Interleukin-1 family
| Interleukin-1 / 18 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 | |||||||||
| Identifiers | |||||||||
| Symbol | IL1 | ||||||||
| Pfam | PF00340 | ||||||||
| InterPro | IPR000975 | ||||||||
| PROSITE | PDOC00226 | ||||||||
| SCOP | 1i1b | ||||||||
| SUPERFAMILY | 1i1b | ||||||||
| |||||||||
The Interleukin-1 family (IL-1 family) is a group of 11 cytokines, which plays a central role in the regulation of immune and inflammatory responses to infections or sterile insults.
Discovery
Discovery of these cytokines began with studies on the pathogenesis of fever. The studies were performed by Menkin and Beeson in 1943-1948 on the fever-producing properties of proteins released from rabbit peritoneal exudate cells. These studies were followed by contributions of several investigators, who were primarily interested in the link between fever and infection/inflammation. The basis for the term "interleukin" was to streamline the growing number of biological properties attributed to soluble factors from macrophages and lymphocytes. IL-1 was the name given to the macrophage product, whereas IL-2 was used to define the lymphocyte product. At the time of the assignment of these names, there was no amino acid sequence analysis known and the terms were used to define biological properties.
In 1985 two distinct, but distantly related complementary DNAs encoding proteins sharing human IL-1 activity were reported to be isolated from a macrophage cDNA library, thus defining two individual members of the IL-1 family – IL-1α and IL-1β.[1][2][3]
The Interleukin-1 superfamily
IL-1 family is a group of 11 cytokines, which induces a complex network of proinflammatory cytokines and via expression of integrins on leukocytes and endothelial cells, regulates and initiates inflammatory responses.[4]
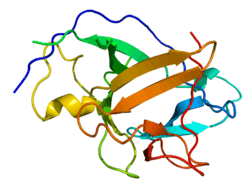
IL-1α and IL-1β are the most studied members, because they were discovered first and because they possess strongly proinflammatory effect. They have a natural antagonist IL-1Ra (IL-1 receptor antagonist). All three of them include a beta trefoil fold and bind IL-1 receptor (IL-1R) and activate signaling via MyD88 adaptor, which is described in the Signaling section of this page. IL-1Ra regulates IL-1α and IL-1β proinflammatory activity by competing with them for binding sites of the receptor.[4][5][6]
Synthesis
All of the members of IL-1 family, except IL-1Ra, are first synthesized as a precursor protein, which means it is synthesized as a long form of a protein which has to be proteolytically cleaved to a shorter, active molecule, which is generally called a mature protein. IL-1 family precursors do not have a clear signal peptide for processing and secretion and none of them are found in the Golgi; they belong to so-called leaderless secretory protein group. The similar feature of IL-1α and IL-33 is that their precursor forms can bind to their respective receptor and can activate signal transduction. But this is not a common feature for all IL-1 family members, since IL-1β and IL-18 precursor forms do not bind their receptors and require proteolytic cleavage by either intracellular caspase-1 or extracellular neutrophilic proteases.[4]
Nomenclature
The interleukin-1 superfamily has 11 members, which have similar gene structure, although originally it contained only four members IL-1α, IL-1β, IL-1Ra and IL-18. After discovery of another 5 members the updated nomenclature was generally accepted which included all members of IL-1 cytokine family. The old IL-1 members were renamed to IL-1F1, IL-1F2, IL-1F3 and IL-1F4.[7]
But according to new trends in nomenclature, the old names of IL-1 family returned. In 2010, laboratories all around the world agreed that IL-1α, IL-1β, IL-1Ra and IL-18 are more familiar to the general scientific knowledge. According to that, they suggested that IL-1F6, IL-1F8 and IL-1F9 should get new names IL-36α, IL-36β and IL-36γ, even though they are encoded by distinct genes, they use the same receptor complex IL-1Rrp2 and coreceptor IL-1RAcP and deliver almost identical signals. The nomenclature also proposes that IL-1F5 should be renamed to IL-36Ra, because it works as an antagonist to IL-36α, IL-36β and IL-36γ similar to how IL-1Ra works for IL-1α and IL-1β. Another revision was the renaming of IL-1F7 to IL-37 because this suppressing cytokine has many splicing variants, they should be called IL-37a, IL-37b and so on. For IL-1F10 there is a reserved name, IL-38.[8]
