Intrauterine hypoxia
| Intrauterine hypoxia | |
|---|---|
 | |
| Micrograph of a placental infarct (left of image), a cause of intrauterine hypoxia. H&E stain. | |
| Classification and external resources | |
| Specialty | pediatrics |
| ICD-10 | P20 |
| ICD-9-CM | 768 |
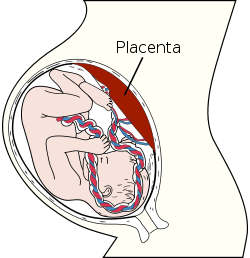
Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction and maternal smoking. Intrauterine growth restriction (IUGR) may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system (the brain and spinal cord). This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, ADHD, eating disorders and cerebral palsy.[1][2][3][4][5][6]
Cause
There are various causes for intrauterine hypoxia (IH). The most preventable cause is maternal smoking. Cigarette smoking by expectant mothers has been shown to have a wide variety of deleterious effects on the developing fetus. Among the negative effects are carbon monoxide induced tissue hypoxia and placental insufficiency which causes a reduction in blood flow from the uterus to the placenta thereby reducing the availability of oxygenated blood to the fetus. Placental insufficiency as a result of smoking has been shown to have a causal effect in the development of pre-eclampsia. While some previous studies have suggested that carbon monoxide from cigarette smoke may have a protective effect against preeclampsia, a recent study conducted by the Genetics of Pre-Eclampsia Consortium (GOPEC) in the United Kingdom found that smokers were five times more likely to develop pre-eclampsia.[7] Nicotine alone has been shown to be a teratogen which affects the autonomic nervous system, leading to increased susceptibility to hypoxia-induced brain damage.[7][8][9][10][11][12] Maternal anemia in which smoking has also been implicated is another factor associated with IH/BA. Smoking by expectant mothers causes a decrease in maternal nucleated red blood cells (NRBC), thereby reducing the amount of red blood cells available for oxygen transport.[13][14][15]
The perinatal brain injury occurring as a result of birth asphyxia, manifesting within 48 hours of birth, is a form of hypoxic ischemic encephalopathy.
Treatment
Treatment of infants suffering birth asphyxia by lowering the core body temperature is now known to be an effective therapy to reduce mortality and improve neurological outcome in survivors, and hypothermia therapy for neonatal encephalopathy begun within 6 hours of birth significantly increases the chance of normal survival in affected infants.
There has long been a debate over whether newborn infants with birth asphyxia should be resuscitated with 100% oxygen or normal air.[16] It has been demonstrated that high concentrations of oxygen lead to generation of oxygen free radicals, which have a role in reperfusion injury after asphyxia.[17] Research by Ola Didrik Saugstad and others led to new international guidelines on newborn resuscitation in 2010, recommending the use of normal air instead of 100% oxygen.[18][19]
Epidemiology
In the United States, intrauterine hypoxia and birth asphyxia were listed together as the tenth leading cause of neonatal death.[20]
Financial Costs
IH/BA is also a causitive factor in cardiac and circulatory birth defects the sixth most expensive condition, as well as premature birth and low birth weight the second most expensive and it is one of the contributing factors to infant respiratory distress syndrome (RDS) also known as hyaline membrane disease, the most expensive medical condition to treat and the number one cause of infant mortality.[21][22][23]
| Most expensive medical condition treated in U.S. hospitals. 4 out of 10 linked to intrauterine hypoxia/birth asphxia | Cost | Hospital Charge |
| 1. Infant respiratory distress syndrome | $45,542 | $138,224 |
| 2. Premature birth and low birth weight | $44,490 | $119,389 |
| 6. Cardiac and circulatory birth defects | $35,960 | $101,412 |
| 9. Intrauterine hypoxia or birth asphyxia | $27,962 | $74,942 |
Medicolegal
In the United States the National Practitioner Data Bank 2006 Annual Report obstetrics-related cases accounted for 8.7 percent of all 2006 physician Malpractice Payment Reports and had the highest median payment amounts ($333,334).[24]
References
- ↑ Maslova, MV; Maklakova, AS; Sokolova, NA; Ashmarin, IP; Goncharenko, EN; Krushinskaya, YV (2003). "The effects of ante- and postnatal hypoxia on the central nervous system and their correction with peptide hormones". Neuroscience and Behavioral Physiology. 33 (6): 607–11. PMID 14552554. doi:10.1023/A:1023938905744.
- ↑ Habek, D; Habek, JC; Jugović, D; Salihagić, A (2002). "Intrauterine hypoxia and sudden infant death syndrome". Acta medica Croatica : casopis Hravatske akademije medicinskih znanosti. 56 (3): 109–18. PMID 12630342.
- ↑ Bulterys, MG; Greenland, S; Kraus, JF (1990). "Chronic fetal hypoxia and sudden infant death syndrome: interaction between maternal smoking and low hematocrit during pregnancy". Pediatrics. 86 (4): 535–40. PMID 2216618.
- ↑ Peleg, D; Kennedy, CM; Hunter, SK (1998). "Intrauterine growth restriction: identification and management". American family physician. 58 (2): 453–60, 466–7. PMID 9713399.
