was nearly absent in weaners despite the, sometimes substantial, presence of eggs in the farrowing pens of intensive herds.[7][10] Here, the increased hygienic standards in combination with the low humidity in the farrowing pens may significantly reduce the presence of favourable microenvironments for egg survival. On the other hand, in piglets raised under outdoor conditions, significant transmission is thought to occur soon after birth and pigs are infected before fattening.[8][11]
There are three major reasons why Ascaris is still so prevalent in current high intensity pig farms. First, because it has a direct life cycle, and is therefore not reliant on other organisms for its transmission to new hosts. Second, the female parasitic worms are highly fecund and are capable of producing hundreds of thousands of eggs per day that contaminate the surroundings instantaneously. One study showed that pigs that are naturally exposed to a paddock contaminated with A. suum have the highest egg excretion approximately 17 weeks after being introduced onto the paddock. After this point, egg counts seem to drop again.[12] The lifespan of adult A. suum worms can be over 1 year, which is significantly longer than the average lifespan of a fattening pig these days. Therefore, once adult worms are present in fattening pigs, egg shedding increases with the age of the pigs unless the worms are cleared from the intestine by anthelmintic therapy. Third, the eggs of A. suum are generally considered to be highly resistant to external environmental factors suggesting their possible survival for up to several years in the appropriate conditions. So, even if parasitic worms are flushed from the intestine by anthelmintic drugs (which do not have a remanent effect), the pig keeps on reinfecting itself continuously since it is present in a highly contaminated environment. This ensures the establishment of fresh infections very rapidly after treatment. These factors, together with the seemingly unimportant health consequences of A. suum infections have led to a certain negligent attitude towards roundworm infections on the part of the farmer.
Pathogenesis
Pigs that are infected with A. suum, sometimes carry numerous adult worms in their intestine. Yet, these pigs do not show any disease specific symptoms and are indistinguishable from uninfected pigs. Clinical signs such as breathing difficulties and wheezing, and indirect signs like decreased growth rate and overall lower food conversion efficiency are not specific and therefore seldom associated with ascariosis by the farmer. Although the presence of adult parasites in the small intestine might affect the pig’s productivity,[13] it does not appear to affect the pig’s health significantly. The larval stages of this parasite on the other hand, do cause significant damage to the internal organs of its host in their attempt to successfully complete their hepatopulmonary migration.

In the liver, the inflammatory reaction to this damage is manifested as the so-called ‘white spots’ that are visible on the surface of the liver. Hepatic white spots are the most characteristic lesions caused by migrating A. suum larvae in pigs. After larvae migrated through the liver, the destroyed liver cells are replaced by interlobular depositions of fibrous tissue and cellular infiltrates, producing the typical white spots.[14][15] Three types of white spots have been described: compact and mesh-worked white spots both produced by eosinophilic interstitial hepatitis and the lymphonodular type spots caused by lymphofollicular hyperplasia. White spots appear as early as 3 days post infection and start to resolve after about 2–3 weeks post infection.[16][17] As a result of this, livers can appear normal about 35 days after primary inoculation with Ascaris eggs.[18] In order to complete their hepatopulmonary migration, larvae need to pass through the lungs as well. As these larvae move into the alveolar and bronchial air spaces they cause direct physical damage to the lungs. This can subsequently promote the development of pneumonia or pleurisy. The damage to the respiratory system can be recorded at the slaughterhouse and has been associated with the presence of Ascaris infection.[19] It is obvious that the severity of the damage will depend on the amount of larvae that migrate through the lung [20] and that increased infection levels can easily cause respiratory distress and coughing. However, even after ingestion of high amounts of eggs, the A. suum infection itself very seldom causes lethal damage to the lung. It is rather the secondary, opportunistic, bacterial or viral infections that increase the chances of severe health problems.
Economic importance of pig ascariasis
Infections with A. suum, and especially the larval migration phase, have shown to reduce the economic profitability of a pig farm.[21] The presence of this parasite on a pig farm reduces its productivity in a number of direct or indirect ways. Perhaps the most obvious of which is the condemnation of the livers that are visibly affected by parasite migration. Whether the liver is trimmed or fully condemned evidently depends on the amount of white spots detected on the liver. At the level of the lung, the passage of ascarid larvae is associated with impaired pulmonary bacterial clearance [22] making it easier for secondary bacterial and viral infections to settle. Increased susceptibility to Pasteurella multicoda, Escherichia coli and Salmonella spp. have already been associated with ascariosis.[23][24][25] Moreover, a recent study also observed a significant negative effect of A. suum infection on the seroconversion and antibody levels to a Mycoplasma hyopneumoniae vaccine.[26] Not only the negative effects of these diseases on the productivity but also the costs of their treatment indirectly contributes to the effect of ascariosis.