| Name | Family name | Receptor | Coreceptor | Property | Chromosomal location |
|---|---|---|---|---|---|
| IL-1α | IL-1F1 | IL-1RI | IL-1RAcP | Proinflammatory | 2q14 |
| IL-1β | IL-1F2 | IL-1RI | IL-1RAcP | Proinflammatory | 2q14 |
| IL-1Ra | IL-1F3 | IL-1RI | NA | Antagonist for IL-1α, IL-1β | 2q14.2 |
| IL-18 | IL-1F4 | IL-18Rα | IL-18Rβ | Proinflammatory | 11q22.2-q22.3 |
| IL-36Ra | IL-1F5 | IL-1Rrp2 | NA | Antagonist for IL-36α, IL-36β, IL-36γ | 2q14 |
| IL-36α | IL-1F6 | IL-1Rrp2 | IL-1RAcP | Proinflammatory | 2q12 - q14.1 |
| IL-37 | IL-1F7 | Unknown | Unknown | Anti-inflammatory | 2q12 – q14.1 |
| IL-36β | IL-1F8 | IL-1Rrp2 | IL-1RAcP | Proinflammatory | 2q14 |
| IL-36γ | IL1-F9 | IL-1Rrp2 | IL-1RAcP | Proinflammatory | 2q12 – q21 |
| IL-38 | IL-1F10 | IL-1Rrp2 | Unknown | Anti-inflammatory | 2q13 |
| IL-33 | IL-1F11 | ST2 | IL-1RAcP | Th2 responses, proinflammatory | 9p24.1 |
Signaling
IL-1α and IL-1β bind to the same receptor molecule, which is called type I IL-1 receptor (IL-1RI). There is a third ligand of this receptor – the Interleukin 1 receptor antagonist (IL-1Ra), which does not activate downstream signaling, so it acts as an inhibitor of IL-1α and IL-1β signaling by competing with them for binding sites of the receptor.[4][11]
IL-1α or IL-1β bind first to the first extracellular chain of IL-1RI, that recruits the IL-1 receptor accessory protein (IL-1RAcP), which serves as a coreceptor and is necessary for signal transduction and it is also needed for activation of IL-1RI by IL-18 and IL-33.[11]
After the formation of receptor heterodimeric complex which is assembled by IL-1α or IL-1β, IL-1RI and IL-1RAcP, two intracellular adaptor proteins are assembled by conserved cytosolic regions called Toll- and IL-1R-like (TIR) domains. They are called the myeloid differentiation primary response gene 88 (MYD88) and interleukin-1 receptor-activated protein kinase (IRAK) 4. Phosphorylation of IRAK4 is followed by phosphorylation of IRAK1, IRAK2 and tumor necrosis factor receptor-associated factor (TRAF) 6. TRAF6 is a ubiquitin E3 ligase, that in association with ubiquitin-conjugating enzyme (ubiquitin E2 ligase) complex attaches K63-linked polyubiquitin chains to some of IL-1signaling intermediates, for instance TGF-β-activated protein kinase (TAK-1). That facilitates the association of TAK-1 with TRAF6 and with MEKK3.[11] These signaling pathways lead to activation of many transcription factors, such as NF-κB, AP-1, c-Jun N-terminal kinase (JNK) and p38 MAPK.[11][12]
IL-1α precursor and mature IL-1β lack a signal peptide which should direct them into the endoplasmic/Golgi-dependent secretion pathway and they are secreted by an unconventional protein secretion pathway, of which the mechanism and regulation are not known.[13]
Biological activity
IL-1 is intensely produced by tissue macrophages, monocytes, fibroblasts, and dendritic cells, but is also expressed by B lymphocytes, NK cells, microglia, and epithelial cells. They form an important part of the inflammatory response of the body against infection. These cytokines increase the expression of adhesion factors on endothelial cells to enable transmigration (also called diapedesis) of immunocompetent cells, such as phagocytes, lymphocytes and others, to sites of infection. They also affect the activity of the hypothalamus, the thermoregulatory center, which leads to a rise in body temperature (fever) . That is why IL-1 is called an endogenous pyrogen. Besides fever, IL-1 also causes hyperalgesia (increased pain sensitivity), vasodilation and hypotension. [9] [13]
IL-1α
IL-1α is a “dual-function cytokine”, which means it plays a role in the nucleus by affecting transcription, apart from its extracellular receptor-mediated effects as a classical cytokine. In this group also belongs IL-33.[14]
