Heart
| Heart | |
|---|---|
 The human heart | |
| Details | |
| System | Circulatory |
| Artery | Aorta,[lower-alpha 1] pulmonary trunk and right and left pulmonary arteries[lower-alpha 2] Right coronary artery, left main coronary artery[lower-alpha 3] |
| Vein | Superior vena cava, inferior vena cava,[lower-alpha 4] right and left pulmonary veins,[lower-alpha 5] great cardiac vein, middle cardiac vein, small cardiac vein, anterior cardiac veins.[lower-alpha 6] |
| Nerve | Accelerans nerve, vagus nerve |
| Identifiers | |
| Latin | cor |
| Greek | kardía (καρδία) |
| MeSH | A07.541 |
| TA | A12.1.00.001 |
| FMA | 7088 |
 |
|
| Problems playing this file? See media help. | |
The heart is a muscular organ in humans and other animals, which pumps blood through the blood vessels of the circulatory system.[1] Blood provides the body with oxygen and nutrients, as well as assists in the removal of metabolic wastes.[2] In humans, the heart is located between the lungs, in the middle compartment of the chest.[3]
In humans, other mammals, and birds, the heart is divided into four chambers: upper left and right atria; and lower left and right ventricles.[4][5] Commonly the right atrium and ventricle are referred together as the right heart and their left counterparts as the left heart.[6] Fish, in contrast, have two chambers, an atrium and a ventricle, while reptiles have three chambers.[5] In a healthy heart blood flows one way through the heart due to heart valves, which prevent backflow.[3] The heart is enclosed in a protective sac, the pericardium, which also contains a small amount of fluid. The wall of the heart is made up of three layers: epicardium, myocardium, and endocardium.[7]
The heart pumps blood with a rhythm determined by a group of pacemaking cells in the sinoatrial node. These generate a current that causes contraction of the heart, traveling through the atrioventricular node and along the conduction system of the heart. The heart receives blood low in oxygen from the systemic circulation, which enters the right atrium from the superior and inferior venae cavae and passes to the right ventricle. From here it is pumped into the pulmonary circulation, through the lungs where it receives oxygen and gives off carbon dioxide. Oxygenated blood then returns to the left atrium, passes through the left ventricle and is pumped out through the aorta to the systemic circulation−where the oxygen is used and metabolized to carbon dioxide.[8] The heart beats at a resting rate close to 72 beats per minute.[9] Exercise temporarily increases the rate, but lowers resting heart rate in the long term, and is good for heart health.[10]
Cardiovascular diseases (CVD) are the most common cause of death globally as of 2008, accounting for 30% of deaths.[11][12] Of these more than three quarters are a result of coronary artery disease and stroke.[11] Risk factors include: smoking, being overweight, little exercise, high cholesterol, high blood pressure, and poorly controlled diabetes, among others.[13] Cardiovascular diseases frequently have no symptoms or may cause chest pain or shortness of breath. Diagnosis of heart disease is often done by the taking of a medical history, listening to the heart-sounds with a stethoscope, ECG, and ultrasound.[3] Specialists who focus on diseases of the heart are called cardiologists, although many specialties of medicine may be involved in treatment.[12]
Structure


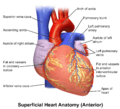
Location and shape
The human heart is situated in the middle mediastinum, at the level of thoracic vertebrae T5-T8. A double-membraned sac called the pericardium surrounds the heart and attaches to the mediastinum.[15] The back surface of the heart lies near the vertebral column, and the front surface sits behind the sternum and rib cartilages.[7] The upper part of the heart is the attachment point for several large blood vessels – the venae cavae, aorta and pulmonary trunk. The upper part of the heart is located at the level of the third costal cartilage.[7] The lower tip of the heart, the apex, lies to the left of the sternum (8 to 9 cm from the midsternal line) between the junction of the fourth and fifth ribs near their articulation with the costal cartilages.[7]
The largest part of the heart is usually slightly offset to the left side of the chest (though occasionally it may be offset to the right) and is felt to be on the left because the left heart is stronger and larger, since it pumps to all body parts. Because the heart is between the lungs, the left lung is smaller than the right lung and has a cardiac notch in its border to accommodate the heart.[7] The heart is cone-shaped, with its base positioned upwards and tapering down to the apex.[7] An adult heart has a mass of 250–350 grams (9–12 oz).[16] The heart is typically the size of a fist: 12 cm (5 in) in length, 8 cm (3.5 in) wide, and 6 cm (2.5 in) in thickness.[7] Well-trained athletes can have much larger hearts due to the effects of exercise on the heart muscle, similar to the response of skeletal muscle.[7]
Chambers
The heart has four chambers, two upper atria, the receiving chambers, and two lower ventricles, the discharging chambers. The atria open into the ventricles via the atrioventricular valves, present in the atrioventricular septum. This distinction is visible also on the surface of the heart as the coronary sulcus.[17] There is an ear-shaped structure in the upper right atrium called the right atrial appendage, or auricle, and another in the upper left atrium, the left atrial appendage.[18] The right atrium and the right ventricle together are sometimes referred to as the right heart. Similarly, the left atrium and the left ventricle together are sometimes referred to as the left heart.[6] The ventricles are separated from each other by the interventricular septum, visible on the surface of the heart as the anterior longitudinal sulcus and the posterior interventricular sulcus.[17]
The cardiac skeleton is made of dense connective tissue and this gives structure to the heart. It forms the atrioventricular septum which separates the atria from the ventricles, and the fibrous rings which serve as bases for the four heart valves.[19] The cardiac skeleton also provides an important boundary in the heart's electrical conduction system since collagen cannot conduct electricity. The interatrial septum separates the atria and the interventricular septum separates the ventricles.[7] The interventricular septum is much thicker than the interatrial septum, since the ventricles need to generate greater pressure when they contract.[7]
Valves

.svg.png)