The decreased health status of pigs, as a consequence of roundworm infection, is reflected in general production parameters like daily weight gain, feed conversion efficiency and meat quality. However, in farms with low infection levels, the effect of infection is expected to be minimal and the economical profitability of active Ascaris control can be questioned.[27] It is difficult to determine the economical losses due to parasites that are not lethal. There are numerous interactions between the worm, the host, the presence of other diseases, the production system and many other factors. Recent evaluations of the economical performance of infected pig farms has indicated that the improved feed conversion, increased daily weight gain, lower mortality and better carcass quality act in a synergetic way. Hence, strategic deworming should result in a win-win effect on economic and environmental performances with gross profit margin increases of 3 to 12 euro per average present finisher per year.[28][29][30] To distinguish between pig populations that suffer significant economical damage and those that are less affected, we depend on the availability of diagnostic tools to provide us with information on the presence and infection pressure of this parasite on a farm. If interpreted correctly, diagnostic tools can be of use to evaluate the applied control strategies and see whether efforts for parasite control need to be increased or changed.
Diagnosis
Infections with A. suum very seldom cause clinical disease and therefore typically remain unrecognized by farmers and veterinarians. To be able to evaluate the evolution of the infection status and therefore the efficacy of the applied control strategies, the use of correct diagnostic tools is crucial. The presence of A. suum infections on pig farms can be investigated in different ways. First, the presence of adult worms in the faeces and general clinical signs including coughing, rapid shallow breathing, unthriftiness, and weight loss or reduced weight gain could indicate the presence of Ascaris on the farm. In the laboratory, serum or faecal samples can be investigated to detect antibodies or parasite eggs respectively. Finally, at the slaughterhouse, the presence of worms in the intestine and the number of affected livers and lungs also provide information on the ‘Ascaris-status’ of a farm.
Coprological examination
The number of eggs excreted by a pig can give an indication of the worm burden because, in continuously exposed pigs, the quantity of eggs that are shed seems to be correlated with the number of adult worms in the intestine.[19] For this, different coprological techniques can be applied [31] which make use of the buoyancy of parasite eggs to separate them from the faecal debris. For the detection of A. suum eggs, the quantitative McMaster test is generally used. The results of this examination are reported as eggs per gram of faeces or EPG. Although coprological examinations are easy to perform and require relatively cheap materials, the performance of the sampling and the tests are time consuming and not cost-effective nor optimal for the screening of large number of samples. In addition, the correct interpretation of the results of coprological examinations can prove to be a rather difficult exercise. Ascaris populations are strongly aggregated within the pig population with few pigs carrying the majority of the worms while most of the pigs carry few or even no adult worms at all.[32] Because of this, a large number of pigs need to be investigated since there is a significant possibility to have false positive and false negative egg counts. False positives are the result of coprophagia and/or geophagia and their prevalence and magnitude depends on different management and housing factors.[33] The number and range of false-positive A.suum egg counts in pigs can be considerable, but in general, EPG levels lower than 200 should be considered false-positives.[33] However, for diagnosis on farm level, these false positive samples are not as important as the false negatives. False negative results are possible when only immature worms are present or when only worms of a single sex are present. Boes and colleagues [33] have shown that as much as 23% of the investigated pigs that harboured worms in their intestine did not excrete any eggs. Consequentially, prevalence studies that reveal many low A. suum egg counts in pigs should be interpreted with care. Furthermore, the number of adult worms, and therefore the EPG is not representative of the amount of migrating larvae the pig has been exposed to. Regardless of the dose regimen, the numbers of worms that end up in the small intestine is generally inconsistent and independent of the intake of infective stages. Moreover, there seems to exist an inverse relationship between the number of adults found in the intestine and the amount of eggs given during a single experimental infection dose.[34]
White spots on the liver
Another way to estimate Ascaris exposure is to check the degree of white spot formation on swine livers. The development of the so called ‘white spots’ or ‘milk spots’ is caused by migrating larvae and is usually recorded at the slaughterhouse. Although the number of liver lesions indicates the recent passing of migrating A. suum larvae, there exists no relationship whatsoever between the number of lesions and the number of adult parasites that eventually end up in the small intestine (Nilsson, 1982). In a study by Bernardo et al. (1990c), the presence of white spots on the liver is more than twice as prevalent as worms in the small intestine at slaughter. The absence of worms in the intestine when white spots are visible on the liver can mean two things: 1) eggs have recently been ingested, but not enough time had elapsed to allow development of macroscopically detectable ascarids or; 2) infection had been cleared by the host immune response but lesions had not yet resolved.
