Huntington's disease
| Huntington's disease | |
|---|---|
| Synonyms | Huntington's chorea |
 | |
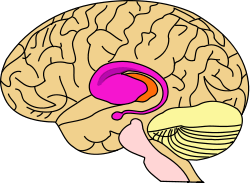
| An edited microscopic image of medium spiny neurons (yellow) with nuclear inclusions (orange), which occur as part of the disease process, image width 360 µm | |
| Specialty | Neurology |
| Symptoms | Problems with mood, mental abilities, coordination, jerky body movements[1][2] |
| Complications | Pneumonia, heart disease, physical injury from falls, suicide[3] |
| Usual onset | 30 and 50 years old[4] |
| Duration | Long term[4] |
| Causes | Genetic (inherited or new mutation)[4] |
| Diagnostic method | Genetic testing[5] |
| Similar conditions | Sydenham's chorea, benign hereditary chorea, lupus, paraneoplastic syndrome, Wilson's disease[6] |
| Treatment | Supportive care[2] |
| Medication | Tetrabenazine[3] |
| Prognosis | 15–20 years from diagnosis[4] |
| Frequency | 4–15 in 100,000 (European descent)[1] |
Huntington's disease (HD), also known as Huntington's chorea, is an inherited disorder that results in death of brain cells.[4] The earliest symptoms are often subtle problems with mood or mental abilities.[1] A general lack of coordination and an unsteady gait often follow.[2] As the disease advances, uncoordinated, jerky body movements become more apparent.[1] Physical abilities gradually worsen until coordinated movement becomes difficult and the person is unable to talk.[1][2] Mental abilities generally decline into dementia.[3] The specific symptoms vary somewhat between people.[1] Symptoms usually begin between 30 and 50 years of age, but can start at any age.[4][3] The disease may develop earlier in life in each successive generation.[1] About 8% of cases start before the age of 20 years and typically present with symptoms more similar to Parkinson's disease.[3] People with HD often underestimate the degree of their problems.[1]
HD is typically inherited from a person's parents, with 10% of cases due to a new mutation.[1] The disease is caused by an autosomal dominant mutation in either of an individual's two copies of a gene called Huntingtin. This means a child of an affected person typically has a 50% chance of inheriting the disease.[4] The Huntingtin gene provides the genetic information for a protein that is also called "huntingtin".[1] Expansion of CAG (cytosine-adenine-guanine) triplet repeats in the gene coding for the Huntingtin protein results in an abnormal protein, which gradually damages cells in the brain, through mechanisms that are not fully understood.[4] Diagnosis is by genetic testing, which can be carried out at any time, regardless of whether or not symptoms are present.[5] This fact raises several ethical debates: the age at which an individual is considered mature enough to choose testing; whether parents have the right to have their children tested; and managing confidentiality and disclosure of test results.[2]
There is no cure for HD.[4] Full-time care is required in the later stages of the disease.[2] Treatments can relieve some symptoms and in some improve quality of life. The best evidence for treatment of the movement problems is with tetrabenazine.[3] HD affects about 4 to 15 in 100,000 people of European descent.[1][3] It is rare among Japanese, while the occurrence rate in Africa is unknown. The disease affects men and women equally.[3] Complications such as pneumonia, heart disease, and physical injury from falls reduce life expectancy. Suicide is the cause of death in about 9% of cases.[3] Death typically occurs fifteen to twenty years from when the disease was first detected.[4]
The first likely description of the disease was in 1841 by Charles Oscar Waters. The condition was described in further detail in 1872 by George Huntington, after whom it is named.[7] The genetic basis was discovered in 1993 by an international collaborative effort led by the Hereditary Disease Foundation.[8][9] Research and support organizations began forming in the late 1960s to increase public awareness, to provide support for individuals and their families, and to promote research.[9][10] Current research directions include determining the exact mechanism of the disease, improving animal models to aid with research, testing of medications to treat symptoms or slow the progression of the disease, and studying procedures such as stem cell therapy with the goal of repairing damage caused by the disease.[8]
Signs and symptoms
| Irritability | 38–73% |
| Apathy | 34–76% |
| Anxiety | 34–61% |
| Depressed mood | 33–69% |
| Obsessive and compulsive | 10–52% |
| Psychotic | 3–11% |
Symptoms of Huntington's disease most commonly become noticeable between the ages of 35 and 44 years, but they can begin at any age from infancy to old age.[12][13] In the early stages, there are subtle changes in personality, cognition, and physical skills.[12] The physical symptoms are usually the first to be noticed, as cognitive and behavioral symptoms[14] are generally not severe enough to be recognized on their own at the earlier stages.[12] Almost everyone with Huntington's disease eventually exhibits similar physical symptoms, but the onset, progression and extent of cognitive and behavioral symptoms vary significantly between individuals.[15][16]
The most characteristic initial physical symptoms are jerky, random, and uncontrollable movements called chorea.[12] Chorea may be initially exhibited as general restlessness, small unintentionally initiated or uncompleted motions, lack of coordination, or slowed saccadic eye movements.[12] These minor motor abnormalities usually precede more obvious signs of motor dysfunction by at least three years.[15] The clear appearance of symptoms such as rigidity, writhing motions or abnormal posturing appear as the disorder progresses.[17] These are signs that the system in the brain that is responsible for movement has been affected.[18] Psychomotor functions become increasingly impaired, such that any action that requires muscle control is affected. Common consequences are physical instability, abnormal facial expression, and difficulties chewing, swallowing, and speaking.[17] Eating difficulties commonly cause weight loss and may lead to malnutrition.[19][20] Sleep disturbances are also associated symptoms.[21] Juvenile HD differs from these symptoms in that it generally progresses faster and chorea is exhibited briefly, if at all, with rigidity being the dominant symptom. Seizures are also a common symptom of this form of HD.[17]
Cognitive abilities are progressively impaired.[18] Especially affected are executive functions, which include planning, cognitive flexibility, abstract thinking, rule acquisition, initiation of appropriate actions, and inhibition of inappropriate actions.[18] As the disease progresses, memory deficits tend to appear. Reported impairments range from short-term memory deficits to long-term memory difficulties, including deficits in episodic (memory of one's life), procedural (memory of the body of how to perform an activity) and working memory.[18] Cognitive problems tend to worsen over time, ultimately leading to dementia.[18] This pattern of deficits has been called a subcortical dementia syndrome to distinguish it from the typical effects of cortical dementias e.g. Alzheimer's disease.[18]
Reported neuropsychiatric manifestations are anxiety, depression, a reduced display of emotions (blunted affect), egocentrism, aggression, and compulsive behavior, the latter of which can cause or worsen addictions, including alcoholism, gambling, and hypersexuality.[11] Difficulties in recognizing other people's negative expressions have also been observed.[18] The prevalence of these symptoms is highly variable between studies, with estimated rates for lifetime prevalence of psychiatric disorders between 33% and 76%.[11] For many sufferers and their families, these symptoms are among the most distressing aspects of the disease, often affecting daily functioning and constituting reason for institutionalization.[11] Suicidal thoughts and suicide attempts are more common than in the general population.[12] Often individuals have reduced awareness of chorea, cognitive and emotional impairments.[22]
Mutant Huntingtin is expressed throughout the body and associated with abnormalities in peripheral tissues that are directly caused by such expression outside the brain. These abnormalities include muscle atrophy, cardiac failure, impaired glucose tolerance, weight loss, osteoporosis, and testicular atrophy.[23]
Genetics
All humans have two copies of the Huntingtin gene (HTT), which codes for the protein Huntingtin (HTT). The gene is also called HD and IT15, which stands for 'interesting transcript 15'. Part of this gene is a repeated section called a trinucleotide repeat, which varies in length between individuals and may change length between generations. If the repeat is present in a healthy gene, a dynamic mutation may increase the repeat count and result in a defective gene. When the length of this repeated section reaches a certain threshold, it produces an altered form of the protein, called mutant Huntingtin protein (mHTT). The differing functions of these proteins are the cause of pathological changes which in turn cause the disease symptoms. The Huntington's disease mutation is genetically dominant and almost fully penetrant: mutation of either of a person's HTT alleles causes the disease. It is not inherited according to sex, but the length of the repeated section of the gene and hence its severity can be influenced by the sex of the affected parent.[24]
Genetic mutation
HD is one of several trinucleotide repeat disorders which are caused by the length of a repeated section of a gene exceeding a normal range.[25] The HTT gene is located on the short arm of chromosome 4[25] at 4p16.3. HTT contains a sequence of three DNA bases—cytosine-adenine-guanine (CAG)—repeated multiple times (i.e. ... CAGCAGCAG ...), known as a trinucleotide repeat.[25] CAG is the 3-letter genetic code (codon) for the amino acid glutamine, so a series of them results in the production of a chain of glutamine known as a polyglutamine tract (or polyQ tract), and the repeated part of the gene, the PolyQ region.[26]
| Repeat count | Classification | Disease status | Risk to offspring |
|---|---|---|---|
| <26 | Normal | Will not be affected | None |
| 27–35 | Intermediate | Will not be affected | Elevated but <<50% |
| 36–39 | Reduced Penetrance | May or may not be affected | 50% |
| 40+ | Full Penetrance | Will be affected | 50% |
Generally, people have fewer than 36 repeated glutamines in the polyQ region which results in production of the cytoplasmic protein Huntingtin.[25] However, a sequence of 36 or more glutamines results in the production of a protein which has different characteristics.[25] This altered form, called mutant huntingtin (mHTT), increases the decay rate of certain types of neurons. Regions of the brain have differing amounts and reliance on these types of neurons, and are affected accordingly.[17] Generally, the number of CAG repeats is related to how much this process is affected, and accounts for about 60% of the variation of the age of the onset of symptoms. The remaining variation is attributed to environment and other genes that modify the mechanism of HD.[25] 36–39 repeats result in a reduced-penetrance form of the disease, with a much later onset and slower progression of symptoms. In some cases the onset may be so late that symptoms are never noticed.[27] With very large repeat counts, HD has full penetrance and can occur under the age of 20, when it is then referred to as juvenile HD, akinetic-rigid, or Westphal variant HD. This accounts for about 7% of HD carriers.[28]
Inheritance

Huntington's disease has autosomal dominant inheritance, meaning that an affected individual typically inherits one copy of the gene with an expanded trinucleotide repeat (the mutant allele) from an affected parent.[12] Since penetrance of the mutation is very high, those who have a mutated copy of the gene will have the disease. In this type of inheritance pattern, each offspring of an affected individual has a 50% risk of inheriting the mutant allele and therefore being affected with the disorder (see figure). This probability is sex-independent.[29]
Trinucleotide CAG repeats over 28 are unstable during replication, and this instability increases with the number of repeats present.[27] This usually leads to new expansions as generations pass (dynamic mutations) instead of reproducing an exact copy of the trinucleotide repeat.[25] This causes the number of repeats to change in successive generations, such that an unaffected parent with an "intermediate" number of repeats (28–35), or "reduced penetrance" (36–40), may pass on a copy of the gene with an increase in the number of repeats that produces fully penetrant HD.[25] Such increases in the number of repeats (and hence earlier age of onset and severity of disease) in successive generations is known as genetic anticipation.[25] Instability is greater in spermatogenesis than oogenesis;[25] maternally inherited alleles are usually of a similar repeat length, whereas paternally inherited ones have a higher chance of increasing in length.[25][30] It is rare for Huntington's disease to be caused by a new mutation, where neither parent has over 36 CAG repeats.[31]