The heart has four valves, which separate its chambers. One valve lies between each atrium and ventricle, and one valve rests at the exit of each ventricle.[7]
The valves between the atria and ventricles are called the atrioventricular valves. Between the right atrium and the right ventricle is the tricuspid valve. The tricuspid valve has three cusps,[20] which connect to chordae tendinae and three papillary muscles named the anterior, posterior, and septal muscles, after their relative positions.[20] The mitral valve lies between the left atrium and left ventricle. It is also known as the bicuspid valve due to its having two cusps, an anterior and a posterior cusp. These cusps are also attached via chordae tendinae to two papillary muscles projecting from the ventricular wall.[21]
The papillary muscles extend from the walls of the heart to valves by cartilaginous connections called chordae tendinae. These muscles prevent the valves from falling too far back when they close.[22] During the relaxation phase of the cardiac cycle, the papillary muscles are also relaxed and the tension on the chordae tendineae is slight. As the heart chambers contract, so do the papillary muscles. This creates tension on the chordae tendineae, helping to hold the cusps of the atrioventricular valves in place and preventing them from being blown back into the atria.[7] [lower-alpha 7][20]
Two additional semilunar valves sit at the exit of each of the ventricles. The pulmonary valve is located at the base of the pulmonary artery. This has three cusps which are not attached to any papillary muscles. When the ventricle relaxes blood flows back into the ventricle from the artery and this flow of blood fills the pocket-like valve, pressing against the cusps which close to seal the valve. The semilunar aortic valve is at the base of the aorta and also is not attached to papillary muscles. This too has three cusps which close with the pressure of the blood flowing back from the aorta.[7]
Right heart
The right heart consists of two chambers, the right atrium and the right ventricle, separated by a valve, the tricuspid valve.[7]
The right atrium receives blood almost continuously from the body's two major veins, the superior and inferior venae cavae. A small amount of blood from the coronary circulation also drains into the right atrium via the coronary sinus, which is immediately above and to the middle of the opening of the inferior vena cava.[7] In the wall of the right atrium is an oval-shaped depression known as the fossa ovalis, which is a remnant of an opening in the fetal heart known as the foramen ovale.[7] Most of the internal surface of the right atrium is smooth, the depression of the fossa ovalis is medial, and the anterior surface has prominent ridges of pectinate muscles, which are also present in the right atrial appendage.[7]
The right atrium is connected to the right ventricle by the tricuspid valve.[7] The walls of the right ventricle are lined with trabeculae carneae, ridges of cardiac muscle covered by endocardium. In addition to these muscular ridges, a band of cardiac muscle, also covered by endocardium, known as the moderator band reinforces the thin walls of the right ventricle and plays a crucial role in cardiac conduction. It arises from the lower part of the interventricular septum and crosses the interior space of the right ventricle to connect with the inferior papillary muscle.[7] The right ventricle tapers into the pulmonary trunk, into which it ejects blood when contracting. The pulmonary trunk branches into the left and right pulmonary arteries that carry the blood to each lung. The pulmonary valve lies between the right heart and the pulmonary trunk.[7]
Left heart
The left heart has two chambers: the left atrium, and the left ventricle, separated by the mitral valve.[7]
The left atrium receives oxygenated blood back from the lungs via one of the four pulmonary veins. The left atrium has an outpouching called the left atrial appendage. Like the right atrium, the left atrium is lined by pectinate muscles.[23] The left atrium is connected to the left ventricle by the mitral valve.[7]
The left ventricle is much thicker as compared with the right, due to the greater force needed to pump blood to the entire body. Like the right ventricle, the left also has trabeculae carneae, but there is no moderator band. The left ventricle pumps blood to the body through the aortic valve and into the aorta. Two small openings above the aortic valve carry blood to the heart itself, the left main coronary artery and the right coronary artery.[7]
Heart wall

The heart wall is made up of three layers: the inner endocardium, middle myocardium and outer epicardium. These are surrounded by a double-membraned sac called the pericardium.
The innermost layer of the heart is called the endocardium. It is made up of a lining of simple squamous epithelium, and covers heart chambers and valves. It is continuous with the endothelium of the veins and arteries of the heart, and is joined to the myocardium with a thin layer of connective tissue.[7] The endocardium, by secreting endothelins, may also play a role in regulating the contraction of the myocardium.[7]

The middle layer of the heart wall is the myocardium, which is the cardiac muscle – a layer of involuntary striated muscle tissue surrounded by a framework of collagen. The cardiac muscle pattern is elegant and complex, as the muscle cells swirl and spiral around the chambers of the heart, with the outer muscles forming a figure 8 pattern around the atria and around the bases of the great vessels, and inner muscles formining a figure 8 around the two ventricles and proceed toward the apex. This complex swirling pattern allows the heart to pump blood more effectively.[7]
There are two types of cells in cardiac muscle: muscle cells which have the ability to contract easily, and pacemaker cells of the conducting system. The muscle cells make up the bulk (99%) of cells in the atria and ventricles. These contractile cells are connected by intercalated discs which allow a rapid response to impulses of action potential from the pacemaker cells. The intercalated discs allow the cells to act as a syncytium and enable the contractions that pump blood through the heart and into the major arteries.[7] The pacemaker cells make up 1% of cells and form the conduction system of the heart. They are generally much smaller than the contractile cells and have few myofibrils which gives them limited contractibility. Their function is similar in many respects to neurons.[7] Cardiac muscle tissue has autorhythmicity, the unique ability to initiate a cardiac action potential at a fixed rate – spreading the impulse rapidly from cell to cell to trigger the contraction of the entire heart.[7]
The pericardium surrounds the heart. It consists of two membranes: an inner serous membrane called the epicardium, and an outer fibrous membrane. Blood vessels and nerves reach the cardiac muscle from the epicardium.[7] These help influence the heart rate.[7] These enclose the pericardial cavity which contains the pericardial fluid that lubricates the surface of the heart.[24]
Coronary circulation
Heart tissue, like all cells in the body, needs to be supplied with oxygen, nutrients and a way of removing metabolic wastes. This is achieved by the coronary circulation, which includes arteries, veins, and lymphatic vessels. Blood flow through the coronary vessels occurs in peaks and troughs relating to the heart muscle's relaxation or contraction.[7]
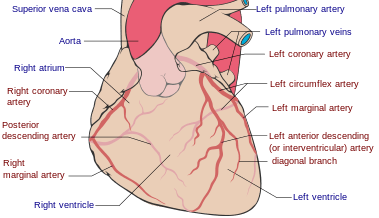
Heart tissue receives blood from two arteries which arise just above the aortic valve. These are the left main coronary artery and the right coronary artery. The left main coronary artery splits shortly after leaving the aorta into two vessels, the left anterior descending and the left circumflex artery. The left anterior descending artery supplies heart tissue and the front, outer side, and the septum of the left ventricle. It does this by branching into smaller arteries – diagonal and septal branches. The left circumflex supplies the back and underneath of the left ventricle. The right coronary artery supplies the right atrium, right ventricle, and lower posterior sections of the left ventricle. The right coronary artery also supplies blood to the atrioventricular node (in about 90% of people) and the sinoatrial node (in about 60% of people). The right coronary artery runs in a groove at the back of the heart and the left anterior descending artery runs in a groove at the front. There is significant variation between people in the anatomy of the arteries that supply the heart [25] The arteries divide at their furtherst reaches into smaller branches that join together at the edges of each arterial distribution.[7]
The coronary sinus is a large vein that drains into the right atrium, and receives most of the venous drainage of the heart. It receives blood from the great cardiac vein (receiving the left atrium and both ventricles), the posterior cardiac vein (draining the back of the left ventricle), the middle cardiac vein (draining the bottom of the left and right ventricles), and small cardiac veins.[26] The anterior cardiac veins drain the front of the right ventricle and drain directly into the right atrium.[7]
Small lymphatic networks called plexuses exist beneath each of the three layers of the heart. These networks collect into a main left and a main right trunk, which travel up the groove between the ventricles that exists on the heart's surface, receiving smaller vessels as they travel up. These vessels then travel into the atrioventricular groove, and receive a third vessel which drains the section of the left ventricle sitting on the diaphragm. The left vessel joins with this third vessel, and travels along the pulmonary artery and left atrium, ending in the inferior tracheobronchial node. The right vessel travels along the right atrium and the part of the right ventricle sitting on the diaphragm. It usually then travels in front of the ascending aorta and then ends in a brachiocephalic node.[27]
Nerve supply