- ↑ Rosenberg, A (2008). "The IUGR newborn". Seminars in perinatology. 32 (3): 219–24. PMID 18482625. doi:10.1053/j.semperi.2007.11.003.
- ↑ Gonzalez, FF; Miller, SP (2006). "Does perinatal asphyxia impair cognitive function without cerebral palsy?". Archives of Disease in Childhood: Fetal and Neonatal Edition. 91 (6): F454–9. PMC 2672766
 . PMID 17056843. doi:10.1136/adc.2005.092445.
. PMID 17056843. doi:10.1136/adc.2005.092445. - 1 2 Pipkin FB, Genetics of Preeclampsia, Consortium (2008). "Smoking in moderate/severe preeclampsia worsens pregnancy outcome, but smoking cessation limits the damage". Hypertension. 51 (4): 1042–6. PMID 18259022. doi:10.1161/HYPERTENSIONAHA.107.106559.
- ↑ Slotkin, TA (1998). "Fetal nicotine or cocaine exposure: which one is worse?". The Journal of Pharmacology and Experimental Therapeutics. 285 (3): 931–45. PMID 9618392.
- ↑ Bouhours-Nouet, N; May-Panloup, P; Coutant, R; De Casson, FB; Descamps, P; Douay, O; Reynier, P; Ritz, P; Malthièry, Y; Simard, G (2005). "Maternal smoking is associated with mitochondrial DNA depletion and respiratory chain complex III deficiency in placenta". American Journal of Physiology. Endocrinology and Metabolism. 288 (1): E171–7. PMID 15585597. doi:10.1152/ajpendo.00260.2003.
- ↑ Gogiia, TE (2005). "Risk of iugr syndrome development during preeclampsia of the pregnant". Georgian medical news (128): 15–7. PMID 16369054.
- ↑ Salafia, CM; Minior, VK; Pezzullo, JC; Popek, EJ; Rosenkrantz, TS; Vintzileos, AM (1995). "Intrauterine growth restriction in infants of less than thirty-two weeks' gestation: associated placental pathologic features". American Journal of Obstetrics and Gynecology. 173 (4): 1049–57. PMID 7485292. doi:10.1016/0002-9378(95)91325-4.
- ↑ Kingdom, JC; Kaufmann, P (1997). "Oxygen and placental villous development: origins of fetal hypoxia". Placenta. 18 (8): 613–21; discussion 623–6. PMID 9364596. doi:10.1016/S0143-4004(97)90000-X.
- ↑ Chełchowska, M; Laskowska-Klita, T (2002). "Effect of maternal smoking on some markers of iron status in umbilical cord blood". Roczniki Akademii Medycznej w Bialymstoku (1995). 47: 235–40. PMID 12533965.
- ↑ Habek, D; Habek, JC; Ivanisević, M; Djelmis, J (2002). "Fetal tobacco syndrome and perinatal outcome". Fetal diagnosis and therapy. 17 (6): 367–71. PMID 12393968. doi:10.1159/000065387.
- ↑ Pathology of the human placenta By Kurt Benirschke, Peter Kaufmann. page 453. Publisher: Springer; 4th edition (March 23, 2000) Language: English ISBN 0-387-98894-7 ISBN 978-0387988948
- ↑ Davis, PG; Tan, A; O'Donnell, CPF; Schulze, A (2004). "Resuscitation of newborn infants with 100% oxygen or air: a systematic review and meta-analysis". The Lancet. 364: 1329–1333. PMID 15474135. doi:10.1016/S0140-6736(04)17189-4.
- ↑ Kutzsche, S; Ilves, P; Kirkeby, OJ; Saugstad, OD (2001). "Hydrogen peroxide production in leukocytes during cerebral hypoxia and reoxygenation with 100% or 21% oxygen in newborn piglets". Pediatric Research. 49: 834–842. PMID 11385146. doi:10.1203/00006450-200106000-00020.
- ↑ ILCOR Neonatal Resuscitation Guidelines 2010
- ↑ Norwegian paediatrician honoured by University of Athens, Norway.gr
- ↑ National Center for Health Statistics
- ↑ Rueda-Clausen, CF; Morton, JS; Davidge, ST (2009). "Effects of hypoxia-induced intrauterine growth restriction on cardiopulmonary structure and function during adulthood". Cardiovascular research. 81 (4): 713–22. PMID 19088083. doi:10.1093/cvr/cvn341.
- ↑ Sly, PD; Drew, JH (1981). "Massive pulmonary haemorrhage: a cause of sudden unexpected deaths in severely growth retarded infants". Australian paediatric journal. 17 (1): 32–4. PMID 7247876. doi:10.1111/j.1440-1754.1981.tb00010.x.
- ↑ Hyaline Membrane Disease eMedicine
- ↑ National Practitioner Data Bank 2006 Annual Report
External links
- Hypoxic-Ischemic Brain Injury in the Newborn
- Hypoxic-Ischemic Encephalopathy
- Smoking and Pre-eclampsia
- Clear Criteria for Defining Birth Asphyxia