In the rare situations where both parents have an expanded HD gene, the risk increases to 75%, and when either parent has two expanded copies, the risk is 100% (all children will be affected). Individuals with both genes affected are rare. For some time HD was thought to be the only disease for which possession of a second mutated gene did not affect symptoms and progression,[32] but it has since been found that it can affect the phenotype and the rate of progression.[25][33]
Mechanism
The huntingtin protein interacts with over 100 other proteins, and appears to have multiple biological functions.[34] The behavior of this mutated protein is not completely understood, but it is toxic to certain cell types, particularly in the brain. Early damage is most evident in the striatum, but as the disease progresses, other areas of the brain are also more conspicuously affected. Early symptoms are attributable to functions of the striatum and its cortical connections—namely control over movement, mood and higher cognitive function.[24] DNA methylation also appears to be changed in HD.[35]
Huntingtin function
HTT is expressed in all mammalian cells. The highest concentrations are found in the brain and testes, with moderate amounts in the liver, heart, and lungs.[24] The function of HTT in humans is unclear. It interacts with proteins which are involved in transcription, cell signaling, and intracellular transporting.[24][36] In animals genetically modified to exhibit HD, several functions of HTT have been found.[37] In these animals, HTT is important for embryonic development, as its absence is related to embryonic death. Caspase, an enzyme which plays a role in catalyzing apoptosis, is thought to be activated by the mutated gene through damaging the ubiquitin-protease system. It also acts as an anti-apoptotic agent preventing programmed cell death and controls the production of brain-derived neurotrophic factor, a protein which protects neurons and regulates their creation during neurogenesis. HTT also facilitates vesicular transport and synaptic transmission and controls neuronal gene transcription.[37] If the expression of HTT is increased and more HTT produced, brain cell survival is improved and the effects of mHTT are reduced, whereas when the expression of HTT is reduced, the resulting characteristics are more typical of the presence of mHTT.[37] In humans the disruption of the normal gene does not cause the disease.[24] It is thought that the disease is not caused by inadequate production of HTT, but by a gain of toxic function of mHTT.[24]
Cellular changes

There are multiple cellular changes through which the toxic function of mHTT may manifest and produce the HD pathology.[38][39] During the biological process of posttranslational modification of mHTT, cleavage of the protein can leave behind shorter fragments constituted of parts of the polyglutamine expansion.[38] The polar nature of glutamine causes interactions with other proteins when it is overabundant in unmodified HTT proteins or the HTT fragments created from HTT cleavage. Thus, the mHTT molecule strands will form hydrogen bonds with one another, forming a protein aggregate rather than folding into functional proteins.[40] Over time, the aggregates accumulate, ultimately interfering with neuron function because these fragments can then misfold and coalesce, in a process called protein aggregation, to form inclusion bodies within cells.[38][40] Neuronal inclusions run indirect interference. Inclusion bodies have been found in both the cell nucleus and cytoplasm.[38] Inclusion bodies in cells of the brain are one of the earliest pathological changes, and some experiments have found that they can be toxic for the cell, but other experiments have shown that they may form as part of the body's defense mechanism and help protect cells.[38]
Several pathways by which mHTT may cause cell death have been identified. These include: effects on chaperone proteins, which help fold proteins and remove misfolded ones; interactions with caspases, which play a role in the process of removing cells; the toxic effects of glutamine on nerve cells; impairment of energy production within cells; and effects on the expression of genes.[40][41]
An additional theory that explains another way cell function may be disrupted by HD proposes that damage to mitochondria in striatal cells (numerous accounts of mitochondrial metabolism deficiency have been found) and the interactions of the altered huntingtin protein with numerous proteins in neurons leads to an increased vulnerability of glutamine, which, in large amounts, has been found to be an excitotoxin. Excitotoxins may cause damage to numerous cellular structures. Although glutamine is not found in excessively high amounts, it has been postulated that because of the increased vulnerability, even normal amounts glutamine can cause excitotoxins to be expressed.[40]
Macroscopic changes
HD affects the whole brain, but certain areas are more vulnerable than others. The most prominent early effects are in a part of the basal ganglia called the neostriatum, which is composed of the caudate nucleus and putamen.[24] Other areas affected include the substantia nigra, layers 3, 5 and 6 of the cerebral cortex, the hippocampus, purkinje cells in the cerebellum, lateral tuberal nuclei of the hypothalamus and parts of the thalamus.[25] These areas are affected according to their structure and the types of neurons they contain, reducing in size as they lose cells.[25] Striatal spiny neurons are the most vulnerable, particularly ones with projections towards the external globus pallidus, with interneurons and spiny cells projecting to the internal pallidum being less affected.[25][42] HD also causes an abnormal increase in astrocytes and activation of the brain's immune cells, microglia.[43]
The basal ganglia—the part of the brain most prominently affected in early HD—play a key role in movement and behavior control. Their functions are not fully understood, but current theories propose that they are part of the cognitive executive system[18] and the motor circuit.[44] The basal ganglia ordinarily inhibit a large number of circuits that generate specific movements. To initiate a particular movement, the cerebral cortex sends a signal to the basal ganglia that causes the inhibition to be released. Damage to the basal ganglia can cause the release or reinstatement of the inhibitions to be erratic and uncontrolled, which results in an awkward start to motion or motions to be unintentionally initiated, or a motion to be halted before, or beyond, its intended completion. The accumulating damage to this area causes the characteristic erratic movements associated with HD.[44] The spontaneous and erratic physical movements associated with HD are classified as a type of hyperkinetic dysarthria. Because of the basal ganglia's inability to inhibit movements, individuals affected by it will inevitably experience a reduced ability to produce speech and swallow foods and liquids (dysphagia).[45]
Transcriptional dysregulation
CREB-binding protein (CBP), a transcriptional coregulator, is essential for cell function because as a coactivator at a significant number of promoters, it activates the transcription of genes for survival pathways.[41] Furthermore, the amino acids that form CBP include a strip of 18 glutamines. Thus, the glutamines on CBP interact directly with the increased numbers of glutamine on the HTT chain and CBP gets pulled away from its typical location next to the nucleus.[46] Specifically, CBP contains an acetyltransferase domain to which HTT binds through its polyglutamine-containing domain.[47] Autopsied brains of those who had Huntington's disease also have been found to have incredibly reduced amounts of CBP.[46] In addition, when CBP is overexpressed, polyglutamine-induced death is diminished, further demonstrating that CBP plays an important role in Huntington's disease and neurons in general.[41]
Diagnosis
Medical diagnosis of the onset of HD can be made following the appearance of physical symptoms specific to the disease.[12] Genetic testing can be used to confirm a physical diagnosis if there is no family history of HD. Even before the onset of symptoms, genetic testing can confirm if an individual or embryo carries an expanded copy of the trinucleotide repeat in the HTT gene that causes the disease. Genetic counseling is available to provide advice and guidance throughout the testing procedure, and on the implications of a confirmed diagnosis. These implications include the impact on an individual's psychology, career, family planning decisions, relatives and relationships. Despite the availability of pre-symptomatic testing, only 5% of those at risk of inheriting HD choose to do so.[24]
Clinical

A physical examination, sometimes combined with a psychological examination, can determine whether the onset of the disease has begun.[12] Excessive unintentional movements of any part of the body are often the reason for seeking medical consultation. If these are abrupt and have random timing and distribution, they suggest a diagnosis of HD. Cognitive or behavioral symptoms are rarely the first symptoms diagnosed; they are usually only recognized in hindsight or when they develop further. How far the disease has progressed can be measured using the unified Huntington's disease rating scale, which provides an overall rating system based on motor, behavioral, cognitive, and functional assessments.[49][50] Medical imaging, such as computerized tomography (CT) and magnetic resonance imaging (MRI), can show atrophy of the caudate nuclei early in the disease, as seen in the illustration to the right, but these changes are not, by themselves, diagnostic of HD. Cerebral atrophy can be seen in the advanced stages of the disease. Functional neuroimaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), can show changes in brain activity before the onset of physical symptoms, but they are experimental tools, and are not used clinically.[25]
Predictive genetic testing
Because HD follows an autosomal dominant pattern of inheritance, there is a strong motivation for individuals who are at risk of inheriting it to seek a diagnosis. The genetic test for HD consists of a blood test which counts the numbers of CAG repeats in each of the HTT alleles.[51] Cutoffs are given as follows:
- 40 or more CAG repeats: full penetrance allele (FPA).[52] A "positive test" or "positive result" generally refers to this case. A positive result is not considered a diagnosis, since it may be obtained decades before the symptoms begin. However, a negative test means that the individual does not carry the expanded copy of the gene and will not develop HD.[25] The test will tell a person who originally had a 50 percent chance of inheriting the disease if their risk goes up to 100 percent or is eliminated. A person who tests positive for the disease will develop HD sometime within their lifetime, provided he or she lives long enough for the disease to appear.[25]
- 36 to 39 repeats: incomplete or reduced penetrance allele (RPA). It may cause symptoms, usually later in the adult life.[52] There is a maximum risk of 60% that a person with an RPA will be symptomatic at the age of 65 years, and a 70% risk of being symptomatic at the age of 75 years.[52]
- 27 to 35 repeats: intermediate allele (IA), or large normal allele. It is not associated with symptomatic disease in the tested individual, but may expand upon further inheritance to give symptoms in offspring.[52]
- 26 or fewer repeats: Not associated with HD.[52]
A pre-symptomatic test is a life-changing event and a very personal decision.[25] The main reason given for choosing testing for HD is to aid in career and family decisions.[25] Before 1993 there was not an available test for individuals to learn if they carried the Huntington's gene. At that time surveys indicated that 50–70% of at-risk individuals would have been interested in receiving testing, but since predictive testing has been offered far fewer choose to be tested.[53] Over 95% of individuals at risk of inheriting HD do not proceed with testing, mostly because there is no treatment.[25] A key issue is the anxiety an individual experiences about not knowing whether they will eventually develop HD, compared to the impact of a positive result.[24] Irrespective of the result, stress levels have been found to be lower two years after being tested, but the risk of suicide is increased after a positive test result.[24] Individuals found to have not inherited the disorder may experience survivor guilt with regard to family members who are affected.[24] Other factors taken into account when considering testing include the possibility of discrimination and the implications of a positive result, which usually means a parent has an affected gene and that the individual's siblings will be at risk of inheriting it.[24] In one study genetic discrimination was found in 46% of individuals at risk for Huntington's disease. It occurred at higher rates within personal relationships than health insurance or employment relations.[54] Genetic counseling in HD can provide information, advice and support for initial decision-making, and then, if chosen, throughout all stages of the testing process.[55] Because of the implications of this test, patients who wish to undergo testing must complete three counseling sessions which provide information about Huntington's.[56]