IL-1α is synthesized as a precursor protein and it is constitutively stored in the cytoplasm of cells with mesenchymal origin and in epithelial cells. On the contrary, monocytes and macrophages do not contain preformed IL-1α precursors, but instead require de novo synthesis. IL-1α precursor is processed to a mature 17-kDa protein by a Ca2+-activated protease, calpain, by liberating the 16-kDa N-terminal propiece cleavage product (ppIL-1α), which contains a nuclear localization sequence (NLS), translocates to the nucleus and functions as a transcription factor. The precursor form of IL-1α, which has both the N-terminal and C-terminal receptor interacting domains, acts as a damage-associated molecular pattern (DAMP) molecule. DAMPs, also known as alarmins, are recognized by innate immunity cells by pattern recognition receptors (PRRs) and functions as danger signals for the immune system. In short, DAMPs are released from stressed cells, which undergo necrosis or pyroptosis and their intracellular components are released into extracellular space. Because of misfolding and other oxidative changes of these molecules in the context of altered pH, they are recognized by innate immunity as molecules that should not be in extracellular space. The reasons why the cell could be stressed are infection, injury, ischemia, hypoxia, acidosis and complement lysis. The IL-33 precursor molecule acts in a similar way as a DAMP molecule.[14]
Interestingly, the inflammatory responses in the absence of infection (such as ischemia) are only dependent on IL-1α signaling via the Interleukin-1 receptor (IL-1R), rather than TLRs signaling. IL-1α also stimulates transcription and secretion of IL-1β from monocytes, so the initiator of immune responses is likely IL-1α precursor by induction of neutrophil infiltration. IL-1β seems to be an amplifier of inflammation by recruiting of macrophages in the context of sterile inflammation.[14][15][16]
IL-1β
IL-1β is synthesized as a precursor form protein only after stimulation, in contrast to IL-1α. Its expression is induced by transcription factor NF-κB after exposure of innate immune cells to alarmins. This occurs, for instance, after exposure of macrophages and dendritic cells to lipopolysaccharide (LPS), which binds to TLR4 and acts as pathogen-associated molecular pattern, which is another group of alarmins.[13][16]
The synthesis of IL-1β precursor (and IL-18) is induced by stimulation of innate immune cells by Toll-like receptors (TLRs) or RIG-like receptors (RLRs), but to gain the ability to bind to IL-1 receptor, the IL-1β precursor has to be cleaved by a cysteine protease called caspase-1. Caspase-1 needs to be activated by a formation called the inflammasome which is mediated by cytoplasmic pattern recognition receptor signaling. So, the secretion of IL-1β needs these two steps and activation of different receptors to be activated. Under special circumstances IL-1β can be processed also by other proteases, like during high neutrophilic inflammation.[13][17]
IL-18 is also synthesized as a precursor which is cleaved by caspase-1.[13]
IL-33
IL-33 is synthesized as a 31-kDa precursor form and binds the ST2 receptor and IL-1RAcP coreceptor, which stimulates signaling that activates transcription factors as NF-κB and ERK, p38 and JNK MAPKs. The signaling can be triggered by a precursor form of IL-33 in the same way as IL-1α precursor activates signaling through the IL-1 receptor. On the other hand, the mature forms IL-3395-270, IL-3399-270 and IL-33109-270, which are processed from a precursor by serine proteases cathepsin G and elastase, are even more potent activators of inflammatory responses. In contrast with IL-1, processing by caspases, like caspase-1, results in IL-33 inactivation.[18] [19] [20]
IL-33 is a dual function cytokine. Besides its chromatin-associated function, it is constitutively expressed in healthy endothelial cells, because it acts as DAMPs after its release to extracellular space of cells in the context of immunologic not-silent cell death (necrosis or pyroptosis), and drives cytokine production in natural helper cells, nuocytes, Th2 lymphocytes, mast cells, basophils, eosinophils, invariant natural killer and natural killer T cells. It is involved in allergic and parasite-induced inflammatory responses.[18][19]
Cytokine-induced effector cytokine production