The heart receives nerve signals from the vagus nerve and from nerves arising from the sympathetic trunk. These nerves act to influence, but not control, the heart rate. Sympathetic nerves also influence the force of heart contraction.[28] Signals that travel along these nerves arise from two paired cardiovascular centres in the medulla oblongata. The vagus nerve of the parasympathetic nervous system acts to decrease the heart rate, and nerves from the sympathetic trunk act to increase the heart rate.[7] These nerves form a network of nerves that lies over the heart called the cardiac plexus.[7][27]
The vagus nerve is a long, wandering nerve that emerges from the brainstem and provides parasympathetic stimulation to a large number of organs in the thorax and abdomen, including the heart.[29] The nerves from the sympathetic trunk emerge through the T1-T4 thoracic ganglia and travel to both the sinoatrial and atrioventricular nodes, as well as to the atria and ventricles. The ventricles are more richly innervated by sympathetic fibers than parasympathetic fibers. Sympathetic stimulation causes the release of the neurotransmitter norepinephrine (also known as noradrenaline) at the neuromuscular junction of the cardiac nerves. This shortens the repolarization period, thus speeding the rate of depolarization and contraction, which results in an increased heart rate. It opens chemical or ligand-gated sodium and calcium ion channels, allowing an influx of positively charged ions.[7] Norepinephrine binds to the beta–1 receptor.[7]
Development

The heart is the first functional organ to develop and starts to beat and pump blood at about three weeks into embryogenesis. This early start is crucial for subsequent embryonic and prenatal development.
The heart derives from splanchnopleuric mesenchyme in the neural plate which forms the cardiogenic region. Two endocardial tubes form here that fuse to form a primitive heart tube known as the tubular heart.[30] Between the third and fourth week, the heart tube lengthens, and begins to fold to form an S-shape within the pericardium. This places the chambers and major vessels into the correct alignment for the developed heart. Further development will include the septa and valves formation and remodelling of the heart chambers. By the end of the fifth week the septa are complete and the heart valves are completed by the ninth week.[7]
Before the fifth week, there is an opening in the fetal heart known as the foramen ovale. The foramen ovale allowed blood in the fetal heart to pass directly from the right atrium to the left atrium, allowing some blood to bypass the lungs. Within seconds after birth, a flap of tissue known as the septum primum that previously acted as a valve closes the foramen ovale and establishes the typical cardiac circulation pattern. A depression in the surface of the right atrium remains where the foramen ovale once walls, called the fossa ovalis.[7]
The embryonic heart begins beating at around 22 days after conception (5 weeks after the last normal menstrual period, LMP). It starts to beat at a rate near to the mother's which is about 75–80 beats per minute (bpm). The embryonic heart rate then accelerates and reaches a peak rate of 165–185 bpm early in the early 7th week (early 9th week after the LMP).[31][32] After 9 weeks (start of the fetal stage) it starts to decelerate, slowing to around 145 (±25) bpm at birth. There is no difference in female and male heart rates before birth.[33]
Physiology
Blood flow

The heart functions as a pump in the circulatory system to provide a continuous flow of blood throughout the body. This circulation consists of the systemic circulation to and from the body and the pulmonary circulation to and from the lungs. Blood in the pulmonary circulation exchanges carbon dioxide for oxygen in the lungs through the process of respiration. The systemic circulation then transports oxygen to the body and returns carbon dioxide and relatively deoxygenated blood to the heart for transfer to the lungs.[7]
The right heart collects deoxygenated blood from two large veins, the superior and inferior venae cavae. Blood collects in the right and left atrium continuously.[7] The superior vena cava drains blood from above the diaphragm and empties into the upper back part of the right atrium. The inferior vena cava drains the blood from below the diaphragm and empties into the back part of the atrium below the opening for the superior vena cava. Immediately above and to the middle of the opening of the inferior vena cava is the opening of the thin-walled coronary sinus.[7] Additionally, the coronary sinus returns deoxygenated blood from the myocardium to the right atrium. The blood collects in the right atrium. When the right atrium contracts, the blood is pumped through the tricuspid valve into the right ventricle. As the right ventricle contracts, the tricuspid valve closes and the blood is pumped into the pulmonary trunk through the pulmonary valve. The pulmonary trunk divides into pulmonary arteries and progressively smaller arteries throughout the lungs, until it reaches capillaries. As these pass by alveoli carbon dioxide is exchanged for oxygen. This happens through the passive process of diffusion.
In the left heart, oxygenated blood is returned to the left atrium via the pulmonary veins. It is then pumped into the left ventricle through the mitral valve and into the aorta through the aortic valve for systemic circulation. The aorta is a large artery that branches into many smaller arteries, arterioles, and ultimately capillaries. In the capillaries, oxygen and nutrients from blood are supplied to body cells for metabolism, and exchanged for carbon dioxide and waste products.[7] Capillary blood, now deoxygenated, travels into venules and veins that ultimately collect in the superior and inferior vena cavae, and into the right heart.
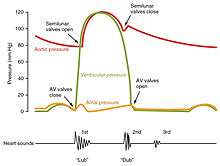
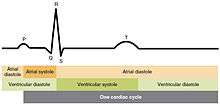
Cardiac cycle