Counseling and guidelines on the use of genetic testing for HD have become models for other genetic disorders, such as autosomal dominant cerebellar ataxias.[24][57][58] Presymptomatic testing for HD has also influenced testing for other illnesses with genetic variants such as polycystic kidney disease, familial Alzheimer's disease and breast cancer.[57] The European Molecular Genetics Quality Network have published yearly external quality assessment scheme for molecular genetic testing for this disease and have developed best practice guidelines for genetic testing for HD to assist in testing and reporting of results.[59]
Preimplantation genetic diagnosis
Embryos produced using in vitro fertilization may be genetically tested for HD using preimplantation genetic diagnosis (PGD). This technique, where one or two cells are extracted from a typically 4- to 8-cell embryo and then tested for the genetic abnormality, can then be used to ensure embryos affected with HD genes are not implanted, and therefore any offspring will not inherit the disease. Some forms of preimplantation genetic diagnosis—non-disclosure or exclusion testing—allow at-risk people to have HD-free offspring without revealing their own parental genotype, giving no information about whether they themselves are destined to develop HD. In exclusion testing, the embryos' DNA is compared with that of the parents and grandparents to avoid inheritance of the chromosomal region containing the HD gene from the affected grandparent. In non-disclosure testing, only disease-free embryos are replaced in the uterus while the parental genotype and hence parental risk for HD are never disclosed.[60][61]
Prenatal testing
It is also possible to obtain a prenatal diagnosis for an embryo or fetus in the womb, using fetal genetic material acquired through chorionic villus sampling. An amniocentesis can be performed if the pregnancy is further along, within 14–18 weeks. This procedure looks at the amniotic fluid surrounding the baby for indicators of the HD mutation.[62] This, too, can be paired with exclusion testing to avoid disclosure of parental genotype. Prenatal testing can be done when a parent has been diagnosed with HD, when they have had genetic testing showing the expansion of the HTT gene, or when they have a 50% chance of inheriting the disease. The parents can be counseled on their options, which include termination of pregnancy, and on the difficulties of a child with the identified gene.[63][64]
In addition, in at-risk pregnancies due to an affected male partner, non-invasive prenatal diagnosis can be performed by analyzing cell-free fetal DNA in a blood sample taken from the mother (via venipuncture) between six and twelve weeks of pregnancy.[52] It has no procedure-related risk of miscarriage (excepting via needle contamination).[52]
Differential diagnosis
About 99% of HD diagnoses based on the typical symptoms and a family history of the disease are confirmed by genetic testing to have the expanded trinucleotide repeat that causes HD. Most of the remaining are called HD-like (HDL) syndromes.[17][65] The cause of most HDL diseases is unknown, but those with known causes are due to mutations in the prion protein gene (HDL1), the junctophilin 3 gene (HDL2), a recessively inherited unknown gene (HDL3—only found in two families and poorly understood), and the gene encoding the TATA box-binding protein (SCA17, sometimes called HDL4). Other autosomal dominant diseases that can be misdiagnosed as HD are dentatorubral-pallidoluysian atrophy and neuroferritinopathy. There are also autosomal recessive disorders that resemble sporadic cases of HD. These include chorea acanthocytosis and pantothenate kinase-associated neurodegeneration. One X-linked disorder of this type is McLeod syndrome.[65]
Management

There is no cure for HD, but there are treatments available to reduce the severity of some of its symptoms.[66] For many of these treatments, evidence to confirm their effectiveness in treating symptoms of HD specifically are incomplete.[67][68] As the disease progresses the ability to care for oneself declines, and carefully managed multidisciplinary caregiving becomes increasingly necessary.[67] Although there have been relatively few studies of exercises and therapies that help rehabilitate cognitive symptoms of HD, there is some evidence for the usefulness of physical therapy, occupational therapy, and speech therapy.[12] An association between caffeine intake and earlier age of onset in Huntington's disease has been found[69][70] but, since this finding was based on retrospective questionnaire data rather than a blinded, randomized trial or case-control study, this work is a poor basis for guiding lifestyle decisions.[71]
Therapy
Weight loss and eating difficulties due to dysphagia and other muscle discoordination are common, making nutrition management increasingly important as the disease advances.[67] Thickening agents can be added to liquids as thicker fluids are easier and safer to swallow.[67] Reminding the affected person to eat slowly and to take smaller pieces of food into the mouth may also be of use to prevent choking.[67] If eating becomes too hazardous or uncomfortable, the option of using a percutaneous endoscopic gastrostomy is available. This is a feeding tube, permanently attached through the abdomen into the stomach, which reduces the risk of aspirating food and provides better nutritional management.[72] Assessment and management by speech-language pathologists with experience in Huntington's disease is recommended.[12]
People with Huntington's disease may see a physical therapist for non-invasive and non-medication-based ways of managing the physical symptoms. Physical therapists may implement fall risk assessment and prevention, as well as strengthening, stretching, and cardiovascular exercises. Walking aids may be prescribed as appropriate. Physical therapists also prescribe breathing exercises and airway clearance techniques with the development of respiratory problems.[73] Consensus guidelines on physiotherapy in Huntington's disease have been produced by the European HD Network.[73] Goals of early rehabilitation interventions are prevention of loss of function. Participation in rehabilitation programs during early to middle stage of the disease may be beneficial as it translates into long term maintenance of motor and functional performance. Rehabilitation during the late stage aims to compensate for motor and functional losses.[74] For long-term independent management, the therapist may develop home exercise programs for appropriate people.[75]
Additionally, an increasing number of people with Huntington’s disease are turning to palliative care, which aims to improve quality of life through the treatment of the symptoms and stress of serious illness, in addition to their other treatments.[76]
Medications
Tetrabenazine was approved in 2008 for treatment of chorea in Huntington's disease in the US.[77] Other drugs that help to reduce chorea include neuroleptics and benzodiazepines.[13] Compounds such as amantadine or remacemide are still under investigation but have shown preliminary positive results.[78] Hypokinesia and rigidity, especially in juvenile cases, can be treated with antiparkinsonian drugs, and myoclonic hyperkinesia can be treated with valproic acid.[13]
Psychiatric symptoms can be treated with medications similar to those used in the general population.[67][68] Selective serotonin reuptake inhibitors and mirtazapine have been recommended for depression, while atypical antipsychotic drugs are recommended for psychosis and behavioral problems.[68] Specialist neuropsychiatric input is recommended as people may require long-term treatment with multiple medications in combination.[12]
Education
The families of individuals who have inherited or are at risk of inheriting HD have generations of experience of HD, but may be unaware of recent breakthroughs in understanding the disease, and of the availability of genetic testing. Genetic counseling benefits these individuals by updating their knowledge, seeking to dispel any unfounded beliefs that they may have, and helping them consider their future options and plans. Also covered is information concerning family planning choices, care management, and other considerations.[24][79]
Prognosis
The length of the trinucleotide repeat accounts for 60% of the variation in the age symptoms appear and the rate they progress. A longer repeat results in an earlier age of onset and a faster progression of symptoms.[25][80] Individuals with more than sixty repeats often develop the disease before age 20, while those with fewer than 40 repeats may not ever develop noticeable symptoms.[81] The remaining variation is due to environmental factors and other genes that influence the mechanism of the disease.[25]
Life expectancy in HD is generally around 20 years following the onset of visible symptoms.[17] Most life-threatening complications result from muscle coordination and, to a lesser extent, behavioral changes induced by declining cognitive function. The largest risk is pneumonia, which causes death in one third of those with HD. As the ability to synchronize movements deteriorates, difficulty clearing the lungs and an increased risk of aspirating food or drink both increase the risk of contracting pneumonia. The second greatest risk is heart disease, which causes almost a quarter of fatalities of those with HD.[17] Suicide is the third greatest cause of fatalities, with 7.3% of those with HD taking their own lives and up to 27% attempting to do so. It is unclear to what extent suicidal thoughts are influenced by behavioral symptoms, as they signify sufferers' desires to avoid the later stages of the disease.[82][83][84] Other associated risks include choking, physical injury from falls, and malnutrition.[17]
Epidemiology
The late onset of Huntington's disease means it does not usually affect reproduction.[24] The worldwide prevalence of HD is 5–10 cases per 100,000 persons,[85][86] but varies greatly geographically as a result of ethnicity, local migration and past immigration patterns.[24] Prevalence is similar for men and women. The rate of occurrence is highest in peoples of Western European descent, averaging around 7 per 100,000 people, and is lower in the rest of the world; e.g., one per million people of Asian and African descent. A 2013 epidemiological study of the prevalence of Huntington's disease in the UK between 1990 and 2010 found that the average prevalence for the UK was 12.3 per 100,000.[24][87] Additionally, some localized areas have a much higher prevalence than their regional average.[24] One of the highest incidences is in the isolated populations of the Lake Maracaibo region of Venezuela, where HD affects up to 700 per 100,000 persons.[24][88] Other areas of high localization have been found in Tasmania and specific regions of Scotland, Wales and Sweden.[84] Increased prevalence in some cases occurs due to a local founder effect, a historical migration of carriers into an area of geographic isolation.[84][89] Some of these carriers have been traced back hundreds of years using genealogical studies.[84] Genetic haplotypes can also give clues for the geographic variations of prevalence.[84][90] Iceland, on the contrary, has a rather low prevalence of 1 per 100,000, despite the fact that Icelanders as a people are descended of the early Germanic tribes of Scandinavia which also gave rise to the Swedes; all cases with the exception of one going back nearly two centuries having derived from the offspring of a couple living early in the 19th century.[91] Finland, as well, has a low incidence of only 2.2 per 100,000 people.[92]
Until the discovery of a genetic test, statistics could only include clinical diagnosis based on physical symptoms and a family history of HD, excluding those who died of other causes before diagnosis. These cases can now be included in statistics; and, as the test becomes more widely available, estimates of the prevalence and incidence of the disorder are likely to increase.[84][93]
History
Although Huntington's has been recognized as a disorder since at least the Middle Ages, the cause has been unknown until fairly recently. Huntington's was given different names throughout this history as understanding of the disease changed. Originally called simply 'chorea' for the jerky dancelike movements associated with the disease, HD has also been called "hereditary chorea" and "chronic progressive chorea".[95] The first definite mention of HD was in a letter by Charles Oscar Waters, published in the first edition of Robley Dunglison's Practice of Medicine in 1842. Waters described "a form of chorea, vulgarly called magrums", including accurate descriptions of the chorea, its progression, and the strong heredity of the disease.[96] In 1846 Charles Gorman observed how higher prevalence seemed to occur in localized regions.[96] Independently of Gorman and Waters, both students of Dunglison at Jefferson Medical College in Philadelphia,[97] Johan Christian Lund also produced an early description in 1860.[96] He specifically noted that in Setesdalen, a secluded mountain valley in Norway, there was a high prevalence of dementia associated with a pattern of jerking movement disorders that ran in families.[98]
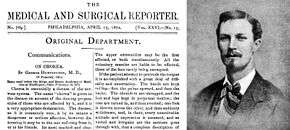
The first thorough description of the disease was by George Huntington in 1872. Examining the combined medical history of several generations of a family exhibiting similar symptoms, he realized their conditions must be linked; he presented his detailed and accurate definition of the disease as his first paper. Huntington described the exact pattern of inheritance of autosomal dominant disease years before the rediscovery by scientists of Mendelian inheritance.