When milk spots are present, it is likely that A. suum infection is present. The presence of milk spots has a high sensitivity and high negative predictive value as a screening test for ascariosis in individual hogs (Bernardo et al., 1990c). Under continuous exposure, the number of white spots on the liver increases until weeks 6-9, after which there is a gradual decline towards lower levels (Eriksen et al., 1992b). This decline could be attributed to the build-up of immunity as continuous exposure to A. suum infections stimulates the development of strong protective immunity at the level of the intestine, called the prehepatic barrier (Eriksen, 1982; Urban et al., 1988). This would impede freshly acquired larvae from reaching the liver and therefore prevent the formation of white spots. Hence, the number of liver white spots is a poor indicator of long-term A. suum exposure as it only reflects recent larval migration. Livers might therefore look normal or only mildly affected at slaughter even though pigs have been exposed to high numbers of infective eggs during the course of their life. In addition, the visual assessment of livers is very subjective. Especially when pigs with low numbers of white spots are slaughtered, the decision on whether or not an abnormality on the liver is considered a true white spot largely depends on the perception of the person doing the assessment. On top of that, this usually has to be performed within an extremely short time span due to the high speed of slaughter. This supports the variability in the white spot counts and increases doubt on the reliability and uniformity of the data on liver lesions at slaughter.
Serological examination
The use of serological tests is widespread and generally accepted in the pig industry. Tests are available for a number of important bacterial and viral diseases in pigs (e.g. Salmonellosis, Mycoplasma infection, Aujeszky’s disease, PRRS Virus, etc.). However, for Ascaris, a commercial serological test is not available at this moment. The use of a serological method, however, could in theory overcome the difficulties associated with the traditional methods (examination of faeces or livers) of diagnosing ascariosis in pigs. Throughout the different stages of infection, Ascaris worms are in close contact with the host’s immune system and pigs build up antibody responses to worm antigens to which they are exposed.[35] Of all the infective larvae taken up by the host, only few will eventually get to develop into adult parasites due to the immune processes that expel the majority of the larvae during migration and after return to the gut (Helwigh and Nansen, 1999; Roepstorff et al., 1997). Because of this, no correlation between antibody levels and worm load could be detected in naturally infected or trickle-infected pigs (Nejsum et al., 2009b; Roepstorff and Murrell, 1997). As a result, ELISA values do not represent the amount of adult parasites eventually dwelling in the pig’s intestine, but rather reflect the degree of exposure to the parasite; hereby significantly increasing the chance to detect A. suum infected pigs and consequentially making it more sensitive than the conventional diagnostic techniques. Several studies describe the use of an Enzyme Linked ImmunoSorbent Assay (ELISA) for the detection of anti-Ascaris antibodies in the sera of swine. In this regard, the use of different adult and larval extracts or excretory/secretory products and some purified adult proteins have been evaluated [35] (Bogh et al., 1994; Frontera et al., 2003b; Lind et al., 1993; Urban and Romanowski, 1985; Yoshihara et al., 1993). Although most of these tests have shown to be effective in diagnosing A. suum infection, no apparent steps were taken or proposed for future practical application of the developed ELISA’s. Moreover, the studies described above made use of antigen mixtures instead of specific, purified antigens, increasing the likelihood that antibodies to antigens of other pathogens could cross-react.
Control of A. suum on pig farms
Although, the aim of control programs against this parasite should be to eliminate the parasite completely, a significant reduction in transmission intensity will readily result in a marked decrease of adverse effects on the health and productivity of the pig herd. Although, anthelmintic treatment alone, without the support of good general farm management and increased hygienic standards will probably not suffice to effectively control parasitic infections on farms, it is, at this moment, the only available method to clear pigs from roundworm infections.