The cardiac cycle refers to a complete heartbeat which includes systole and diastole and the intervening pause.[9] The cycle begins with contraction of the atria and ends with relaxation of the ventricles. Systole refers to contraction of the atria or ventricles of the heart. Diastole is when the atria or ventricles relax and fill with blood. The atria and ventricles work in concert, so in systole when the ventricles are contracting, the atria are relaxed and collecting blood. When the ventricles are relaxed in diastole, the atria contract to pump blood to the ventricles. This coordination ensures blood is pumped efficiently to the body.[7]
At the beginning of the cardiac cycle, in early diastole, both the atria and ventricles are relaxed. Since blood moves from areas of high pressure to areas of low pressure, when the chambers are relaxed, blood will flow into the atria (through the coronary sinus and the pulmonary veins). As the atria begin to fill, the pressure will rise so that the blood will move from the atria into the ventricles. In late diastole the atria contract, pumping more blood into the ventricles. This causes a rise in pressure in the ventricles. As the ventricles reach systole, blood will be pumped into the pulmonary artery (right ventricle) or aorta (left ventricle).[9]
When the atrioventricular valves (tricuspid and mitral) are open, during blood flow to the ventricles, the aortic and pulmonary valves are closed to prevent backflow into the ventricles. When the ventricular pressure is greater than the atrial pressure the tricuspid and mitral valves will shut. When the ventricles contract the pressure forces the aortic and pulmonary valves open. As the ventricles relax, the aortic and pulmonary valves will close in response to decreased pressure.[9]
Cardiac output
Cardiac output (CO) is a measurement of the amount of blood pumped by each ventricle (stroke volume) in one minute. This is calculated by multiplying the stroke volume (SV) by the beats per minute of the heart rate (HR). So that: CO = SV x HR.[7] The cardiac output is normalized to body size through body surface area and is called the cardiac index.
The average cardiac output, using an average stroke volume of about 70mL, is 5.25 L/min, with a normal range of 4.0–8.0 L/min.[7] The stroke volume is normally measured using an echocardiogram and can be influenced by the size of the heart, physical and mental condition of the individual, sex, contractility, duration of contraction, preload and afterload.[7]
Preload refers to the filling pressure of the atria at the end of diastole, when they are at their fullest. A main factor is how long it takes the ventricles to fill—if the ventricles contract faster, then there is less time to fill and the preload will be less.[7] Preload can also be affected by a person's blood volume. The force of each contraction of the heart muscle is proportional to the preload, described as the Frank-Starling mechanism. This states that the force of contraction is directly proportional to the initial length of muscle fiber, meaning a ventricle will contract more forcefully, the more it is stretched.[7][34]
Afterload, or how much pressure the heart must generate to eject blood at systole, is influenced by vascular resistance. It can be influenced by narrowing of the heart valves (stenosis) or contraction or relaxation of the peripheral blood vessels.[7]
The strength of heart muscle contractions controls the stroke volume. This can be influenced positively or negatively by agents termed inotropes.[35] These agents can be a result of changes within the body, or be given as drugs as part of treatment for a medical disorder, or as a form of life support, particularly in intensive care units. Inotropes that increase the force of contraction are "positive" inotropes, and include sympathetic agents such as adrenaline, noradrenaline and dopamine.[36] "Negative" inotropes decrease the force of contraction and include calcium channel blockers.[35]
Electrical conduction

The normal rhythmical heart beat, called sinus rhythm, is established by the sinoatrial node, the heart's pacemaker. Here an electrical signal is created that travels through the heart, causing the heart muscle to contract.
The sinoatrial node is found in the upper part of the right atrium near to the junction with the superior vena cava.[37] The electrical signal generated by the sinoatrial node travels through the right atrium in a radial way that is not completely understood. It travels to the left atrium via Bachmann's bundle, such that the muscles of the left and right atria contract together.[38][39][40] The signal then travels to the atrioventricular node. This is found at the bottom of the right atrium in the atrioventricular septum—the boundary between the right atrium and the left ventricle. The septum is part of the cardiac skeleton, tissue within the heart that the electrical signal cannot pass through, which forces the signal to pass through the atrioventricular node only.[7] The signal then travels along the bundle of His to left and right bundle branches through to the ventricles of the heart. In the ventricles the signal is carried by specialized tissue called the Purkinje fibers which then transmit the electric charge to the heart muscle.[41]

Heart rate
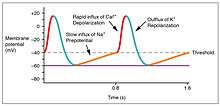
The normal resting heart rate is called the sinus rhythm, created and sustained by the sinoatrial node, a group of pacemaking cells found in the wall of the right atrium. Cells in the sinoatrial node do this by creating an action potential. The cardiac action potential is created by the movement of specific electrolytes into and out of the pacemaker cells. The action potential then spreads to nearby cells.[42]
When the sinoatrial cells are resting, they have a negative charge on their membranes. However a rapid influx of sodium ions causes the membrane's charge to become positive. This is called depolarisation and occurs spontaneously.[7] Once the cell has a sufficiently high charge, the sodium channels close and calcium ions then begin to enter the cell, shortly after which potassium begins to leave it. All the ions travel through ion channels in the membrane of the sinoatrial cells. The potassium and calcium only start to move out of and into the cell once it has a sufficiently high charge, and so are called voltage-gated. Shortly after this, the calcium channels close and potassium channels open, allowing potassium to leave the cell. This causes the cell to have a negative resting charge and is called repolarization. When the membrane potential reaches approximately −60 mV, the potassium channels close and the process may begin again.[7]
The ions move from areas where they are concentrated to where they are not. For this reason sodium moves into the cell from outside, and potassium moves from within the cell to outside the cell. Calcium also plays a critical role. Their influx through slow channels means that the sinoatrial cells have a prolonged "plateau" phase when they have a positive charge. A part of this is called the absolute refractory period. Calcium ions also combine with the regulatory protein troponin C in the troponin complex to enable contraction of the cardiac muscle, and separate from the protein to allow relaxation.[43]
The adult resting heart rate ranges from 60 to 100 bpm. The resting heart rate of a newborn can be 129 beats per minute (bpm) and this gradually decreases until maturity.[44] An athlete's heart rate can be lower than 60 bpm. During exercise the rate can be 150 bpm with maximum rates reaching from 200 to 220 bpm.[7]
Influences
The normal sinus rhythm of the heart, giving the resting heart rate, is influenced a number of factors. The cardiovascular centres in the brainstem that control the sympathetic and parasympathetic influences to the heart through the vagus nerve and sympathetic trunk.[45] These cardiovascular centres receive input from a series of receptors including baroreceptors, sensing stretch the stretching of blood vessels and chemoreceptors, sensing the amount of oxygen and carbon dioxide in the blood and its pH. Through a series of reflexes these help regulate and sustain blood flow.[7]
Baroreceptors are stretch receptors located in the aortic sinus, carotid bodies, the venae cavae, and other locations, including pulmonary vessels and the right side of the heart itself. Baroreceptors fire at a rate determined by how much they are stretched,[46] which is influenced by blood pressure, level of physical activity, and the relative distribution of blood. With increased pressure and stretch, the rate of baroreceptor firing increases, and the cardiac centers decrease sympathetic stimulation and increase parasympathetic stimulation . As pressure and stretch decrease, the rate of baroreceptor firing decreases, and the cardiac centers increase sympathetic stimulation and decrease parasympathetic stimulation.[7] There is a similar reflex, called the atrial reflex or Bainbridge reflex, associated with varying rates of blood flow to the atria. Increased venous return stretches the walls of the atria where specialized baroreceptors are located. However, as the atrial baroreceptors increase their rate of firing and as they stretch due to the increased blood pressure, the cardiac center responds by increasing sympathetic stimulation and inhibiting parasympathetic stimulation to increase heart rate. The opposite is also true.[7] Chemoreceptors present in the carotid body or adjacent to the aorta in an aortic body respond to the blood's oxygen, carbon dioxide levels. Low oxygen or high carbon dioxide will stimulate firing of the receptors.[47]
Exercise and fitness levels, age, body temperature, basal metabolic rate, and even a person's emotional state can all affect the heart rate. High levels of the hormones epinephrine, norepinephrine, and thyroid hormones can increase the heart rate. The levels of electrolytes including calcium, potassium, and sodium can also influence the speed and regularity of the heart rate; low blood oxygen, low blood pressure and dehydration may increase it.[7]
Heart sounds
The closure of the heart valves causes the heart sounds.
One of the simplest methods of assessing the heart's condition is to listen to it using a stethoscope.[7] Typically, healthy hearts have only two audible heart sounds, called S1 and S2. The first heart sound S1, is the sound created by the closing of the atrioventricular valves during ventricular contraction and is normally described as "lub". The second heart sound, S2, is the sound of the semilunar valves closing during ventricular diastole and is described as "dub".[7] Each sound consists of two components, reflecting the slight difference in time as the two valves close.[48] S2 may split into two distinct sounds, either as a result of inspiration or different valvular or cardiac problems.[48] Additional heart sounds may also be present and these give rise to gallop rhythms. A third heart sound, S3 usually indicates an increase in ventricular blood volume. A fourth heart sound S4 is referred to as an atrial gallop and is produced by the sound of blood being forced into a stiff ventricle. The combined presence of S3 and S4 give a quadruple gallop.[7]
Heart murmurs are abnormal heart sounds which can be either pathological or benign.[49] One example of a murmur is Still's murmur, which presents a musical sound in children, has no symptoms and disappears in adolescence.[50]
A different type of sound, a pericardial friction rub can be heard in cases of pericarditis where the inflamed membranes can rub together.[51]
Clinical significance
Disease