"Of its hereditary nature. When either or both the parents have shown manifestations of the disease ..., one or more of the offspring almost invariably suffer from the disease ... But if by any chance these children go through life without it, the thread is broken and the grandchildren and great-grandchildren of the original shakers may rest assured that they are free from the disease.".[94][99]
Sir William Osler was interested in the disorder and chorea in general, and was impressed with Huntington's paper, stating that "In the history of medicine, there are few instances in which a disease has been more accurately, more graphically or more briefly described."[96][100] Osler's continued interest in HD, combined with his influence in the field of medicine, helped to rapidly spread awareness and knowledge of the disorder throughout the medical community.[96] Great interest was shown by scientists in Europe, including Louis Théophile Joseph Landouzy, Désiré-Magloire Bourneville, Camillo Golgi, and Joseph Jules Dejerine, and until the end of the century, much of the research into HD was European in origin.[96] By the end of the 19th century, research and reports on HD had been published in many countries and the disease was recognized as a worldwide condition.[96]
During the rediscovery of Mendelian inheritance at the turn of the 20th century, HD was used tentatively as an example of autosomal dominant inheritance.[96] The English biologist William Bateson used the pedigrees of affected families to establish that HD had an autosomal dominant inheritance pattern.[97] The strong inheritance pattern prompted several researchers, including Smith Ely Jelliffe, to attempt to trace and connect family members of previous studies.[96] Jelliffe collected information from across New York and published several articles regarding the genealogy of HD in New England.[101] Jelliffe's research roused the interest of his college friend, Charles Davenport, who commissioned Elizabeth Muncey to produce the first field study on the East Coast of the United States of families with HD and to construct their pedigrees.[102] Davenport used this information to document the variable age of onset and range of symptoms of HD; he claimed that most cases of HD in the USA could be traced back to a handful of individuals.[102] This research was further embellished in 1932 by P. R. Vessie, who popularized the idea that three brothers who left England in 1630 bound for Boston were the progenitors of HD in the USA.[103] The claim that the earliest progenitors had been established and eugenic bias of Muncey's, Davenport's, and Vessie's work contributed to misunderstandings and prejudice about HD.[97] Muncey and Davenport also popularized the idea that in the past some HD sufferers may have been thought to be possessed by spirits or victims of witchcraft, and were sometimes shunned or exiled by society.[104][105] This idea has not been proven. Researchers have found contrary evidence; for instance, the community of the family studied by George Huntington openly accommodated those who exhibited symptoms of HD.[97][104]
The search for the cause of this condition was enhanced considerably in 1968, when the Hereditary Disease Foundation (HDF) was created by Milton Wexler, a psychoanalyst based in Los Angeles, California, whose wife Leonore Sabin had been diagnosed earlier that year with Huntington's disease.[106] The three brothers of Wexler's wife also suffered from this disease. The foundation was involved in the recruitment of over 100 scientists in the Huntington's Disease Collaborative Research Project who over a 10-year period worked to locate the responsible gene.
Thanks to the HDF, the ongoing US-Venezuela Huntington's Disease Collaborative Research Project was started in 1979, and reported a major breakthrough in 1983 with the discovery of the approximate location of a causal gene.[89] This was the result of an extensive study focusing on the populations of two isolated Venezuelan villages, Barranquitas and Lagunetas, where there was an unusually high prevalence of the disease. It involved over 18,000 people—mostly from a single extended family.
Among other innovations, the project developed DNA-marking methods which were an important step in making the Human Genome Project possible.[107] In 1993, the research group isolated the precise causal gene at 4p16.3,[108] making this the first autosomal disease locus found using genetic linkage analysis.[108][109]
In the same time frame, key discoveries concerning the mechanisms of the disorder were being made, including the findings by Anita Harding's research group on the effects of the gene's length.[110]
Modelling the disease in various types of animals, such as the transgenic mouse developed in 1996, enabled larger scale experiments. As these animals have faster metabolisms and much shorter lifespans than humans, results from experiments are received sooner, speeding research. The 1997 discovery that mHTT fragments misfold led to the discovery of the nuclear inclusions they cause. These advances have led to increasingly extensive research into the proteins involved with the disease, potential drug treatments, care methods, and the gene itself.[96][111]
The condition was formerly called 'Huntington's chorea' but this term has been replaced by 'Huntington's disease' because not all patients develop chorea and due to the importance of cognitive and behavioral problems.[112]
Society and culture
Ethics
Huntington's disease, particularly the application of the genetic test for the disease, has raised several ethical issues. The issues for genetic testing include defining how mature an individual should be before being considered eligible for testing, ensuring the confidentiality of results, and whether companies should be allowed to use test results for decisions on employment, life insurance or other financial matters. There was controversy when Charles Davenport proposed in 1910 that compulsory sterilization and immigration control be used for people with certain diseases, including HD, as part of the eugenics movement.[113] In vitro fertilization has some issues regarding its use of embryos. Some HD research has ethical issues due to its use of animal testing and embryonic stem cells.[114][115]
The development of an accurate diagnostic test for Huntington's disease has caused social, legal, and ethical concerns over access to and use of a person's results.[116][117] Many guidelines and testing procedures have strict procedures for disclosure and confidentiality to allow individuals to decide when and how to receive their results and also to whom the results are made available.[24] Financial institutions and businesses are faced with the question of whether to use genetic test results when assessing an individual, such as for life insurance or employment. The United Kingdom's insurance companies have agreed that until 2017 they will not use genetic information when writing insurance policies under GB£500,000, but Huntington's is explicitly excluded from this agreement.[118][119] As with other untreatable genetic conditions with a later onset, it is ethically questionable to perform pre-symptomatic testing on a child or adolescent, as there would be no medical benefit for that individual. There is consensus for testing only individuals who are considered cognitively mature, although there is a counter-argument that parents have a right to make the decision on their child's behalf. With the lack of an effective treatment, testing a person under legal age who is not judged to be competent is considered unethical in most cases.[39][120][121]
There are ethical concerns related to prenatal genetic testing or preimplantation genetic diagnosis to ensure a child is not born with a given disease.[122] For example, prenatal testing raises the issue of selective abortion, a choice considered unacceptable by some.[122] As it is a dominant disease, there are difficulties in situations in which a parent does not want to know his or her own diagnosis. This would require parts of the process to be kept secret from the parent.[122]
Support organizations

In 1968, after experiencing HD in his wife's family, Dr. Milton Wexler was inspired to start the Hereditary Disease Foundation (HDF), with the aim of curing genetic illnesses by coordinating and supporting research.[9] The foundation and Wexler's daughter, Nancy Wexler, were key parts of the research team in Venezuela which discovered the HD gene.[9]
At roughly the same time as the HDF formed, Marjorie Guthrie helped to found the Committee to Combat Huntington's Disease (now the Huntington's Disease Society of America), after her husband Woody Guthrie died from complications of HD.[10]
Since then, support and research organizations have formed in many countries around the world and have helped to increase public awareness of HD. A number of these collaborate in umbrella organizations, like the International Huntington Association and the European HD network.[123] Many support organizations hold an annual HD awareness event, some of which have been endorsed by their respective governments. For example, 6 June is designated "National Huntington's Disease Awareness Day" by the US Senate.[124]
The largest funder of Huntington's disease research globally, in terms of financial expenditure,[125] is the CHDI Foundation, a US non-profit biomedical foundation that aims to "rapidly discover and develop drugs that delay or slow Huntington's disease".[126] CHDI was formerly known as the High Q Foundation. In 2006, it spent $50 million on Huntington's disease research.[125] CHDI collaborates with many academic and commercial laboratories globally and engages in oversight and management of research projects as well as funding.[127] Many organizations exist to support and inform those affected by HD.