IL-33 has a role in so called cytokine-induced effector cytokine production, which means that a production of effector cytokines by differentiated T helper lymphocytes is cytokine dependent and can happen without antigen stimulation by T-cell receptor of these cells. IL-33 in combination with some STAT5 activators, such as IL-2, IL-7 or TSLP, up-regulates expression of its own receptor on already differentiated Th2 lymphocytes, because naive T helper cells nor Th1 nor Th17 populations do not have ST2 receptors. This up-regulation works as a positive feedback which causes even more strong activation of IL-33 dependent-signaling pathways in the lymphocyte. This up-regulation is directly controlled by GATA3 transcription factor. IL-33 combined with IL-2, IL-7 or TSLP also stimulates cell proliferation. The effector cytokine which is secreted from IL-33- and STAT5 activator-stimulated Th2 cells is IL-13, which is NF-κB dependent. IL-13 is very similar to IL-4 in amino acid sequence and structure. They also used the same type II IL-4 receptor to activate STAT6.[20]
Similar functions have IL-1 to Th17 cells and IL-18 to Th1 lymphocytes. IL-1 combined with some STAT3 activators, such as IL-6, IL-21 or IL-23, which are important for Th17 lymphocytes differentiation, have similar positive feedback in Th17 cells just like IL-33 and STAT5 activators have in Th2 cells. They highly up-regulate expression of IL-1 receptor and RORγt on the surface of stimulated Th17 lymphocytes. The effector cytokines mediated by this signalization are IL-17A, IL-4 and IL-6. IL-18 with IL-12, which is a STAT4 activator, have similar effects on Th1 cells by up-regulating expression of IL-18R1 receptor and T-bet.[20][21]
IL-1 in disease and its clinical significance
IL-1 has a major role in neuroinflammation.[22] During inflammation, there are increased levels of TNF and IL-1 in the brain,[23] and their presence may cause the breakdown of the blood-brain barrier.[23] Polymorphisms in IL-1 genes have been found to contribute to genetic susceptibility to some cancers,[24] ankylosing spondylitis[25] and Grave's disease.[26]
In terms of clinical use, because of its characterization as a hematopoetic factor, IL-1 was given to patients after bone marrow transplantation to improve the engraftment. But soon it was discovered that the patients were experiencing symptoms of systemic inflammation. Pharmacological blockade of these receptors was then sought in order to relieve symptoms. The endogenous IL-1 receptor antagonist (IL-1Ra), also known as anakinra, was tried in clinical trials to lessen systemic inflammation, but did not demonstrate a statistically significant difference from placebo.[4]
Nowadays, the blockade of IL-1 activity (especially IL-1β) is a standard therapy for patients with autoimmune diseases or lymphomas. Anakinra (IL-1Ra) is FDA-approved as a therapy for patients with rheumatoid arthritis,[27] because it reduces symptoms and slows joint destruction of this inflammatory disease. It has also been prescribed to patients with indolent or smoldering myeloma with a high risk of progression to multiple myeloma. In combination with other medication, IL-1Ra provides a significant increase in the number of years of progression-free disease in its recipients. The benefits of this treatment are the natural structure and no toxicity or gastrointestinal disturbances.[4]
References
- ↑ March CJ, Mosley B, Larsen A, Cerretti DP, Braedt G, Price V, Gillis S, Henney CS, Kronheim SR, Grabstein K (Aug 1985). "Cloning, sequence and expression of two distinct human interleukin-1 complementary DNAs". Nature. 315 (6021): 641–7. PMID 2989698. doi:10.1038/315641a0.
- ↑ Auron PE, Webb AC, Rosenwasser LJ, Mucci SF, Rich A, Wolff SM, Dinarello CA (1984). "Nucleotide sequence of human monocyte interleukin 1 precursor cDNA". Proc. Natl. Acad. Sci. U.S.A. 81 (24): 7907–11. PMC 392262
 . PMID 6083565. doi:10.1073/pnas.81.24.7907.
. PMID 6083565. doi:10.1073/pnas.81.24.7907. - ↑ Dinarello CA (1994). "The interleukin-1 family: 10 years of discovery". FASEB J. 8 (15): 1314–25. PMID 8001745.
- 1 2 3 4 5 6 7 Dinarello CA (2011). "Interleukin-1 in the pathogenesis and treatment of inflammatory diseases". Blood. 117 (14): 3720–32. PMC 3083294
 . PMID 21304099. doi:10.1182/blood-2010-07-273417.
