Pyloric stenosis
| Pyloric stenosis | |
|---|---|
| Synonyms | Pylorostenosis, infantile hypertrophic pyloric stenosis |
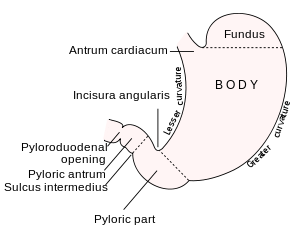 | |
| Outline of stomach, showing its anatomical landmarks, including the pylorus. | |
| Specialty | General surgery |
| Symptoms | Projectile vomiting after feeding[1] |
| Complications | Dehydration, electrolyte problems[1] |
| Usual onset | 2 to 12 weeks old[1] |
| Causes | Unknown[2] |
| Risk factors | Cesarean section, preterm birth, bottle feeding, first born[3] |
| Diagnostic method | physical examination,[1] ultrasound[4] |
| Similar conditions | Gastroesophageal reflux,[1] intussusception[5] |
| Treatment | Surgery[1] |
| Prognosis | Excellent[1] |
| Frequency | 1.5 per 1,000 babies[1] |
Pyloric stenosis is a narrowing of the opening from the stomach to the first part of the small intestine (the pylorus). Symptoms include projectile vomiting without the presence of bile. This most often occurs after the baby is fed. The typically age that symptoms become obvious is two to twelve weeks old.[1]
The cause of pyloric stenosis is unclear.[2] Risk factors in babies include birth by cesarean section, preterm birth, bottle feeding, and being first born.[3] The diagnosis may be made by feeling an olive-shaped mass in the babies abdomen.[1] This is often confirmed with ultrasound.[4]
Treatment initially begins by correcting dehydration and electrolyte problems. This is then typically followed by surgery. Results are generally good both in the short term and in the long term. Some treat the condition without surgery by using atropine.[1]
About one to two per thousand babies are affected. Males are affected about four times more often than females.[1] The condition is very rare in adults.[6] The first description of pyloric stenosis was in 1888 with surgery management first carried out 1912 by Conrad Ramstedt.[1][2] Before surgical treatment most babies died.[1]
Signs and symptoms
Babies with this condition usually present any time in the first weeks to months of life with progressively worsening vomiting. The vomiting is often described as non-bile stained ("non bilious") and "projectile vomiting", because it is more forceful than the usual spittiness (gastroesophageal reflux) seen at this age. Some infants present with poor feeding and weight loss but others demonstrate normal weight gain. Dehydration may occur which causes a baby to cry without having tears and to produce less wet or dirty diapers due to not urinating for hours or for a few days. Symptoms usually begin between 3 to 12 weeks of age. Findings include epigastric fullness with visible peristalsis in the upper abdomen from the person's left to right.[7] Constant hunger, belching, and colic are other possible signs that the baby is unable to eat properly.
Cause
Pyloric stenosis seems to be multifactorial, with some genetic and some environmental components. It is four times more likely to occur in males,[8] and is also more common in the first born.[9] Rarely, infantile pyloric stenosis can occur as an autosomal dominant condition.[10]
It is uncertain whether it is a congenital anatomic narrowing or a functional hypertrophy of the pyloric sphincter muscle.
Pathophysiology
The gastric outlet obstruction due to the hypertrophic pylorus impairs emptying of gastric contents into the duodenum. As a consequence, all ingested food and gastric secretions can only exit via vomiting, which can be of a projectile nature. While the exact cause of the hypertrophy remains unknown, one study suggested that neonatal hyperacidity may be involved in the pathogenesis.[11] This physiological explanation for the development of clinical pyloric stenosis at around 4 weeks and its spontaneous long term cure without surgery if treated conservatively, has recently been further reviewed.[12]
Persistent vomiting results in loss of stomach acid (hydrochloric acid). The vomited material does not contain bile because the pyloric obstruction prevents entry of duodenal contents (containing bile) into the stomach. The chloride loss results in a low blood chloride level which impairs the kidney's ability to excrete bicarbonate. This is the significant factor that prevents correction of the alkalosis.[13]
A secondary hyperaldosteronism develops due to the decreased blood volume. The high aldosterone levels causes the kidneys to avidly retain Na+ (to correct the intravascular volume depletion), and excrete increased amounts of K+ into the urine (resulting in a low blood level of potassium).
The body's compensatory response to the metabolic alkalosis is hypoventilation resulting in an elevated arterial pCO2.
Diagnosis

Diagnosis is via a careful history and physical examination, often supplemented by radiographic imaging studies. Pyloric stenosis should be suspected in any young infant with severe vomiting. On physical exam, palpation of the abdomen may reveal a mass in the epigastrium. This mass, which consists of the enlarged pylorus, is referred to as the 'olive',[15] and is sometimes evident after the infant is given formula to drink. Rarely, there are peristaltic waves that may be felt or seen (video on NEJM) due to the stomach trying to force its contents past the narrowed pyloric outlet.