Research directions
Research into the mechanism of HD has focused on identifying the functioning of HTT, how mHTT differs or interferes with it, and the brain pathology that the disease produces. Research is conducted using in vitro methods, animal models and human volunteers. Animal models are critical for understanding the fundamental mechanisms causing the disease and for supporting the early stages of drug development.[111] Animals with chemically induced brain injury exhibit HD-like symptoms and were initially used, but they did not mimic the progressive features of the disease.[128] The identification of the causative gene has enabled the development of many transgenic animal models including nematode worms, Drosophila fruit flies, mice, rats, sheep, pigs and monkeys that express mutant huntingtin and develop progressive neurodegeneration and HD-like symptoms.[111]
Research is being conducted on many different approaches to prevent Huntington's disease or slow its progression. Disease-modifying strategies can be broadly grouped into three categories: reducing the level of the mutant huntingtin protein (including gene splicing and gene silencing); approaches aimed at improving neuronal survival by reducing the harm caused by the protein to specific cellular pathways and mechanisms (including protein homeostasis and histone deacetylase inhibition); and strategies to replace lost neurons. In addition, novel therapies to improve brain functioning are under development; these seek to produce symptomatic rather than disease-modifying therapies, and include phosphodiesterase inhibitors.[129][130]
Reducing huntingtin production
Gene silencing aims to reduce the production of the mutant protein, since HD is caused by a single dominant gene encoding a toxic protein. Gene silencing experiments in mouse models have shown that when the expression of mHTT is reduced, symptoms improve.[131] Safety of non-allele specific RNAi and ASO gene silencing has now been demonstrated in mice and the large, human-like brains of primates.[132][133] Allele-specific silencing attempts to silence mutant HTT while leaving wild-type HTT untouched. One way of accomplishing this is to identify polymorphisms present on only one allele and produce gene silencing drugs that target polymorphisms in only the mutant allele.[134] The first 'gene silencing' trial involving human HD patients began in 2015, testing the safety of IONIS-HTTRx, produced by Ionis Pharmaceuticals and led by UCL Institute of Neurology.[135][136] Mutant huntingtin was detected and quantified for the first time in cerebrospinal fluid from Huntington's disease mutation-carriers in 2015 using a novel 'single-molecule counting' immunoassay,[137] providing a direct way to assess whether huntingtin-lowering treatments are achieving the desired effect.[138][139] Similarly, gene splicing techniques are being looked at to try to repair a genome with the erroneous gene that causes HD, using tools such as CRISPR/Cas9.[130]
Improving cell survival
Among the approaches aimed at improving cell survival in the presence of mutant huntingtin are correction of transcriptional regulation using histone deacetylase inhibitors, modulating aggregation of huntingtin, improving metabolism and mitochondrial function and restoring function of synapses.[131]
Neuronal replacement
Stem cell therapy is the replacement of damaged neurons by transplantation of stem cells into affected regions of the brain. Experiments have yielded mixed results using this technique in animal models and preliminary human clinical trials.[140] Whatever their future therapeutic potential, stem cells are already a valuable tool for studying Huntington's disease in the laboratory.[141]
Clinical trials
Several clinical trials of new experimental treatments are underway and planned in Huntington's disease.[142]
Compounds that have failed to prevent or slow progression of Huntington's disease in human trials include remacemide, coenzyme Q10, riluzole, creatine, minocycline, ethyl-EPA, phenylbutyrate and dimebon.[143]
References
- 1 2 3 4 5 6 7 8 9 10 11 Dayalu, P; Albin, RL (February 2015). "Huntington disease: pathogenesis and treatment.". Neurologic Clinics. 33 (1): 101–14. PMID 25432725. doi:10.1016/j.ncl.2014.09.003.
- 1 2 3 4 5 6 Warby, SC; Graham, RK; Hayden, MR; Pagon, RA; Adam, MP; Ardinger, HH; Wallace, SE; Amemiya, A; Bean, LJH; Bird, TD; Fong, CT; Mefford, HC; Smith, RJH; Stephens, K (2014). "Huntington Disease". PMID 20301482.
- 1 2 3 4 5 6 7 8 9 Frank, S (January 2014). "Treatment of Huntington's disease.". Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 11 (1): 153–60. PMC 3899480
 . PMID 24366610. doi:10.1007/s13311-013-0244-z.
. PMID 24366610. doi:10.1007/s13311-013-0244-z. - 1 2 3 4 5 6 7 8 9 10 "Huntington's Disease Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". NINDS. January 28, 2016. Retrieved 19 July 2016.
- 1 2 Durr, A; Gargiulo, M; Feingold, J (November 2012). "The presymptomatic phase of Huntington disease.". Revue neurologique. 168 (11): 806–8. PMID 22902173. doi:10.1016/j.neurol.2012.07.003.
- ↑ Ferri, Fred F. (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed. ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter H. ISBN 0323076998.
- ↑ Vale, TC; Cardoso, F (2015). "Chorea: A Journey through History.". Tremor and other hyperkinetic movements (New York, N.Y.). 5. PMC 4454991
 . PMID 26056609. doi:10.7916/D8WM1C98.
. PMID 26056609. doi:10.7916/D8WM1C98. - 1 2 "Learning About Huntington's Disease". www.genome.gov. Retrieved 19 July 2016.
- 1 2 3 4 "History of the HDF". Hereditary Disease Foundation. Retrieved 18 November 2015.
- 1 2 "Huntington's Disease Society of America – Our History". Huntington's Disease Society of America. 2008. Retrieved 17 March 2009.
- 1 2 3 4 van Duijn E, Kingma EM, van der Mast RC (2007). "Psychopathology in verified Huntington's disease gene carriers". J Neuropsychiatry Clin Neurosci. 19 (4): 441–8. PMID 18070848. doi:10.1176/appi.neuropsych.19.4.441.
- 1 2 3 4 5 6 7 8 9 10 11 12 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- 1 2 3 "Huntington Disease". genereviews bookshelf. University of Washington. 19 July 2007. Retrieved 12 March 2009.
- ↑ Hammond K, Tatum B (26 June 2010). "The Behavioral Symptoms of Huntington's Disease". Huntington's Outreach Project for Education, at Stanford. Retrieved 4 August 2014.
- 1 2 Kremer B (2002). "Clinical neurology of Huntington's disease". In Bates G, Harper P, Jones L. Huntington's Disease – Third Edition. Oxford: Oxford University Press. pp. 28–53. ISBN 0-19-851060-8.
- ↑ Wagle AC, Wagle SA, Marková IS, Berrios GE (2000). "Psychiatric Morbidity in Huntington's disease". Neurology, Psychiatry and Brain Research (8): 5–16.
- 1 2 3 4 5 6 7 8 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [219]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- 1 2 3 4 5 6 7 8 Montoya A, Price BH, Menear M, Lepage M (2006). "Brain imaging and cognitive dysfunctions in Huntington's disease" (PDF). J Psychiatry Neurosci. 31 (1): 21–9. PMC 1325063
 . PMID 16496032. Retrieved 1 April 2009.
. PMID 16496032. Retrieved 1 April 2009. - ↑ Aziz NA, van der Marck MA, Pijl H, Olde Rikkert MG, Bloem BR, Roos RA (2008). "Weight loss in neurodegenerative disorders". J. Neurol. 255 (12): 1872–80. PMID 19165531. doi:10.1007/s00415-009-0062-8.
- ↑ "Booklet by the Huntington Society of Canada" (PDF). Caregiver's Handbook for Advanced-Stage Huntington Disease. HD Society of Canada. 11 April 2007. Retrieved 10 August 2008.
- ↑ Gagnon JF, Petit D, Latreille V, Montplaisir J (2008). "Neurobiology of sleep disturbances in neurodegenerative disorders". Curr. Pharm. Des. 14 (32): 3430–45. PMID 19075719. doi:10.2174/138161208786549353.
- ↑ Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J. Bradley's neurology in clinical practice (6th ed.). Philadelphia, PA: Elsevier/Saunders. p. 108. ISBN 1-4377-0434-4.
- ↑ van der Burg JM, Björkqvist M, Brundin P (2009). "Beyond the brain: widespread pathology in Huntington's disease". Lancet Neurol. 8 (8): 765–74. PMID 19608102. doi:10.1016/S1474-4422(09)70178-4.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [221]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [220]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- ↑ Katsuno M, Banno H, Suzuki K, et al. (2008). "Molecular genetics and biomarkers of polyglutamine diseases". Curr. Mol. Med. 8 (3): 221–34. PMID 18473821. doi:10.2174/156652408784221298.
- 1 2 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [222]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- ↑ Nance MA, Myers RH (2001). "Juvenile onset Huntington's disease—clinical and research perspectives". Ment Retard Dev Disabil Res Rev. 7 (3): 153–7. PMID 11553930. doi:10.1002/mrdd.1022.
- ↑ Passarge E (2001). Color Atlas of Genetics (2nd ed.). Thieme. p. 142. ISBN 0-86577-958-9.
- ↑ Ridley RM, Frith CD, Crow TJ, Conneally PM (1988). "Anticipation in Huntington's disease is inherited through the male line but may originate in the female". Journal of Medical Genetics. 25 (9): 589–595. PMC 1051535
 . PMID 2972838. doi:10.1136/jmg.25.9.589.
. PMID 2972838. doi:10.1136/jmg.25.9.589. - ↑ Semaka A, Creighton S, Warby S, Hayden MR (2006). "Predictive testing for Huntington disease: interpretation and significance of intermediate alleles". Clin. Genet. 70 (4): 283–94. PMID 16965319. doi:10.1111/j.1399-0004.2006.00668.x.