Cardiovascular diseases, which include diseases of the heart, are the leading cause of death worldwide.[52] The majority of cardiovascular disease is noncommunicable and related to lifestyle and other factors, becoming more prevalent with ageing.[52] Heart disease is a major cause of death, accounting for an average of 30% of all deaths in 2008, globally.[11] This rate varies from a lower 28% to a high 40% in high-income countries.[12] Doctors that specialise in the heart are called cardiologists. Many other medical professionals are involved in treating diseases of the heart, including doctors such as general practitioners, cardiothoracic surgeons and intensivists, and allied health practitioners including physiotherapists and dieticians.[53]
Coronary artery disease is also known as ischemic heart disease, is caused by atherosclerosis – a build-up of plaque along the inner walls of the arteries which narrows them, reducing the blood flow to the heart.[54] A stable plaque may cause chest pain (angina) or breathlessness during exercise or at rest, or no symptoms at all. A ruptured plaque can block a blood vessel and lead to ischaemia of the heart muscle, causing unstable angina or a heart attack.[55] In the worst case this may cause cardiac arrest, a sudden and utter loss of output from the heart.[56] Obesity, high blood pressure, uncontrolled diabetes, smoking and high cholesterol can all increase the risk of developing atherosclerosis and coronary artery disease.[52][54]
Heart failure is where the heart can't beat out enough blood to meet the needs of the body.[54] It is generally a chronic condition, associated with age, that progresses gradually.[57] Each side of the heart can fail independently of the other, resulting in heart failure of the right heart or the left heart. Left heart failure can also lead to right heart failure (cor pulmonale) by increasing strain on the right heart. If the heart is unable to pump sufficient blood, it may accumulate throughout the body, causing breathlessness in the lungs (pulmonary congestion; pulmonary edema), swelling (edema) of the feet or other gravity-dependent areas, decrease exercise tolerance, or cause other clinical signs such as an enlarged liver, cardiac murmurs, or a raised jugular venous pressure. Common causes of heart failure include coronary artery disease, valve disorders and diseases of cardiac muscle.[58]
Cardiomyopathy is a noticeable deterioration of the heart muscle's ability to contract, which can lead to heart failure. The causes of many types of cardiomyopathy are poorly understood; some identified causes include alcohol, toxins, systemic disease such as sarcoidosis, and congenital conditions such as HOCM. The types of cardiomyopathy are described according to how they affect heart muscle. Cardiomyopathy can cause the heart to become enlarged (hypertrophic cardiomyopathy), constrict the outflow tracts of the heart (restrictive cardiomyopathy), or cause the heart to dilate and impact the efficiency of its beating (dilated cardiomyopathy).[59] HOCM is often undiagnosed and can cause sudden death in young athletes.[7]
Heart murmurs are abnormal heart sounds which can be either related to disease or benign, and there are several kinds.[60] There are normally two heart sounds, and abnormal heart sounds can either be extra sounds, or "murmurs" related to the flow of blood between the sounds. Murmurs are graded by volume, from 1 (the quietest), to 6 (the loudest), and evaluated by their relationship to the heart sounds, position in the cardiac cycle, and additional features such as their radiation to other sites, changes with a person's position, the frequency of the sound as determined by the side of the stethoscope by which they are heard, and site at which they are heard loudest.[60]Phonocardiograms can record these sounds,[7] and echocardiograms are generally required for their diagnosis.[61] Murmurs can result from valvular heart diseases due to narrowing (stenosis), or regurgitation of any of the main heart valves, such as aortic stenosis, mitral regurgitation or mitral valve prolapse. They can also result from a number of other disorders, including atrial and ventricular septal defects.[60] Two common and infective causes of heart murmurs are infective endocarditis and rheumatic fever, particularly in developing countries. Infective endocarditis involves colonisation of a heart valve,[62] and rheumatic fever involves an initial bacterial infection by Group A streptococcus followed by a reaction against heart tissue that resembles the streptococcal antigen.[63]
Abnormalities in the normal sinus rhythm of the heart can prevent the heart from effectively pumping blood, and are generally identified by ECG. These cardiac arrhythmias can cause an abnormal but regular heart rhythm, such as a rapid heart rate (tachycardia, classified as arising from above the ventricles or from the ventricles) or a slow heart rate (bradycardia); or may result in irregular rhythms. Tachycardia is generally defined as a heart rate faster than 100 beats per minute, and bradycardia as a heart rate slower than 60.[64] Asystole is the cessation of heart rhythm. A random and varying rhythm is classified as atrial or ventricular fibrillation depending if the electrical activity originates in the atria or the ventricles.[64] Abnormal conduction can cause a delay or unusual order of contraction of the heart muscle. This can be a result of a disease process, such as heart block, or congenital, such as Wolff-Parkinson-White syndrome.[64]
Diseases may also affect the pericardium which surrounds the heart, which when inflamed is called pericarditis. This may result from infective causes (such as glandular fever, cytomegalovirus, coxsackievirus, tuberculosis or Q fever), systemic disorders such as amyloidosis or sarcoidosis, tumours, high uric acid levels, and other causes. This inflammation affects the ability of the heart to pump effectively. When fluid builds up in the pericardium this is called pericardial effusion, which when it causes acute heart failure is called cardiac tamponade. This may be blood from a traumatic injury or fluid from an effusion.[65] This can compress the heart and adversely affect the function of the heart. The fluid can be removed from the pericardial sac using a syringe in a procedure called pericardiocentesis.[66]
The heart can be affected by congenital diseases. These include failure of the developmental foramen ovale to close, present in up to 25% of people;[67] ventricular or atrial septal defects, congenital diseases of the heart valves (e.g. congenital aortic stenosis) or disease relating to blood vessels or blood flow from the heart (such as a patent ductus arteriosus or aortic coarctation).;[68][69] These may cause symptoms at a variety of ages. If unoxygenated blood travels directly from the right to the left side of the heart, it may be noticed at birth, as it may cause a baby to become blue (cyanotic) such as Tetralogy of Fallot. A heart problem may impact a child's ability to grow.[68] Some causes rectify with time and are regarded as benign. Other causes may be incidentally detected on a cardiac examination. These disorders are often diagnosed on an echocardiogram.[69]
Diagnosis
Heart disease is diagnosed by the taking of a medical history, a cardiac examination, and further investigations, including blood tests, echocardiograms, ECGs and imaging. Other invasive procedures such as cardiac catheterisation can also play a role.[70]
Examination
The cardiac examination includes inspection, feeling the chest with the hands (palpation) and listening with a stethoscope (auscultation).[71][72] It involves assessment of signs that may be visible on a person's hands (such as splinter haemorrhages), joints and other areas. A person's pulse is taken, usually at the radial artery near the wrist, in order to assess for the rhythm and strength of the pulse. The blood pressure is taken, using either a manual or automatic sphygmomanometer or using a more invasive measurement from within the artery. Any elevation of the jugular venous pulse is noted. A person's chest is felt for any transmitted vibrations from the heart, and then listened to with a stethoscope. A normal heart has two hearts sounds – additional heart sounds or heart murmurs may also be able to be heard and may point to disease. Additional tests may be conducted to assess a person's heart murmurs if they are present, and peripheral signs of heart disease such as swollen feet or fluid in the lungs may be assessed.[72]
Blood tests
Blood tests play an important role in the diagnosis and treatment of many cardiovascular conditions.
Troponin is a sensitive biomarker for a heart with insufficient blood supply. It is released 4–6 hours after injury, and usually peaks at about 12–24 hours.[36] Two tests of troponin are often taken – one at the time of initial presentation, and another within 3–6 hours,[73] with either a high level or a significant rise being diagnostic. A test for brain natriuretic peptide (BNP) can be used to evaluate for the presence of heart failure, and rises when there is increased demand on the left ventricle. These tests are considered biomarkers because they are highly specific for cardiac disease.[74] Testing for the MB form of creatine kinase provides information about the heart's blood supply, but is used less frequently because it is less specific and sensitive.[75]
Other blood tests are often taken to help understand a person's general health and risk factors that may contribute to heart disease. These often include a full blood count investigating for anaemia, and basic metabolic panel that may reveal any disturbances in electrolytes. A coagulation screen is often required to ensure that the right level of anticoagulation is given. Fasting lipids and fasting blood glucose (or an HbA1c level) are often ordered to evaluate a person's cholesterol and diabetes status, respectively.[76]
Electrocardiogram
Using surface electrodes on the body, it is possible to record the electrical activity of the heart. This tracing of the electrical signal is the electrocardiogram (ECG) or (EKG). An ECG is a bedside test and involves the placement of ten leads on the body. This produces a "12 lead" ECG (three extra leads are calculated mathematically, and one lead is a ground).[77]
There are five prominent features on the ECG: the P wave (atrial depolarisation), the QRS complex (ventricular depolarisation[lower-alpha 8]) and the T wave (ventricular repolarisation).[7] As the heart cells contract, they create a current that travels through the heart. A downward deflection on the ECG implies cells are becoming more positive in charge ("depolarising") in the direction of that lead, whereas an upward inflection implies cells are becoming more negative ("repolarising") in the direction of the lead. This depends on the position of the lead, so if a wave of depolarising moved from left to right, a lead on the left would show a negative deflection, and a lead on the right would show a positive deflection. The ECG is a useful tool in detecting rhythm disturbances and in detecting insufficient blood supply to the heart.[77] Sometimes abnormalities are suspected, but not immediately visible on the ECG. Testing when exercising can be used to provoke an abnormality, or an ECG can be worn for a longer period such as a 24-hour Holter monitor if a suspected rhythm abnormality is not present at the time of assessment.[77]
Imaging
Several imaging methods can be used to assess the anatomy and function of the heart, including ultrasound (echocardiography), angiography, CT scans, MRI and PET. An echocardiogram is an ultrasound of the heart used to measure the heart's function, assess for valve disease, and look for any abnormalities. Echocardiography can be conducted by a probe on the chest ("transthoracic") or by a probe in the esophagus ("transoesophageal"). A typical echocardiography report will include information about the width of the valves noting any stenosis, whether there is any backflow of blood (regurgitation) and information about the blood volumes at the end of systole and diastole, including an ejection fraction, which describes how much blood is ejected from the left and right ventricles after systole. Ejection fraction can then be obtained by dividing the volume ejected by the heart (stroke volume) by the volume of the filled heart (end-diastolic volume).[78] Echocardiograms can also be conducted under circumstances when the body is more stressed, in order to examine for signs of lack of blood supply. This cardiac stress test involves either direct exercise, or where this is not possible, injection of a drug such as dobutamine.[72]
CT scans, chest X-rays and other forms of imaging can help evaluate the heart's size, evaluate for signs of pulmonary oedema, and indicate whether there is fluid around the heart. They are also useful for evaluating the aorta, the major blood vessel which leaves the heart.[72]
Treatment
A number of medications are used to treat diseases of the heart, or ameliorate symptoms.
For diseases of the heart rate or rhythm, a number of different antiarrhythmic agents are used. These may interfere with electrolyte channels and thus the cardiac action potential (such as calcium channel blockers, sodium channel blockers), interfere with stimulation of the heart by the sympathetic nervous system (beta blockers), or interfere with the movement of sodium and potassium across the cell membrane, such as digoxin.[79] Other examples include atropine for slow rhythms, and amiodarone for irregular rhythms. Such medications are not the only way of treating diseases of heart rate or rhythm. In the context of a new-onset irregular heart rhythm (atrial fibrillation), immediate electrical cardioversion may be attempted. For a slow heartbeat or heart block, a pacemaker or defibrillator may be inserted.[76] The acuity of onset often affects how a rhythm disturbance is managed, as does whether a rhythm causes hemodynamic instability, such as low blood pressure or symptoms. An instigating cause is investigated for, such as a heart attack, medication, or metabolic problem.[76]
For ischaemic heart disease, treatment also includes amelioration of symptoms. This includes nitroglycerin, beta blockers and, in the context of an acute event, stronger pain relief such as morphine and other opiates. Many of these drugs have additional protective benefits, by decreasing the sympathetic tone on the heart that occurs with the pain, or by dilating blood vessels (GTN).[76]
Treatment of heart disease includes primary and secondary prevention to prevent the occurrence or worsening of symptoms and atherosclerosis. This includes recommendations to cease smoking, decrease alcohol consumption, increase exercise, and make modifications to their diet to decrease the consumption of fats and sugars. Medications may also be given to help better control concurrent diabetes. Statins or other drugs such as fibrates may also be given to decrease a person's cholesterol levels. Blood pressure medication may also be commenced or modified.[76]
For many diseases of the heart, including atrial fibrillation and valvular disease, and after a heart operation, anticoagulation in the form of aspirin, warfarin, clopidogrel or novel oral anticoagulants is often given simultaneously, because of an increased risk of stroke or, in the context of a clotted heart vessel, rethrombosis.[76]
Surgery
Surgery, when considered necessary for diseases of the heart, can take place via an open operation or via small guidewires inserted via peripheral arteries ("percutaneous coronary intervention"). Percutaneous coronary intervention is usually used in the context of an acute coronary syndrome, and may be used to insert a stent.[80]
Coronary artery bypass surgery is one such operation. In this operation, one or more arteries surrounding the heart that have become narrowed are bypassed. This is done by taking blood vessels harvested from another part of the body. Commonly harvested veins include the saphenous veins or the internal mammary artery. Because this operation involves the heart tissue, a machine is used so that blood can bypass the heart during the operation.[80]
Heart valve repair or valve replacement are options for diseases of the heart valves.[80]
History
Ancient