Anthelmintic treatment
Ever since the advent of broad-spectrum anthelmintics in the 1960’s, treatment of worm infections in pigs has become increasingly reliant on mass-treatment with anthelmintic drugs. When selecting a drug for the control of helminth infections, several things need to be taken into account. Namely, 1) the margin of safety of the used compound, 2) the efficacy of compound against the different stages of the parasite, 3) the spectrum of activity, 4) the mode of administration and last but not least, 5) the cost of the drug. All of the modern anthelmintics are found to be very safe. Treatments with doses exceeding several times the recommended dose could not show any clinical effect in pigs. For the effective control of helminth infections on a pig farm it is advantageous to select an anthelminticum that kills the larval stages and has a broad spectrum of activity. The drugs pyrantel, fenbendazole, flubendazole and levamisole also have shown activity against migrating stages of A. suum (Kennedy et al., 1987; Oakley, 1974; Stewart et al., 1984; Thienpont et al., 1978). Piperazine and pyrantel have restricted activity against the other common porcine nematode infections (Trichuris suis & Oesophagostomum spp.) (Rochette, 1985) and are therefore not the drugs of choice when co-infections with these parasites are present on a farm. Anthelmintics of the macrocyclic lactone family (e.g. ivermectin, doramectin) have a significantly longer residual effect in comparison with the other anthelmintics. Lichtensteiger et al., (1999) reported that the anthelmintic activity of ivermectin persisted for less than 7 days and over 7, but less than 14 days for doramectin. Moreover, these compounds are also highly efficient against ectoparasites like mange mites (Sarcoptes scabiei var suis) and hog lice (Haematopinus suis) (Lee et al., 1980; Lichtensteiger et al., 1999; Logan et al., 1996; Stewart et al., 1981b; Yazwinski et al., 1997). Anthelmintics are available in a variety of formulations. Administration of the drug in either water or feed is the easiest and most economical way, but has the disadvantage of variable dosages being delivered when numbers of pigs are being treated in groups from a single source of medication. Delivery by injection on the other hand, is more accurate in dosage but is time- and labour intensive, which adds to the overall cost of treatment. Injectable anthelmintics have a significantly longer withdrawal period (a minimum of 28 days for doramectin) in comparison with in-feed formulations and are usually conserved for the treatment of the breeding stock (Conder and Baker, 2002). The overall cost of anthelmintic treatment will vary, depending on the choice of anthelmintic, number of treatments, and weight of the animals being treated. In general, for the choice of anthelmintic, pig farmers will base themselves on information received from their veterinarians or feed companies and more importantly, on their previous experiences with a selected anthelmintic (Theodoropoulos et al., 2001). To date, no studies have reported anthelminticum resistance in A. suum in pigs. Whether anthelmintic resistance would be easily induced in A. suum is unknown. However, the development of anthelmintic resistance in Oesophagostomum spp. and in the closely related horse parasite, Parascaris equorum (Boersema et al., 2002; Laugier et al., 2012; Nansen and Roepstorff, 1999; Nareaho et al., 2011) suggests that continued malpractice in this area might eventually lead to anthelmintic resistance in A. suum.
Over time, questions have been raised concerning the long-term impact of the massive application of these highly efficacious, broad-spectrum anthelmintic compounds on the environment. Due to the bioavilability of some of these drugs, high percentages of these substances are being excreted unchanged after oral or systemic administration (Farkas et al., 2003; Plumb, 2008). Decomposing animal excrements/waste is spread all over our land for increased crop productivity, hereby also spreading the anthelmintic drugs and their residues. To this day however, we remain oblivious to what the possible long-term ecological effects of these drugs and their residues are on pasture fauna and flora (Spratt, 1997). This concern, among others, is stimulating the need for alternative, more biological measures of parasite control. In biological farming, the use of traditional synthetic drugs is not allowed and therefore, organic farmers prefer a phytopharmaceutical approach for the control of parasitic infections on their farm (van Krimpen et al., 2010). Although many plants are suggested to have some nematocidal effects (Chitwood, 2002), recent studies by van Krimpen et al., (2010) could not show any significant reduction on the worm load of infected pigs after treatment with a herb mixture (Thymus vulgaris, Melissa officinalis and Echinacea purpurea), Papaya fruits, Bolbo leaf or complete Artemesia plants in comparison with untreated controls. Nevertheless, continued efforts could be made to standardize the plant extracts with good anthelmintic activity and formulate best alternative herbal preparations to replace or complement the synthetic drugs, which are currently in use. In addition to phytopharmaceutical research, the possibility of using nematophageous fungi for the biological control of A. suum is currently being investigated. According to the study of Ferreira et al., (2011) mycelia of Pochonia chlamydosporia, which were added to the food of pigs, showed ovicidal activity against A. suum eggs after passage through the gastrointestinal tract.