- ↑ Wexler NS, Young AB, Tanzi RE, Travers H, Starosta-Rubinstein S, Penney JB, Snodgrass SR, Shoulson I, Gomez F, Ramos Arroyo MA (1987). "Homozygotes for Huntington's disease". Nature. 326 (6109): 194–197. PMID 2881213. doi:10.1038/326194a0.
- ↑ Squitieri F, Gellera C, Cannella M, et al. (2003). "Homozygosity for CAG mutation in Huntington disease is associated with a more severe clinical course". Brain. 126 (Pt 4): 946–55. PMID 12615650. doi:10.1093/brain/awg077.
- ↑ Goehler H, Lalowski M, Stelzl U, et al. (2004). "A protein interaction network links GIT1, an enhancer of Huntingtin aggregation, to Huntington's disease". Mol. Cell. 15 (6): 853–65. PMID 15383276. doi:10.1016/j.molcel.2004.09.016.
- ↑ Glajch, KE; Sadri-Vakili, G (2015). "Epigenetic Mechanisms Involved in Huntington's Disease Pathogenesis.". Journal of Huntington's disease. 4 (1): 1–15. PMID 25813218. doi:10.3233/JHD-159001.
- ↑ Harjes P, Wanker EE (2003). "The hunt for huntingtin function: interaction partners tell many different stories". Trends Biochem. Sci. 28 (8): 425–33. PMID 12932731. doi:10.1016/S0968-0004(03)00168-3. Retrieved 27 April 2009.
- 1 2 3 Cattaneo E, Zuccato C, Tartari M (2005). "Normal huntingtin function: an alternative approach to Huntington's disease". Nat. Rev. Neurosci. 6 (12): 919–30. PMID 16288298. doi:10.1038/nrn1806.
- 1 2 3 4 5 Rubinsztein DC, Carmichael J (2003). "Huntington's disease: Molecular basis of neurodegeneration". Expert Rev Mol Med. 5 (20): 1–21. PMID 14585171. doi:10.1017/S1462399403006549.
- 1 2 Bloch M, Hayden MR (1990). "Opinion: predictive testing for Huntington disease in childhood: challenges and implications". Am. J. Hum. Genet. 46 (1): 1–4. PMC 1683548
 . PMID 2136787.
. PMID 2136787. - 1 2 3 4 Bates, Gillian P.; Dorsey, Ray; Gusella, James F.; Hayden, Michael R.; Kay, Chris; Leavitt, Blair R.; Nance, Martha; Ross, Christopher A.; Scahill, Rachael I.; Wetzel, Ronald; Wild, Edward J.; Tabrizi, Sarah J. (23 April 2015). "Huntington disease". Nature Reviews Disease Primers: 15005. doi:10.1038/nrdp.2015.5.
- 1 2 3 Sadri-Vakili G, Cha JH (2006). "Mechanisms of Disease: histone modifications in Huntington's disease". Nature Clinical Practice Neurology. 2 (6): 330–338. PMID 16932577. doi:10.1038/ncpneuro0199.
- ↑ Purves D, Augustine GA, Fitzpatrick D, Hall W, LaMantia AS, McNamara JO, Williams SM (2001). "Modulation of Movement by the Basal Ganglia – Circuits within the Basal Ganglia System". In Purves D. Neuroscience (2nd ed.). Sunderland, MA: Sinauer Associates. ISBN 0-87893-742-0. Retrieved 1 April 2009.
- ↑ Lobsiger CS, Cleveland DW (2007). "Glial cells as intrinsic components of non-cell autonomous neurodegenerative disease". Nat. Neurosci. 10 (11): 1355–60. PMC 3110080
 . PMID 17965655. doi:10.1038/nn1988.
. PMID 17965655. doi:10.1038/nn1988. - 1 2 Crossman AR (2000). "Functional anatomy of movement disorders" (PDF). J. Anat. 196 (4): 519–25. PMC 1468094
 . PMID 10923984. doi:10.1046/j.1469-7580.2000.19640519.x.
. PMID 10923984. doi:10.1046/j.1469-7580.2000.19640519.x. - ↑ Duffy, Joseph (2013). Motor Speech Disorders: Substrates, Differential Diagnosis, and Management, 3rd Ed. St. Louis, Missouri: Elsevier. pp. 196–7.
- 1 2 "Analysis of Strand Slippage in DNA Polymerase Expansions of CAG/CTG Triplet Repeats Associated with Neurodegenerative Disease – JBC".
- ↑ Steffan J, Bodai L, Pallos J, et al. (18 October 2001). "Histone deacetylase inhibitors arrest polyglutamine-dependent neurodegeneration in Drosophila". Nature. 413: 739–743. PMID 11607033. doi:10.1038/35099568.
- ↑ Gaillard F (1 May 2007). "Huntington's disease". Radiology picture of the day. www.radpod.org. Retrieved 24 July 2009.
- ↑ Rao AK, Muratori L, Louis ED, Moskowitz CB, Marder KS (2009). "Clinical measurement of mobility and balance impairments in Huntington's disease: validity and responsiveness". Gait & Posture. 29 (3): 433–6. PMID 19111470. doi:10.1016/j.gaitpost.2008.11.002. Retrieved 14 April 2009.
- ↑ "Unified Huntington's Disease Rating Scale (UHDRS)". UHDRS and Database. HSG. 1 February 2009. Retrieved 14 April 2009.
- ↑ Myers RH (2004). "Huntington's Disease Genetics". NeuroRx. 1 (2): 255–62. PMC 534940
 . PMID 15717026. doi:10.1602/neurorx.1.2.255.
. PMID 15717026. doi:10.1602/neurorx.1.2.255. - 1 2 3 4 5 6 7 de Die-Smulders CE, de Wert GM, Liebaers I, Tibben A, Evers-Kiebooms G (2013). "Reproductive options for prospective parents in families with Huntington's disease: Clinical, psychological and ethical reflections". Human Reproduction Update. 19 (3): 304–315. PMID 23377865. doi:10.1093/humupd/dms058.
- ↑ Forrest Keenan K, Simpson SA, Miedzybrodzka Z, Alexander DA, Semper J (2013). "How do partners find out about the risk of Huntington's disease in couple relationships?". Journal of Genetic Counseling. 22 (3): 336–44. PMID 23297124. doi:10.1007/s10897-012-9562-2.
- ↑ Erwin C, Williams JK, Juhl AR, Mengeling M, Mills JA, Bombard Y, Hayden MR, Quaid K, Shoulson I, Taylor S, Paulsen JS (2010). "Perception, experience, and response to genetic discrimination in Huntington disease: the international RESPOND-HD study". American Journal of Medical Genetics Part B. 153B (5): 1081–93. PMC 3593716
 . PMID 20468061. doi:10.1002/ajmg.b.31079.
. PMID 20468061. doi:10.1002/ajmg.b.31079. - ↑ Burson CM, Markey KR (2001). "Genetic counseling issues in predictive genetic testing for familial adult-onset neurologic diseases". Semin Pediatr Neurol. 8 (3): 177–86. PMID 11575847. doi:10.1053/spen.2001.26451.
- ↑ Smith JA, Michie S, Stephenson M, Quarrell O (2002). "Risk Perception and Decision-making Processes in Candidates for Genetic Testing for Huntington's Disease: An Interpretative Phenomenological Analysis". Journal of Health Psychology. 7 (2): 131–44. PMID 22114233. doi:10.1177/1359105302007002398.
- 1 2 Hayden MR (March 2003). "Predictive testing for Huntington's disease: a universal model?". Lancet Neurol. 2 (3): 141–2. PMID 12849232. doi:10.1016/S1474-4422(03)00317-X.
- ↑ "Guidelines for the molecular genetics predictive test in Huntington's disease. International Huntington Association (IHA) and the World Federation of Neurology (WFN) Research Group on Huntington's Chorea". Neurology. 44 (8): 1533–6. 1994. PMID 8058167. doi:10.1212/WNL.44.8.1533.
- ↑ Losekoot M, van Belzen MJ, Seneca S, Bauer P, Stenhouse SA, Barton DE (2012). "EMQN/CMGS best practice guidelines for the molecular genetic testing of Huntington disease". Eur J Hum Genet. 21 (5): 480–6. PMC 3641377
 . PMID 22990145. doi:10.1038/ejhg.2012.200.
. PMID 22990145. doi:10.1038/ejhg.2012.200. - ↑ Schulman JD, Black SH, Handyside A, Nance WE (1996). "Preimplantation genetic testing for Huntington disease and certain other dominantly inherited disorders". Clinical Genetics. 49 (2): 57–58. PMID 8740912. doi:10.1111/j.1399-0004.1996.tb04327.x.
- ↑ Stern HJ, Harton GL, Sisson ME, Jones SL, Fallon LA, Thorsell LP, Getlinger ME, Black SH, Schulman JD (2002). "Non-disclosing preimplantation genetic diagnosis for Huntington disease". Prenatal Diagnosis. 22 (6): 503–507. PMID 12116316. doi:10.1002/pd.359.
- ↑ "Predictive Testing for Huntington's Disease". 2011. Retrieved 7 May 2013.
- ↑ Kuliev A, Verlinsky Y (2005). "Preimplantation diagnosis: A realistic option for assisted reproduction and genetic practice". Curr. Opin. Obstet. Gynecol. 17 (2): 179–83. PMID 15758612. doi:10.1097/01.gco.0000162189.76349.c5.
- ↑ "Guidelines for Genetic Testing for Huntington's Disease". Heredity Disease Foundation. Retrieved 7 May 2013.
- 1 2 Schneider SA, Walker RH, Bhatia KP (2007). "The Huntington's disease-like syndromes: what to consider in patients with a negative Huntington's disease gene test". Nat Clin Pract Neurol. 3 (9): 517–25. PMID 17805246. doi:10.1038/ncpneuro0606.
- ↑ Frank S, Jankovic J (2010). "Advances in the Pharmacological Management of Huntington's Disease". Drugs. 70 (5): 561–71. PMID 20329804. doi:10.2165/11534430-000000000-00000.
- 1 2 3 4 5 6 Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [224]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- 1 2 3 Bonelli RM, Wenning GK, Kapfhammer HP (2004). "Huntington's disease: present treatments and future therapeutic modalities". Int Clin Psychopharmacol. 19 (2): 51–62. PMID 15076012. doi:10.1097/00004850-200403000-00001. Retrieved 1 April 2009.