. PMID 21304099. doi:10.1182/blood-2010-07-273417. - ↑ Murzin AG, Lesk AM, Chothia C (Jan 1992). "β-trefoil fold: patterns of structure and sequence in the kunitz inhibitors interleukins-1β and 1α and fibroblast growth factors". Journal of Molecular Biology. 223 (2): 531–43. PMID 1738162. doi:10.1016/0022-2836(92)90668-A.
- ↑ Gosavi S, Whitford PC, Jennings PA, Onuchic JN (Jul 2008). "Extracting function from a β-trefoil folding motif". PNAS. 105 (30): 10384–9. PMC 2492465
 . PMID 18650393. doi:10.1073/pnas.0801343105.
. PMID 18650393. doi:10.1073/pnas.0801343105. - ↑ Sims JE, Nicklin MJ, Bazan JF, Barton JL, Busfield SJ, Ford JE, Kastelein RA, Kumar S, Lin H, Mulero JJ, Pan J, Pan Y, Smith DE, Young PR (2001). "A new nomenclature for IL-1-family genes". Trends Immunol. 22 (10): 536–7. PMID 11574262. doi:10.1016/S1471-4906(01)02040-3.
- ↑ Dinarello C, Arend W, Sims J, Smith D, Blumberg H, O'Neill L, Goldbach-Mansky R, Pizarro T, Hoffman H, Bufler P, Nold M, Ghezzi P, Mantovani A, Garlanda C, Boraschi D, Rubartelli A, Netea M, van der Meer J, Joosten L, Mandrup-Poulsen T, Donath M, Lewis E, Pfeilschifter J, Martin M, Kracht M, Muehl H, Novick D, Lukic M, Conti B, Solinger A, Kelk P, Peyman K, van de Veerdonk F, Gabel C (2010). "IL-1 family nomenclature". Nat. Immunol. 11 (11): 973. PMID 20959797. doi:10.1038/ni1110-973.
- ↑ http://www.pnas.org/content/109/8/3001.short
- ↑ http://www.genenames.org/genefamilies/IL
- 1 2 3 4 Weber A, Wasiliew P, Kracht M (2010). "Interleukin-1 (IL-1) pathway". Sci Signal. 3 (105): cm1. PMID 20086235. doi:10.1126/scisignal.3105cm1.
- ↑ 1. Simi A, Tsakiri N, Wang P, Rothwell NJ. Interleukin-1 and inflammatory neurodegeneration. Biochemical Society Transactions. 2007 Oct 1;35(5):1122–6.
- 1 2 3 4 5 Contassot E, Beer HD, French LE (2012). "Interleukin-1, inflammasomes, autoinflammation and the skin". Swiss Med Wkly. 142: w13590. PMID 22653747. doi:10.4414/smw.2012.13590.
- 1 2 3 Cohen I, Rider P, Carmi Y, Braiman A, Dotan S, White MR, Voronov E, Martin MU, Dinarello CA, Apte RN (2010). "Differential release of chromatin-bound IL-1alpha discriminates between necrotic and apoptotic cell death by the ability to induce sterile inflammation". Proc. Natl. Acad. Sci. U.S.A. 107 (6): 2574–9. PMC 2823886
 . PMID 20133797. doi:10.1073/pnas.0915018107.
. PMID 20133797. doi:10.1073/pnas.0915018107. - ↑ Rider P, Carmi Y, Guttman O, Braiman A, Cohen I, Voronov E, White MR, Dinarello CA, Apte RN (2011). "IL-1α and IL-1β recruit different myeloid cells and promote different stages of sterile inflammation". J. Immunol. 187 (9): 4835–43. PMID 21930960. doi:10.4049/jimmunol.1102048.
- 1 2 Matzinger P (2012). "The evolution of the danger theory. Interview by Lauren Constable, Commissioning Editor". Expert Rev Clin Immunol. 8 (4): 311–7. PMID 22607177. doi:10.1586/eci.12.21.
- ↑ Sahoo M, Ceballos-Olvera I, del Barrio L, Re F (2011). "Role of the inflammasome, IL-1β, and IL-18 in bacterial infections". ScientificWorldJournal. 11: 2037–50. PMC 3217589
 . PMID 22125454. doi:10.1100/2011/212680.