Treatment program
Routine anthelmintic treatments, commonly used in intensive pig rearing systems, are not systematic and treatment schemes vary according to farm and animal category. The breeding stock is usually treated with 3-4 month intervals or prior to farrowing. (Roepstorff and Nansen, 1994). Piglets are typically treated upon entering the fattening units and maybe once more halfway the fattening period. However, these treatment schemes seem to be unable to significantly decrease the infection intensity on a farm. Treatment frequency must be based on the prepatent period of the worm species. For Ascaris this is 42 days. However, when anthelmintic treatment is ineffective i/n killing the migrating larval stages, it is possible that egg shedding occurs earlier as larvae remain in the lung up to 10 days post infection (Roepstorff et al., 1997). Treatment of pigs every 5 weeks would therefore eliminate the worms before they are able to produce millions of eggs and contaminate the environment all over again. When a strict deworming process is applied, the infectivity of the environment will drop, as new hosts will take up eggs from the environment, and eggs will be swept away by cleaning actions or eventually lose their viability. This will ultimately result in a stock of pigs with a reduced or absent parasitic burden. It is important to understand that persistence in the repeated application of the anthelmintic is necessary. If the environmental contamination is high, it will most likely take several fattening rounds to eventually reduce the infection pressure (Bakker, 1984; Jourquin, 2007). Both the fact that infections usually seem to occur in the fattening units and the fact that anthelmintic treatment has limited persistent activity against recurring infectious larvae lead to believe that the common practice of treating pigs prior to, or upon arrival in the fattening units, might be superfluous. In two experiments, it has been reported that a single anthelmintic treatment of fatteners at the start of the fattening period is not justified on economie grounds. It showed to be ineffective in reducing parasite prevalence and it did not have a positive effect on performance results, nor did it influence the incidence of other lesions like white spots (Boes et al., 2010; Nilsson, 1982; Roepstorff and Jorsal, 1990). More importantly, Roepstorff (1997) showed that, depending on the infection status, it might sometimes be more economically beneficial to switch from a routine anthelmintic treatment program to the conditional usage of anthelmintics, treating only when parasite levels reach an unacceptable level. This should however be supported by routine diagnostic screening of pigs from different age categories and is probably only applicable to farms with moderate to highly intensive management.
Management Practices
Routine applications of anthelmintic drug seem to appeal to pig farmers for reasons of convenience (Nansen and Roepstorff, 1999). However, merely resorting to anthelmintic treatment could result in little or no improvement due to continuous reinfection. The use of anthelmintics therefore needs to be complemented by higher quality farm hygiene and more effective farm management practices if one strives to reduce the roundworm infection pressure on the farm. There are numerous aspects of farm management that can have a major impact on the epidemiology of A. suum. Undoubtedly, the type of production system, stable infrastructure and different management factors like the application of a quarantine for imported pigs, all-in-all-out practice, early weaning, and the efficiency of cleaning protocols will affect Ascaris epidemiology. The type of production system that is in use will be a key factor regarding the infection intensity on a farm (Nansen and Roepstorff, 1999). For obvious reasons, there is a higher diversity of parasite species and higher infection intensity on traditional farms and where pigs have access to outdoor facilities when compared to intensive indoor systems (Lai et al., 2011; Roepstorff and Nansen, 1994). Reducing contact of pigs with their own faecal deposits or from pigs from previous rounds is important. Consequentially, housing of pigs on slatted floors seems to reduce the chance of parasite infestation compared to solid or partially slatted floors (Roepstorff and Jorsal, 1990; Sanchez-Vazquez et al., 2010; Tielen et al., 1978). Increased risk is associated with bedding being present in the pens. The use of bedding material may provide extra refugia that promote egg embryonation and hamper the effectiveness of repeated cleaning and disinfection measures. Evidently, the stocking density in the pig house will also be important (Tielen et al., 1978), as chances of pens containing pigs with patent infections will increase. Positioning the water supply in the dung area instead of in the lying area or the feeding troughs seems to be associated with a decreased prevalence of A. suum (Roepstorff et al., 1999). Water spillage in areas where eggs are present will enhance the chances for survival of the eggs due to constant humidity. Despite the extremely rigid eggshell, eggs do not embryonate when relative humidity is low, for instance in the dry resting areas in pig pens, or when floor temperatures are lower than 15 °C. Additionally, pig urine also seems to exhibit a strong inhibitory effect on the development of A. suum eggs (Nilsson, 