Humans have known about the heart since ancient times, although its precise function and anatomy were not clearly understood.[81] From the primarily religious views of earlier societies towards the heart, ancient Greeks are considered to have been the primary seat of scientific understanding of the heart in the ancient world.[82][83][84] Aristotle considered the heart to be organ responsible for creating blood; Plato considered the heart as the source of circulating blood and Hippocrates noted blood circulating cyclically from the body through the heart to the lungs.[82][84] Erasistratos (304–250 BCE) noted the heart as a pump, causing dilation of blood vessels, and noted that arteries and veins both radiate from the heart, becoming progressively smaller with distance, although he believed they were filled with air and not blood. He also discovered the heart valves.[82]
The Greek physician Galen (2nd century CE) knew blood vessels carried blood and identified venous (dark red) and arterial (brighter and thinner) blood, each with distinct and separate functions.[82] Galen, noting the heart as the hottest organ in the body, concluded that it provided heat to the body.[84] The heart did not pump blood around, the heart's motion sucked blood in during diastole and the blood moved by the pulsation of the arteries themselves.[84] Galen believed the arterial blood was created by venous blood passing from the left ventricle to the right through 'pores' between the ventricles.[81] Air from the lungs passed from the lungs via the pulmonary artery to the left side of the heart and created arterial blood.[84]
These ideas went unchallenged for almost a thousand years.[81][84]
Pre-modern
The earliest descriptions of the coronary and pulmonary circulation systems can be found in the Commentary on Anatomy in Avicenna's Canon, published in 1242 by Ibn al-Nafis.[85] In his manuscript, al-Nafis wrote that blood passes through the pulmonary circulation instead of moving from the right to the left ventricle as previously believed by Galen.[86] His work was later translated into Latin by Andrea Alpago.[87]
In Europe, the teachings of Galen continued to dominate the academic community and his doctrines were adopted as the official canon of the Church. Andreas Vesalius questioned some of Galen's beliefs of the heart in De humani corporis fabrica (1543), but his magnum opus was interpreted as a challenge to the authorities and he was subjected to a number of attacks.[88] Michael Servetus wrote in Christianismi Restitutio (1553) that blood flows from one side of the heart to the other via the lungs.[88]
Modern