. PMID 22125454. doi:10.1100/2011/212680. - 1 2 Lefrançais E, Roga S, Gautier V, Gonzalez-de-Peredo A, Monsarrat B, Girard JP, Cayrol C (2012). "IL-33 is processed into mature bioactive forms by neutrophil elastase and cathepsin G". Proc. Natl. Acad. Sci. U.S.A. 109 (5): 1673–8. PMC 3277172
 . PMID 22307629. doi:10.1073/pnas.1115884109.
. PMID 22307629. doi:10.1073/pnas.1115884109. - 1 2 Cayrol C, Girard JP (2009). "The IL-1-like cytokine IL-33 is inactivated after maturation by caspase-1". Proc. Natl. Acad. Sci. U.S.A. 106 (22): 9021–6. PMC 2690027
 . PMID 19439663. doi:10.1073/pnas.0812690106.
. PMID 19439663. doi:10.1073/pnas.0812690106. - 1 2 3 Guo L, Wei G, Zhu J, Liao W, Leonard WJ, Zhao K, Paul W (2009). "IL-1 family members and STAT activators induce cytokine production by Th2, Th17, and Th1 cells". Proc. Natl. Acad. Sci. U.S.A. 106 (32): 13463–8. PMC 2726336
 . PMID 19666510. doi:10.1073/pnas.0906988106.
. PMID 19666510. doi:10.1073/pnas.0906988106. - ↑ Ben-Sasson SZ, Hu-Li J, Quiel J, Cauchetaux S, Ratner M, Shapira I, Dinarello CA, Paul WE (2009). "IL-1 acts directly on CD4 T cells to enhance their antigen-driven expansion and differentiation". Proc. Natl. Acad. Sci. U.S.A. 106 (17): 7119–24. PMC 2678417
 . PMID 19359475. doi:10.1073/pnas.0902745106.
. PMID 19359475. doi:10.1073/pnas.0902745106. - ↑ Moynagh PN (2005). "The interleukin-1 signalling pathway in astrocytes: a key contributor to inflammation in the brain". J. Anat. 207 (3): 265–9. PMC 1571539
 . PMID 16185251. doi:10.1111/j.1469-7580.2005.00445.x.
. PMID 16185251. doi:10.1111/j.1469-7580.2005.00445.x. - 1 2 Hofman FM, von Hanwehr RI, Dinarello CA, Mizel SB, Hinton D, Merrill JE (1986). "Immunoregulatory molecules and IL 2 receptors identified in multiple sclerosis brain". J. Immunol. 136 (9): 3239–45. PMID 3082983.
- ↑ Durães C, Muñoz X, Bonet C, García N, Venceslá A, Carneiro F, Peleteiro B, Lunet N, Barros H, Lindkvist B, Boutron-Ruault MC, Bueno-de-Mesquita HB, Rizzato C, Trichopoulou A, Weiderpass E, Naccarati A, Travis RC, Tjønneland A, Gurrea AB, Johansson M, Riboli E, Figueiredo C, González CA, Capellà G, Machado JC, Sala N (2014). "Genetic variants in the IL1A gene region contribute to intestinal-type gastric carcinoma susceptibility in European populations". Int. J. Cancer. 135 (6): 1343–1355. PMID 24615437. doi:10.1002/ijc.28776.
- ↑ Timms AE, Crane AM, Sims AM, Cordell HJ, Bradbury LA, Abbott A, Coyne MR, Beynon O, Herzberg I, Duff GW, Calin A, Cardon LR, Wordsworth BP, Brown MA (2004). "The interleukin 1 gene cluster contains a major susceptibility locus for ankylosing spondylitis". Am. J. Hum. Genet. 75 (4): 587–598. PMC 1182046
 . PMID 15309690. doi:10.1086/424695.
. PMID 15309690. doi:10.1086/424695. - ↑ Liu N, Li X, Liu C, Zhao Y, Cui B, Ning G (2010). "The association of interleukin-1alpha and interleukin-1beta polymorphisms with the risk of Graves' disease in a case-control study and meta-analysis". Hum. Immunol. 71 (4): 397–401. PMID 20116409. doi:10.1016/j.humimm.2010.01.023.
- ↑ "Anakinra". DrugBank Version 4.1. Retrieved Jan 29, 2014.