1982). Once in the environment, the eggs will embryonate until the infective larvae are present inside the egg. Only then, the egg is infective for a new host. In a Danish study it was shown that A. suum eggs could embryonate on a pasture within 4–6 weeks during a normal Danish summer (Roepstorff and Murrell, 1997). These results were supported by experiments in laboratory conditions, during which it was observed that, although motile larvae were noticed from 4 weeks post-incubation, an incubation period of at least 6 weeks at room temperature was needed for eggs to become infective in mice (Geenen et al., 1999). When environmental factors like temperature, oxygen availability and relative humidity are suboptimal, the time for larvae to become infective increases (Nilsson, 1982). This is reflected by the fact that white spot levels seem to vary within farms depending on the season. Presumably, the rising temperatures in spring and summer allow the eggs that have overwintered in the stables to massively develop into the infective larval stage, leading to heavier infective environments and subsequently higher liver condemnation rates in summer and early autumn (Lai et al., 2011; Menzies et al., 1994; Nilsson, 1982; Sanchez-Vazquez et al., 2012). In intensive indoor systems, the presence of a breeding stock on a farm seems to be associated with a lower chance of A. suum being present on the farm. More often than not, farmers are unaware of the parasite status of the pigs that are bought from external producers. Therefore, importing pigs from piglet producers evidently increases the risk of introducing new infections into the herd. Farmers with fattening herds are advised to buy piglets from larger piglet producers with good management and hygiene (Joachim et al., 2001b) and that were preferably treated prior to delivery. Whether weaners need to be treated at the beginning of fattening or not is open for discussion. However, if their worm-free status cannot be warranted, incoming pigs should be treated upon arrival, hereby reducing the risk of introducing the infection into their herd. Once A. suum is present on the farm, it is easily dispersed over the whole farm through moving animals and dirty materials and boots. Even flies have shown to carry A. suum eggs (Forster et al., 2009). Other management practices like the use of the all-in-all-out system, and early weaning are linked to lower prevalence of A. suum (Joachim et al., 2001b; Roepstorff and Jorsal, 1990; Roepstorff et al., 1999; Tielen et al., 1978). In the all-in-all-out production system, pigs are moved into and out of facilities in distinct groups with the hope that, by preventing the commingling of groups, the spread of disease is reduced. This practice also allows for a period of thorough cleaning and disinfecting between subsequent groups of animals. Early weaning of piglets (3–5 weeks) also seems to be associated with a reduced risk of A. suum infection (Roepstorff et al., 1999). However it is likely that this can be attributed to the fact that both these parameters are associated with other factors that are more important for parasite survival, like for instance, the use of more traditional rearing methods or poorer general pen hygiene. Frequent cleaning of the pens, preferably after each round, is indispensable to destroy or reduce the amount of eggs in the environment. Clearly, the presence of rough and uneven surfaces would provide a good microenvironment for egg development and have an impact on the efficiency of cleaning protocols. Joachim et al., (2001) indicated that in older pens, the prevalence of Ascaris infections was significantly higher (63,0%) than in the new pens (27,9%). Moreover, Nilsson (1982) found high number of eggs (up to 3,000 EPG) in the crevices of the floor between the slatted dung area and the resting area of the pen. Approximately half of these eggs appeared to be embryonated. In a study by Beloeil et al., (2003) 31% of the farms surveyed had residual dung in the fattening pens when restocking them with new fattening pigs, a practice, favouring the transmission of A. suum eggs. Even though careful cleaning of the pens with high-pressure water will remove most of the residual dung, it seems ineffective to completely remove all infective eggs (Nilsson, 1982). The use of disinfectants is very effective against bacteria, but is rather ineffective against A. suum eggs. Instead, steam cleaning and drying of the pens is a highly recommended management practice for killing roundworm eggs. These are, however, hard to comply with in practice. Looking to the future, the percentage of Ascaris-favourable production systems is expected to rise due to increasing consumer demand for drug free, biologically grown, free-range pork and the forthcoming implementation of new regulations for increased pig wellbeing. In Denmark for example, sprinkler systems should be applied in the pens of growing pigs and sows to accommodate a daily shower. Moreover, sows should not be tethered and housed in groups in enriched environments (bedding, wallowing) for part of the gestation (Roepstorff et al., 2011a; Thamsborg et al., 2010). As a result, the number of eggs surviving in the pens will increase and with it, the prevalence of Ascaris and other pig parasites (Haugegaard, 2010). Good diagnostic assessments will be necessary to evaluate how these changes in farm management will affect parasite epidemiology.