A breakthrough in understanding the flow of blood through the heart and body came with the publication of De Motu Cordis (1628) by the English physician William Harvey. Harvey's book completely describes the systemic circulation and the mechanical force of the heart, leading to an overhaul of the Galenic doctrines.[84] Otto Frank (1865–1944) was a German physiologist; among his many published works are detailed studies of this important heart relationship. Ernest Starling (1866–1927) was an important English physiologist who also studied the heart. Although they worked largely independently, their combined efforts and similar conclusions have been recognized in the name "Frank–Starling mechanism".[7]
Although Purkinje fibers and the bundle of His were discovered as early as the 19th century, their specific role in the electrical conduction system of the heart remained unknown until Sunao Tawara published his monograph, titled Das Reizleitungssystem des Säugetierherzens, in 1906. Tawara's discovery of the atrioventricular node prompted Arthur Keith and Martin Flack to look for similar structures in the heart, leading to their discovery of the sinoatrial node several months later. These structures form the anatomical basis of the electrocardiogram, whose inventor, Willem Einthoven, was awarded the Nobel Prize in Medicine or Physiology in 1924.[89]
The first successful heart transplantation was performed in 1967 by the South African surgeon Christiaan Barnard at Groote Schuur Hospital in Cape Town. This marked an important milestone in cardiac surgery, capturing the attention of both the medical profession and the world at large. However, long-term survival rates of patients were initially very low. Louis Washkansky, the first recipient of a donated heart, died 18 days after the operation while other patients did not survive for more than a few weeks.[90] The American surgeon Norman Shumway has been credited for his efforts to improve transplantation techniques, along with pioneers Richard Lower, Vladimir Demikhov and Adrian Kantrowitz. As of March 2000, more than 55,000 heart transplantations have been performed worldwide.[91]
By the middle of the 20th century, heart disease had surpassed infectious disease as the leading cause of death in the United States, and it is currently the leading cause of deaths worldwide. Since 1948, the ongoing Framingham Heart Study has shed light on the effects of various influences on the heart, including diet, exercise, and common medications such as aspirin. Although the introduction of ACE inhibitors and beta blockers has improved the management of chronic heart failure, the disease continues to be an enormous medical and societal burden, with 30 to 40% of patients dying within a year of receiving the diagnosis.[92]
Society and culture
| ||
| jb (F34) "heart" in hieroglyphs |
|---|
Symbolism