- ↑ Lee, CF; Chern, Y (2014). "Adenosine receptors and Huntington's disease". International review of neurobiology. 119: 195–232. PMID 25175968. doi:10.1016/B978-0-12-801022-8.00010-6.
- ↑ Simonin, C; Duru, C; Salleron, J; Hincker, P; Charles, P; Delval, A; Youssov, K; Burnouf, S; Azulay, JP; Verny, C; Scherer, C; Tranchant, C; Goizet, C; Debruxelles, S; Defebvre, L; Sablonnière, B; Romon-Rousseaux, M; Buée, L; Destée, A; Godefroy, O; Dürr, A; Landwehrmeyer, B; REGISTRY Study of the European Huntington's Disease, Network; Bachoud-Levi, AC; Richard, F; Blum, D; Krystkowiak, P; Huntington French Speaking, Network (October 2013). "Association between caffeine intake and age at onset in Huntington's disease". Neurobiology of disease. 58: 179–82. PMID 23732677. doi:10.1016/j.nbd.2013.05.013.
- ↑ "EBM: Levels of Evidence". Essential Evidence Plus. Retrieved 2012-02-23.
- ↑ Panagiotakis PH, DiSario JA, Hilden K, Ogara M, Fang JC (2008). "DPEJ tube placement prevents aspiration pneumonia in high-risk patients". Nutr Clin Pract. 23 (2): 172–5. PMID 18390785. doi:10.1177/0884533608314537.
- 1 2 "EHDN Physiotherapy Guidance Document" (PDF). European HD Network Physiotherapy Working Group. Retrieved 2015-11-15.
- ↑ Quin L, Busee M (February 2012). "Development of physiotherapy guidance and treatment-based classifications for people with Huntington's disease". Neurodegenerative Disease Management. 2 (1): 21–31. doi:10.2217/nmt.11.86.
- ↑ Khalil H, Quinn L, van Deursen R, Martin R, Rosser A, Busse M (January 2012). "Adherence to use of a home-based exercise DVD in people with Huntington disease: participants' perspectives". Physical Therapy. 92 (1): 69–82. PMID 21960468. doi:10.2522/ptj.20100438.
- ↑ Travers E, Jones K, Nicol J (2007). "Palliative care provision in Huntington's disease". International journal of palliative nursing. 13 (3).
- ↑ "FDA Approves First Drug for Treatment of Chorea in Huntington's Disease". FDA Approves First Drug for Treatment of Chorea in Huntington's Disease. U.S. Food and Drug Administration. 15 August 2008. Retrieved 10 August 2008.
- ↑ Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [225]. PMID 17240289. doi:10.1016/S0140-6736(07)60111-1.
- ↑ Harper P (2002). "Genetic counselling and presymptomatic testing". In Bates G, Harper P, Jones L. Huntington's Disease – Third Edition. Oxford: Oxford University Press. pp. 198–242. ISBN 0-19-851060-8.
- ↑ Harper PS (1999). "Huntington's disease: a clinical, genetic and molecular model for polyglutamine repeat disorders". Philos. Trans. R. Soc. Lond., B, Biol. Sci. 354 (1386): 957–61. PMC 1692597
 . PMID 10434293. doi:10.1098/rstb.1999.0446.
. PMID 10434293. doi:10.1098/rstb.1999.0446. - ↑ Andrew SE, Goldberg YP, Kremer B, Telenius H, Theilmann J, Adam S, Starr E, Squitieri F, Lin B, Kalchman MA (1993). "The relationship between trinucleotide (CAG) repeat length and clinical features of Huntington's disease". Nat. Genet. 4 (4): 398–403. PMID 8401589. doi:10.1038/ng0893-398.
- ↑ Crauford D, Snowden J (2002). "Neuropyschological and neuropsychiatric aspects of Huntington's disease". In Bates G, Harper P, Jones L. Huntington's Disease – Third Edition. Oxford: Oxford University Press. pp. 62–87. ISBN 0-19-851060-8.
- ↑ Di Maio L, Squitieri F, Napolitano G, Campanella G, Trofatter JA, Conneally PM (1993). "Suicide risk in Huntington's disease". J. Med. Genet. 30 (4): 293–5. PMC 1016335
 . PMID 8487273. doi:10.1136/jmg.30.4.293.
. PMID 8487273. doi:10.1136/jmg.30.4.293. - 1 2 3 4 5 6 Harper P (2002). "The epidemiology of Huntington's disease". In Bates G, Harper P, Jones L. Huntington's Disease – Third Edition. Oxford: Oxford University Press. pp. 159–189. ISBN 0-19-851060-8.
- ↑ Sharon I; Sharon R; Wilkens JP; Ersan T (2010). "Huntington Disease Dementia". emedicine, WebMD. Medscape. Retrieved 16 May 2010.
- ↑ Driver-Dunckley E, Caviness JN (2007). "Huntington's disease". In Schapira AHV. Neurology and Clinical Neuroscience. Mosby Elsevier. pp. 879–885. ISBN 978-0-323-03354-1.
- ↑ Evans SJ, Douglas I, Rawlins MD, Wexler NS, Tabrizi SJ, Smeeth L (2013). "Prevalence of adult Huntington's disease in the UK based on diagnoses recorded in general practice records". Journal of Neurology, Neurosurgery, and Psychiatry. 84 (10): 1156–60. PMC 3786631
 . PMID 23482661. doi:10.1136/jnnp-2012-304636.
. PMID 23482661. doi:10.1136/jnnp-2012-304636. - ↑ Avila-Giróo R (1973). "Medical and Social Aspects of Huntington's chorea in the state of Zulia, Venezuela". Advances in Neurology. 1: 261–6. ISSN 0091-3952. NAID 10021247802.
- 1 2 Gusella JF, Wexler NS, Conneally PM, Naylor SL, Anderson MA, Tanzi RE, Watkins PC, Ottina K, Wallace MR, Sakaguchi AY (1983). "A polymorphic DNA marker genetically linked to Huntington's disease". Nature. 306 (5940): 234–8. PMID 6316146. doi:10.1038/306234a0.
- ↑ Squitieri F, Andrew SE, Goldberg YP, et al. (1994). "DNA haplotype analysis of Huntington disease reveals clues to the origins and mechanisms of CAG expansion and reasons for geographic variations of prevalence". Hum. Mol. Genet. 3 (12): 2103–14. PMID 7881406. doi:10.1093/hmg/3.12.2103.
- ↑ Sveinsson, Ó (July 2012). "An Unusually Low Prevalence of Huntington's Disease in Iceland". European Neurology. 68: 48–51. PMID 22722209. doi:10.1159/000337680.
- ↑ Sipilä, Jussi O. T.; Hietala, Marja; Siitonen, Ari; Päivärinta, Markku; Majamaa, Kari (Jan 2015). "Epidemiology of Huntington's disease in Finland". Parkinsonism & Related Disorders. 21 (1): 46–49. ISSN 1873-5126. PMID 25466405. doi:10.1016/j.parkreldis.2014.10.025.
- ↑ Almqvist EW, Elterman DS, MacLeod PM, Hayden MR (2001). "High incidence rate and absent family histories in one quarter of patients newly diagnosed with Huntington disease in British Columbia". Clin. Genet. 60 (3): 198–205. PMID 11595021. doi:10.1034/j.1399-0004.2001.600305.x.
- 1 2 Huntington G (1872). "On Chorea". Medical and Surgical Reporter of Philadelphia. The Hague: Nijhoff. 26 (15): 317–321. ISBN 90-6186-011-3. Retrieved 1 April 2009.
- ↑ Karen Bellenir, ed. (2004). "Huntington Disease". Genetic Disorders Sourcebook (3rd ed.). Detroit: Omnigraphics. pp. 159–179. ISBN 0-7808-0742-1.
- 1 2 3 4 5 6 7 8 9 10 Harper P (2002). "Huntington's disease: a historical background". In Bates G, Harper P, Jones L. Huntington's Disease – Third Edition. Oxford: Oxford University Press. pp. 3–24. ISBN 0-19-851060-8.
- 1 2 3 4 Wexler A, Wexler N (2008). The Woman Who Walked Into the Sea. Huntington's and the Making of a Genetic Disease. Yale University Press. p. 288. ISBN 978-0-300-10502-5. Retrieved 2015-11-15.
- ↑ Lund JC (1860). "Chorea Sti Viti i Sætersdalen. Uddrag af Distriktslæge J. C. Lunds Medicinalberetning for 1860". Beretning om Sundhedstilstanden. Norway: 137–138.
- ↑ Lanska DJ (2000). "George Huntington (1850–1916) and hereditary chorea". J Hist Neurosci. 9 (1): 76–89. PMID 11232352. doi:10.1076/0964-704X(200004)9:1;1-2;FT076.
- ↑ Brody IA, Wilkins RH (1967). "Huntington's Chorea". Arch Neurol. 17 (3): 331. PMID 4228262. doi:10.1001/archneur.1967.00470270109013.
- ↑ Jelliffe SE, Muncey EB, Davenport CB (1913). "Huntington's Chorea: A Study in Heredity". The Journal of Nervous and Mental Disease. 40 (12): 796–799. doi:10.1097/00005053-191312000-00010.
- 1 2 Davenport CB, Muncey EB (1916). "Huntington's chorea in relation to heredity and eugenics". American Journal of Insanity. 73 (2): 195–222. doi:10.1176/appi.ajp.73.2.195.
- ↑ Vessie PR (1932). "On the transmission of Huntington's chorea for 300 years – the Bures family group". Nervous and Mental Disease. Baltimore. 76 (6): 553–573. doi:10.1097/00005053-193212000-00001. Retrieved 1 April 2009.
- 1 2 Wexler AR (2002). "Chorea and community in a 19th-century town". Bull Hist Med. 76 (3): 495–527. PMID 12486915. doi:10.1353/bhm.2002.0150.
- ↑ Conneally PM (1984). "Huntington disease: genetics and epidemiology". Am. J. Hum. Genet. 36 (3): 506–26. PMC 1684448
 . PMID 6233902.