Vaccination
Pigs build up natural resistance against recurring infections rather quickly. Significant levels of protection were detected in pigs following one or multiple inoculations with infective eggs or L3s of A. suum (Eriksen, 1982; Helwigh and Nansen, 1999). This provides some hope for future vaccination strategies. Developing vaccines against parasites is highly desirable and the search for a vaccine against Ascaris has been on-going for about half a century. Still, their development so far has been very limited and the information gathered on this topic remains scarce. Initial experiments showed that oral immunisation of pigs with eggs that had been UV-irradiated induced high percentages of protection (Tromba, 1978; Urban and Romanowski, 1985; Urban and Tromba, 1982a, 1984). However these high percentages of protection could not be obtained after vaccination with native worm extracts or excretory/secretory (E/S) products (Hill et al., 1994; Rhodes et al., 1988; Urban and Romanowski, 1985) except for Lukes (1992), who was able to obtain a 89% reduction in lung and liver larvae retrieved from mice immunized twice with 100 mg of antigen in a liposome with levamisole as an immunomodulator. Only one study by Serrano et al., (2001) investigated the protective capacity of purified native antigens. All three antigens that were tested (14, 42 and 97 kDa) showed to induce significant levels of protection after 6 weekly immunizations of 1 µg of antigen in Freund’s incomplete adjuvant. Since the year 2000, interest has shifted from the use of native parasite products towards recombinantly produced proteins as vaccine antigens. Different recombinants were expressed in E. coli. The As14 and As16 recombinants coupled to cholera toxin subunit B were administered three times intranasally to mice or pigs and could induce a reduction of approximately 60% in lung stage larvae recovered from the lungs of the vaccinated animals in comparison with their controls (Tsuji et al., 2004; Tsuji et al., 2003; Tsuji et al., 2001). Similarly, immunizing mice by subcutaneous injection with recombinant As24 in Freund’s complete adjuvant induced 58% of protection (Islam et al., 2005). On the other hand, no protection could be produced when the As37 antigen was tested in a similar setup (Tsuji et al., 2002). Attempts have been made to produce larval antigens in rice plants (Matsumoto et al., 2009; Nozoye et al., 2009). Immunizing mice by feeding them transgenic rice showed to elicit an antigen specific antibody response, indicating that the transgenic rice was able to prime the immune response of mice. Orally immunized mice also showed a reduced amount of larvae recovered from the lungs after challenge infection in comparison with non-immunized controls (Matsumoto et al., 2009). In the future, this could provide an easy way of producing and administering parasite antigens. However, this technique should be further optimized and evaluated.
Incidents and outbreaks
In Canada in 1970, a postgraduate student tainted his roommates' food with A. suum. Four of the victims became seriously ill; two of these suffered acute respiratory failure.[36][37]
Genetics
A 273-megabase draft genome for A. suum was published in 2011.[38]
References
- ↑ http://www.parasitesandvectors.com/content/5/1/42
- ↑ http://jcm.asm.org/content/43/3/1142.full
- ↑ Fagerholm et al., 2000, Differentiation of cuticular structures during the growth of the third-stage larva of A suum after emerging from the egg. J Parasitol 86, 421-427.
- ↑ Murrel et al., 1997, J Parasitol 83, 255-260.
- ↑ Larry S. Roberts & John Janovy, Jr. (2008). Foundations of Parasitology (8th ed.). McGraw-Hill. ISBN 978-0-07-131103-8.
- 1 2 Nilsson, 1982; Acta Vet Scan Suppl. 79,1-108.
- 1 2 Lai et al., 2011; Res Vet Sci 91, e121-124.