Most cases of pyloric stenosis are diagnosed/confirmed with ultrasound, if available, showing the thickened pylorus and non-passage of gastric contents into the proximal duodenum. Muscle wall thickness 3 millimeters (mm) or greater and pyloric channel length of 15 mm or greater are considered abnormal in infants younger than 30 days.[16]
Although somewhat less useful, an upper GI series (x-rays taken after the baby drinks a special contrast agent) can be diagnostic by showing the narrowed pyloric outlet filled with a thin stream of contrast material; a "string sign" or the "railroad track sign". For either type of study, there are specific measurement criteria used to identify the abnormal results. Plain x-rays of the abdomen sometimes shows a dilated stomach as shown here.
Although UGI endoscopy would demonstrate pyloric obstruction, physicians would find it difficult to differentiate accurately between hypertrophic pyloric stenosis and pylorospasm.
Blood tests will reveal low blood levels of potassium and chloride in association with an increased blood pH and high blood bicarbonate level due to loss of stomach acid (which contains hydrochloric acid) from persistent vomiting. There will be exchange of extracellular potassium with intracellular hydrogen ions in an attempt to correct the pH imbalance. These findings can be seen with severe vomiting from any cause.
Treatment


Infantile pyloric stenosis is typically managed with surgery;[17] very few cases are mild enough to be treated medically.
The danger of pyloric stenosis comes from the dehydration and electrolyte disturbance rather than the underlying problem itself. Therefore, the baby must be initially stabilized by correcting the dehydration and the abnormally high blood pH seen in combination with low chloride levels with IV fluids. This can usually be accomplished in about 24–48 hours.
Intravenous and oral atropine may be used to treat pyloric stenosis. It has a success rate of 85-89% compared to nearly 100% for pyloromyotomy, however it requires prolonged hospitalization, skilled nursing and careful follow up during treatment.[18] It might be an alternative to surgery in children who have contraindications for anesthesia or surgery, or in children whose parents do not want surgery.
Surgery
The definitive treatment of pyloric stenosis is with surgical pyloromyotomy known as Ramstedt's procedure (dividing the muscle of the pylorus to open up the gastric outlet). This surgery can be done through a single incision (usually 3–4 cm long) or laparoscopically (through several tiny incisions), depending on the surgeon's experience and preference.[19]
Today, the laparoscopic technique has largely supplanted the traditional open repairs which involved either a tiny circular incision around the navel or the Ramstedt procedure. Compared to the older open techniques, the complication rate is equivalent, except for a markedly lower risk of wound infection.[20] This is now considered the standard of care at the majority of children's hospitals across the US, although some surgeons still perform the open technique. Following repair, the small 3mm incisions are hard to see.
The vertical incision, pictured and listed above, is no longer usually required, though many incisions have been horizontal in the past years.
Once the stomach can empty into the duodenum, feeding can begin again. Some vomiting may be expected during the first days after surgery as the gastrointestinal tract settles. Rarely, the myotomy procedure performed is incomplete and projectile vomiting continues, requiring repeat surgery. Pyloric stenosis generally has no long term side-effects or impact on the child's future.
Epidemiology
Males are more commonly affected than females, with firstborn males affected about four times as often, and there is a genetic predisposition for the disease.[21] It is commonly associated with people of Scandinavian ancestry, and has multifactorial inheritance patterns.[10] Pyloric stenosis is more common in Caucasians than Hispanics, Blacks, or Asians. The incidence is 2.4 per 1000 live births in Caucasians, 1.8 in Hispanics, 0.7 in Blacks, and 0.6 in Asians. It is also less common amongst children of mixed race parents.[22] Caucasian male babies with blood type B or O are more likely than other types to be affected.[21]
Infants exposed to erythromycin are at increased risk for developing hypertrophic pyloric stenosis, especially when the drug is taken around two weeks of life[23] and possibly in late pregnancy and through breastmilk in the first two weeks of life.[24]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Ranells, JD; Carver, JD; Kirby, RS (2011). "Infantile hypertrophic pyloric stenosis: epidemiology, genetics, and clinical update.". Advances in pediatrics. 58 (1): 195–206. PMID 21736982.
- 1 2 3 Georgoula, C; Gardiner, M (August 2012). "Pyloric stenosis a 100 years after Ramstedt.". Archives of disease in childhood. 97 (8): 741–5. PMID 22685043.
- 1 2 Zhu, J; Zhu, T; Lin, Z; Qu, Y; Mu, D (15 March 2017). "Perinatal risk factors for infantile hypertrophic pyloric stenosis: A meta-analysis.". Journal of pediatric surgery. PMID 28318599.
- 1 2 Pandya, S; Heiss, K (June 2012). "Pyloric stenosis in pediatric surgery: an evidence-based review.". The Surgical clinics of North America. 92 (3): 527–39, vii–viii. PMID 22595707.