. PMID 6233902. - ↑ Wexler NS (2012). "Huntington's Disease: Advocacy driving science". Annu Rev Med. 63: 1–22. doi:10.1146/annurev-med-050710-134457.
- ↑ "The Venezuela Huntington's disease project". Hereditary Disease Foundation website. Hereditary Disease Foundation. 2008. Retrieved 8 September 2008.
- 1 2 Macdonald M (1993). "A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. The Huntington's Disease Collaborative Research Group". Cell. 72 (6): 971–83. PMID 8458085. doi:10.1016/0092-8674(93)90585-E.
- ↑ Bertram L, Tanzi RE (2005). "The genetic epidemiology of neurodegenerative disease". J. Clin. Invest. 115 (6): 1449–57. PMC 1137006
 . PMID 15931380. doi:10.1172/JCI24761.
. PMID 15931380. doi:10.1172/JCI24761. - ↑ La Spada AR, Roling DB, Harding AE, et al. (1992). "Meiotic stability and genotype-phenotype correlation of the trinucleotide repeat in X-linked spinal and bulbar muscular atrophy". Nat. Genet. 2 (4): 301–4. PMID 1303283. doi:10.1038/ng1292-301.
- 1 2 3 Ross CA, Tabrizi SJ (January 2011). "Huntington's disease: from molecular pathogenesis to clinical treatment". Lancet Neurology. 10 (1): 83–98. PMID 21163446. doi:10.1016/S1474-4422(10)70245-3.
- ↑ "What is HD?". Huntington's disease association. Retrieved 18 December 2011.
- ↑ Davenport CB (1915). "Huntington's Chorea in Relation to Heredity and Eugenics". Proc. Natl. Acad. Sci. U.S.A. 1 (5): 283–5. PMC 1090803
 . PMID 16575999. doi:10.1073/pnas.1.5.283.
. PMID 16575999. doi:10.1073/pnas.1.5.283. - ↑ Rollin BE (2006). "The Regulation of Animal Research and the Emergence of Animal Ethics: A Conceptual History". Theoretical Medicine and Bioethics. 27 (4): 285–304. PMID 16937023. doi:10.1007/s11017-006-9007-8.
- ↑ Doerflinger RM (2008). "The problem of deception in embryonic stem cell research". Cell Prolif. 41 Suppl 1: 65–70. PMID 18181947. doi:10.1111/j.1365-2184.2008.00492.x.
- ↑ Chapman MA (1990). "Predictive testing for adult-onset genetic disease: ethical and legal implications of the use of linkage analysis for Huntington disease". Am. J. Hum. Genet. 47 (1): 1–3. PMC 1683745
 . PMID 2140926.
. PMID 2140926. - ↑ Huggins M, Bloch M, Kanani S, et al. (1990). "Ethical and legal dilemmas arising during predictive testing for adult-onset disease: the experience of Huntington disease". Am. J. Hum. Genet. 47 (1): 4–12. PMC 1683755
 . PMID 1971997.
. PMID 1971997. - ↑ "Insurance Genetics Moratorium extended to 2017" (Press release). Association of British Insurers. 5 April 2011. Retrieved 13 January 2016.
- ↑ "Expert backs gene test disclosure". BBC article. 7 June 2007.
- ↑ Binedell J, Soldan JR, Scourfield J, Harper PS (1996). "Huntington's disease predictive testing: the case for an assessment approach to requests from adolescents". J. Med. Genet. 33 (11): 912–8. PMC 1050784
 . PMID 8950670. doi:10.1136/jmg.33.11.912.
. PMID 8950670. doi:10.1136/jmg.33.11.912. - ↑ Borry P, Goffin T, Nys H, Dierickx K (2008). "Predictive genetic testing in minors for adult-onset genetic diseases". Mt. Sinai J. Med. 75 (3): 287–96. PMID 18704981. doi:10.1002/msj.20038.
- 1 2 3 Braude PR, De Wert GM, Evers-Kiebooms G, Pettigrew RA, Geraedts JP (1998). "Non-disclosure preimplantation genetic diagnosis for Huntington's disease: practical and ethical dilemmas". Prenat. Diagn. 18 (13): 1422–6. PMID 9949442. doi:10.1002/(SICI)1097-0223(199812)18:13<1422::AID-PD499>3.0.CO;2-R.
- ↑ "The International Huntington Association". International Huntington Association. 2013. Retrieved 3 April 2009.
- ↑ "US Senate s. resolution 531". S. Res. 531. US Senate. 6 April 2008. Retrieved 10 August 2008.
- 1 2 Odling-Smee L (17 May 2007). "Biomedical philanthropy: The money tree". Nature. 447 (7142): 251–251. doi:10.1038/447251a.
- ↑ "CHDI Foundation, Inc". Retrieved 4 December 2011.
- ↑ Check E (17 May 2007). "Biomedical philanthropy: Love or money". Nature. 447 (7142): 252–253. PMID 17507955. doi:10.1038/447252a.
- ↑ Turner C, Schapira AH (2010). "Mitochondrial matters of the brain: the role in Huntington's disease". Journal of bioenergetics and biomembranes. 42 (3): 193–8. PMID 20480217. doi:10.1007/s10863-010-9290-y.
- ↑ Wild, EJ; Tabrizi, SJ (15 September 2014). "Targets for future clinical trials in Huntington's disease: what's in the pipeline?". Movement disorders : official journal of the Movement Disorder Society. 29 (11): 1434–45. PMC 4265300
 . PMID 25155142. doi:10.1002/mds.26007.
. PMID 25155142. doi:10.1002/mds.26007. - 1 2 Solomon, Shoshanna (3 May 2017). "Taube to fund $3m Huntington’s disease research in US". The Times of Israel. Retrieved 5 May 2017.
- 1 2 Munoz-Sanjuan, I; Bates, GP (2011). "The importance of integrating basic and clinical research toward the development of new therapies for Huntington disease". Journal of Clinical Investigation. 121 (2): 476–483. PMC 3026740
 . PMID 21285520. doi:10.1172/JCI45364.
. PMID 21285520. doi:10.1172/JCI45364. - ↑ McBride, Jodi L; Pitzer, Mark R; Boudreau, Ryan L; Dufour, Brett; Hobbs, Theodore; Ojeda, Sergio R; Davidson, Beverly L (25 October 2011). "Preclinical Safety of RNAi-Mediated HTT Suppression in the Rhesus Macaque as a Potential Therapy for Huntington's Disease". Molecular Therapy. 19 (12): 2152–2162. PMC 3242667
 . PMID 22031240. doi:10.1038/mt.2011.219.
. PMID 22031240. doi:10.1038/mt.2011.219. - ↑ Kordasiewicz, Holly B.; Stanek, Lisa M.; Wancewicz, Edward V.; Mazur, Curt; McAlonis, Melissa M.; Pytel, Kimberly A.; Artates, Jonathan W.; Weiss, Andreas; Seng H. Cheng; Shihabuddin, Lamya S.; Hung, Gene; Bennett, C. Frank; Cleveland, Don W. (21 June 2012). "Sustained Therapeutic Reversal of Huntington's Disease by Transient Repression of Huntingtin Synthesis". Neuron. 74 (6): 1031–1044. PMC 3383626
 . PMID 22726834. doi:10.1016/j.neuron.2012.05.009.
. PMID 22726834. doi:10.1016/j.neuron.2012.05.009. - ↑ Barnes, DW; Whitley, RJ (Feb 1987). "Antiviral therapy and pulmonary disease". Chest. 91 (2): 246–51. PMID 3026739. doi:10.1172/JCI45130.
- ↑ "Landmark Huntington's trial starts". Retrieved 19 October 2015.
- ↑ "Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of IONIS-HTTRx in Patients With Early Manifest Huntington's Disease - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. Retrieved 18 April 2016.
- ↑ Wild, EJ; Boggio, R; Langbehn, D; Robertson, N; Haider, S; Miller, JR; Zetterberg, H; Leavitt, BR; Kuhn, R; Tabrizi, SJ; Macdonald, D; Weiss, A (May 2015). "Quantification of mutant huntingtin protein in cerebrospinal fluid from Huntington's disease patients.". The Journal of Clinical Investigation. 125 (5): 1979–86. PMC 4463213
 . PMID 25844897. doi:10.1172/jci80743.
. PMID 25844897. doi:10.1172/jci80743. - ↑ Chase, Alex (21 April 2015). "Huntington disease: Cerebrospinal fluid and MRI biomarkers for prodromal HD". Nature Reviews Neurology. 11 (5): 245–245. doi:10.1038/nrneurol.2015.63.
- ↑ Keiser, Megan S.; Kordasiewicz, Holly B.; McBride, Jodi L. (15 April 2016). "Gene suppression strategies for dominantly inherited neurodegenerative diseases: lessons from Huntington's disease and spinocerebellar ataxia". Human Molecular Genetics. 25 (R1): R53–R64. PMC 4802374
 . PMID 26503961. doi:10.1093/hmg/ddv442.
. PMID 26503961. doi:10.1093/hmg/ddv442. - ↑ Clelland CD, Barker RA, Watts C (2008). "Cell therapy in Huntington disease". Neurosurg Focus. 24 (3–4): E9. PMID 18341412. doi:10.3171/FOC/2008/24/3-4/E8.
- ↑ Cundiff PE, Anderson SA (31 May 2011). "Impact of induced pluripotent stem cells on the study of central nervous system disease". Current Opinion in Genetics & Development. 21 (3): 354–361. PMID 21277194. doi:10.1016/j.gde.2011.01.008.
- ↑ Wild, EJ; Tabrizi, SJ (15 September 2014). "Targets for future clinical trials in Huntington's disease: what's in the pipeline?". Movement disorders : official journal of the Movement Disorder Society. 29 (11): 1434–45. PMC 4265300
 . PMID 25155142. doi:10.1002/mds.26007.
. PMID 25155142. doi:10.1002/mds.26007. - ↑ "Completed Clinical Trials". Huntington Study Group. Archived from the original on 28 June 2012. Retrieved 4 February 2012.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
- Huntington's disease at DMOZ
 Works related to On Chorea at Wikisource
Works related to On Chorea at Wikisource- HOPES project – Stanford University's HD information project
- HDBuzz – HD research news written by scientists in plain language
- HD Drug Works – news about current treatments and planned trials