- 1 2 3 Roepstorff and Nansen, 1994; Vet Parasitol 54,69-85.
- ↑ Beloeil et al., 2003; Livest Prod Sci 81, 99-104.
- ↑ Joachim et al., 2001; Vet Parasitol 96,135-146.
- ↑ Roepstorff and Murrel, 1997; Int J Parasitol 27, 563-572.
- ↑ Mejer and Roepstorff, 2006; Parasitol 133, 305-312.
- ↑ Andersen, 1976, The influence of A. suum infection upon growth rates in pigs; Nord Vet Med 28, 322-330
- ↑ Nakagawa et al., 1983. Pathological studies on white spots of the liver in fattening pigs. Natl Inst Anim Health Q 23, 138-49.
- ↑ Perez et al., 2001. Immunohistochemical characterization of hepatic lesions associated with migrating larvae of A. suum in pigs. J comp Pathol 124, 200-206.
- ↑ Eriksen et al., 1980, Nord Vet Med 32, 233-242.
- ↑ Roepstorff et al., 1997, Parasitol 115, 443-452.
- ↑ Copeman and Gafaar, 1972; Sequential development of hepatic lesions of ascaridosis in colostrum-derived pigs. Aust Vet J 48, 263-68.
- 1 2 Bernardo et al., 1990, Ascariasis, respiratory diseases and production indices in selected Prince Edward Island swine herds. Can J Vet Res 54, 267-273
- ↑ Miskimins et al., 1994. The serious effects of Ascarid larval migration on a group of market-weight swine. Vet Med 89,247-253.
- ↑ Holland, Celia. Ascaris the Neglected parasite. Elsevier. pp. 363–381. ISBN 978-0-12-396978-1.
- ↑ Curtis et al., 1987. Can J Vet Res 51, 525-527.
- ↑ Adedeji et al., 1989, J helminthol 63, 19-24.
- ↑ Smith et al., 2011; Vet Rec 168, 240.
- ↑ Tjornehoj et al., 1992; Parasitol Res 78, 525-528.
- ↑ Steenhard et al., 2009; Vaccine 27, 5161-69.
- ↑ Roepstorff, 1997; Vet Parasitol 73, 139-151.
- ↑ Van Meensel et al., Vet Med-Czech 55, 483-493.
- ↑ Jourquin, 1997; Strategic deworming to boost performance. International Pig Topics 22,7-9.
- ↑ Kanora, 2009; Effect on productivity of treating fattening pigs every 5 weeks with flubendazole in feed. Vlaams Diergeneesk Tijdschr 78, 170-175.
- ↑ Thienpont et al., 1979 Diagnosting helminthiasis through coprological examination, 187p.
- ↑ Boes et al., 1998. Distribution of Ascaris suum in experimentally and naturally infected pigs and comparison with Ascaris lumbricoides infections in hu;ans. Parasitol 117(pt6), 589-596
- 1 2 3 Boes et al., 1997. False=positive Ascaris suum egg counts in pigs. Int J Parasitol 27, 833-838
- ↑ Roepstorff et al., 1997. Experimental Ascaris suum infections in the pig: worm population kinetics following single inoculations with three doses of infective eggs. Parasitol 115, 443-452.
- 1 2 Roepstorff, A. (1998-07-01). "Natural Ascaris suum infections in swine diagnosed by coprological and serological (ELISA) methods". Parasitology Research. 84 (7): 537–543. ISSN 0932-0113. PMID 9694368. doi:10.1007/s004360050444.
- ↑ James A. Phills; A. John Harrold; Gabriel V. Whiteman; Lewis Perelmutter (1972). "Pulmonary infiltrates, asthma and eosinophilia due to Ascaris suum infestation in man" (PDF). New England Journal of Medicine. 286: 965–970. PMID 5062734. doi:10.1056/NEJM197205042861802.
- ↑ "Risk Assessment for Food Terrorism and Other Food Safety Concerns". Food and Drug Administration Center for Food Safety and Applied Nutrition. October 13, 2003. Archived from the original on May 27, 2009. Retrieved February 15, 2012.
- ↑ Aaron R. Jex; Shiping Liu; Bo Li; Neil D. Young; Ross S. Hall; et al. (2011). "Ascaris suum draft genome" (PDF). Nature. 479 (7374): 529–533. PMID 22031327. doi:10.1038/nature10553.