- ↑ Marsicovetere, P; Ivatury, SJ; White, B; Holubar, SD (February 2017). "Intestinal Intussusception: Etiology, Diagnosis, and Treatment.". Clinics in colon and rectal surgery. 30 (1): 30–39. PMID 28144210.
- ↑ Hellan, M; Lee, T; Lerner, T (February 2006). "Diagnosis and therapy of primary hypertrophic pyloric stenosis in adults: case report and review of literature.". Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 10 (2): 265–9. PMID 16455460.
- ↑ "Pyloric stenosis: Symptoms". MayoClinic.com. 2010-08-21. Retrieved 2012-02-21.
- ↑ Krogh, C.; Gortz, S.; Wohlfahrt, J.; Biggar, R. J.; Melbye, M.; Fischer, T. K. (2012). "Pre- and Perinatal Risk Factors for Pyloric Stenosis and Their Influence on the Male Predominance". American Journal of Epidemiology. 176 (1): 24–31. ISSN 0002-9262. doi:10.1093/aje/kwr493.
- ↑ Webb, A. R.; Lari, J.; Dodge, J. (1983). "Infantile hypertrophic pyloric stenosis in South Glamorgan 1970-79.". Arch. Dis. Child. 58: 586–90. doi:10.1136/adc.58.8.586.
- 1 2 Fried K, Aviv S, Nisenbaum C (November 1981). "Probable autosomal dominant infantile pyloric stenosis in a large kindred". Clin. Genet. 20 (5): 328–30. PMID 7333028. doi:10.1111/j.1399-0004.1981.tb01043.x.
- ↑ Rogers, Ian; Vanderbom, Frederick (2014-02-26). The Consequence and Cause of Pyloric Stenosis of Infancy. More Books Lembert Academic Publishers. ISBN 978-3-659-52125-6.
- ↑ Rogers, I.M. (2014). "Pyloric stenosis of infancy and primary hyperacidity-the missing link.". Acta Paediatrica. 103: e558–e560. doi:10.1111/apa.12795.
- ↑ Kerry Brandis, Acid-Base Physiology. Retrieved December 31, 2006.
- ↑ Dawes, Laughlin. "Pyloric stenosis | Radiology Case | Radiopaedia.org". radiopaedia.org. Retrieved 20 April 2017.
- ↑ Shaoul R, Enav B, Steiner Z, Mogilner J, Jaffe M (2004). "Clinical presentation of pyloric stenosis: the change is in our hands" (PDF). Isr Med Assoc J. 6 (3): 134–7. ISSN 1565-1088. PMID 15055266.
- ↑ Rohrschneider, WK; Mittnacht, H; Darge, K; Tröger, J (June 1998). "Pyloric muscle in asymptomatic infants: sonographic evaluation and discrimination from idiopathic hypertrophic pyloric stenosis.". Pediatric radiology. 28 (6): 429–34. PMID 9634457.
- ↑ Askew, Nathan (October 2010). "An overview of infantile hypertrophic pyloric stenosis.". Paediatric nursing. 22 (8): 27–30. PMID 21066945. doi:10.7748/paed.22.8.27.s27. Retrieved 30 August 2012.
- ↑ Aspelund G, Langer JC (February 2007). "Current management of hypertrophic pyloric stenosis". Semin. Pediatr. Surg. 16 (1): 27–33. PMID 17210480. doi:10.1053/j.sempedsurg.2006.10.004.
- ↑ "Medical News:Laparoscopic Repair of Pediatric Pyloric Stenosis May Speed Recovery - in Surgery, Thoracic Surgery from". MedPage Today. 2009-01-16. Retrieved 2012-02-21.
- ↑ Sola JE, Neville HL (August 2009). "Laparoscopic vs open pyloromyotomy: a systematic review and meta-analysis". J. Pediatr. Surg. 44 (8): 1631–7. PMID 19635317. doi:10.1016/j.jpedsurg.2009.04.001.
- 1 2 Dowshen, Steven (November 2007). "Pyloric Stenosis". The Nemours Foundation. Retrieved 2007-12-30.
- ↑ Pediatrics, Pyloric Stenosis at eMedicine
- ↑ Maheshwai, Nitin (March 2007). "Are young infants treated with erythromycin at risk for developing hypertrophic pyloric stenosis?". Archives of Disease in Childhood. 92 (3): 271–3. PMC 2083424
 . PMID 17337692. doi:10.1136/adc.2006.110007. Retrieved 30 August 2012.
. PMID 17337692. doi:10.1136/adc.2006.110007. Retrieved 30 August 2012. - ↑ Kong YL, Tey HL (June 2013). "Treatment of acne vulgaris during pregnancy and lactation". Drugs. 73 (8): 779–87. PMID 23657872. doi:10.1007/s40265-013-0060-0.
External links
| Classification |
V · T · D |
|---|---|
| External resources |