As one of the vital organs, the heart was long identified as the center of the entire body, the seat of life, or emotion, or reason, will, intellect, purpose or the mind.[93] The heart is an emblematic symbol in many religions, signifying "truth, conscience or moral courage in many religions – the temple or throne of God in Islamic and Judeo-Christian thought; the divine centre, or atman, and the third eye of transcendent wisdom in Hinduism; the diamond of purity and essence of the Buddha; the Taoist centre of understanding."[93]
In the Hebrew Bible, the word for heart, lev, is used in these meanings, as the seat of emotion, the mind, and referring to the anatomical organ. It is also connected in function and symbolism to the stomach.[94]
An important part of the concept of the soul in Ancient Egyptian religion was thought to be the heart, or ib. The ib or metaphysical heart was believed to be formed from one drop of blood from the child's mother's heart, taken at conception.[95] To ancient Egyptians, the heart was the seat of emotion, thought, will, and intention. This is evidenced by Egyptian expressions which incorporate the word ib, such as Awi-ib for "happy" (literally, "long of heart"), Xak-ib for "estranged" (literally, "truncated of heart").[96] In Egyptian religion, the heart was the key to the afterlife. It was conceived as surviving death in the nether world, where it gave evidence for, or against, its possessor. It was thought that the heart was examined by Anubis and a variety of deities during the Weighing of the Heart ceremony. If the heart weighed more than the feather of Maat, which symbolized the ideal standard of behavior. If the scales balanced, it meant the heart's possessor had lived a just life and could enter the afterlife; if the heart was heavier, it would be devoured by the monster Ammit.[97]
The Chinese character for "heart", 心, derives from a comparatively realistic depiction of a heart (indicating the heart chambers) in seal script.[98] The Chinese word xīn also takes the metaphorical meanings of "mind", "intention", or "core".[99] In Chinese medicine, the heart is seen as the center of 神 shén "spirit, consciousness".[100] The heart is associated with the small intestine, tongue, governs the six organs and five viscera, and belongs to fire in the five elements.[101]
The Sanskrit word for heart is hṛd or hṛdaya, found in the oldest surviving Sanskrit text, the Rigveda. In Sanskrit, it may mean both the anatomical object and "mind" or "soul", representing the seat of emotion. Hrd may be a cognate of the word for heart in Greek, Latin, and English.[102][103]
Many classical philosophers and scientists, including Aristotle, considered the heart the seat of thought, reason, or emotion, often disregarding the brain as contributing to those functions.[104] The identification of the heart as the seat of emotions in particular is due to the Roman physician Galen, who also located the seat of the passions in the liver, and the seat of reason in the brain.[105]
The heart also played a role in the Aztec system of belief. The most common form of human sacrifice practiced by the Aztecs was heart-extraction. The Aztec believed that the heart (tona) was both the seat of the individual and a fragment of the Sun's heat (istli). To this day, the Nahua consider the Sun to be a heart-soul (tona-tiuh): "round, hot, pulsating".[106]
In Catholicism, there has been a long tradition of veneration of the heart, stemming from worship of the wounds of Jesus Christ which gained prominence from the mid sixteenth century.[107] This tradition influenced the development of the medieval Christian devotion to the Sacred Heart of Jesus and the parallel worship of Immaculate Heart of Mary, made popular by John Eudes.[108]
The expression of a broken heart is a cross-cultural reference to grief for a lost one or to unfulfilled romantic love.
The notion of "Cupid's arrows" is ancient, due to Ovid, but while Ovid describes Cupid as wounding his victims with his arrows, it is not made explicit that it is the heart that is wounded. The familiar iconography of Cupid shooting little heart symbols is a Renaissance theme that became tied to Valentine's day.[93]
Food
Animal hearts are widely consumed as food. As they are almost entirely muscle, they are high in protein. They are often included in dishes with other offal, for example in the pan-Ottoman kokoretsi.
Chicken hearts are considered to be giblets, and are often grilled on skewers: Japanese hāto yakitori, Brazilian churrasco de coração, Indonesian chicken heart satay.[109] They can also be pan-fried, as in Jerusalem mixed grill. In Egyptian cuisine, they can be used, finely chopped, as part of stuffing for chicken.[110] Many recipes combined them with other giblets, such as the Mexican pollo en menudencias[111] and the Russian ragu iz kurinyikh potrokhov.[112]
The hearts of beef, pork, and mutton can generally be interchanged in recipes. As heart is a hard-working muscle, it makes for "firm and rather dry" meat,[113] so is generally slow-cooked. Another way of dealing with toughness is to julienne the meat, as in Chinese stir-fried heart.[114]
Beef heart may be grilled or braised.[115] In the Peruvian anticuchos de corazón, barbecued beef hearts are grilled after being tenderized through long marination in a spice and vinegar mixture. An Australian recipe for "mock goose" is actually braised stuffed beef heart.[116]
Pig heart is stewed, poached, braised,[117] or made into sausage. The Balinese oret is a sort of blood sausage made with pig heart and blood. A French recipe for cœur de porc à l'orange is made of braised heart with an orange sauce.
Other animals
Other vertebrates
The size of the heart varies among the different animal groups, with hearts in vertebrates ranging from those of the smallest mice (12 mg) to the blue whale (600 kg).[118] In vertebrates, the heart lies in the middle of the ventral part of the body, surrounded by a pericardium.[119] which in some fish may be connected to the peritoneum.[120]
The SA node is found in all amniotes but not in more primitive vertebrates. In these animals, the muscles of the heart are relatively continuous and the sinus venosus coordinates the beat which passes in a wave through the remaining chambers. Indeed, since the sinus venosus is incorporated into the right atrium in amniotes, it is likely homologous with the SA node. In teleosts, with their vestigial sinus venosus, the main centre of coordination is, instead, in the atrium. The rate of heartbeat varies enormously between different species, ranging from around 20 beats per minute in codfish to around 600 in hummingbirds[121] and up to 1200 bpm in the ruby-throated hummingbird.[122]
Double circulatory systems

- Pulmonary vein
- Left atrium
- Right atrium
- Ventricle
- Conus arteriosus
- Sinus venosus
Adult amphibians and most reptiles have a double circulatory system, meaning a circulatory system divided into arterial and venous parts. However, the heart itself is not completely separated into two sides. Instead, it is separated into three chambers – two atria and one ventricle. Blood returning from both the systemic circulation and the lungs is returned, and blood is pumped simultaneously into the systemic circulation and the lungs. The double system allows blood to circulate to and from lungs which deliver oxygenated blood directly to the heart.[123]
In reptiles, the heart is usually situated around the middle of the thorax, and in snakes, usually between the junction of the upper first and second third. There is a heart with three chambers: two atria and one ventricle. The ventricle is incompletely separated into two halves by a wall (septum), with a considerable gap near the pulmonary artery and aortic openings. In most reptilian species, there appears to be little, if any, mixing between the bloodstreams, so the aorta receives, essentially, only oxygenated blood.[121][123] The exception to this rule is crocodiles, which have a four-chambered heart.[124]
In the heart of lungfish, the septum extends part-way into the ventricle. This allows for some degree of separation between the de-oxygenated bloodstream destined for the lungs and the oxygenated stream that is delivered to the rest of the body. The absence of such a division in living amphibian species may be partly due to the amount of respiration that occurs through the skin; thus, the blood returned to the heart through the venae cavae is already partially oxygenated. As a result, there may be less need for a finer division between the two bloodstreams than in lungfish or other tetrapods. Nonetheless, in at least some species of amphibian, the spongy nature of the ventricle does seem to maintain more of a separation between the bloodstreams. Also, the original valves of the conus arteriosus have been replaced by a spiral valve that divides it into two parallel parts, thereby helping to keep the two bloodstreams separate.[121]
The fully divided heart
Archosaurs (crocodilians and birds) and mammals show complete separation of the heart into two pumps for a total of four heart chambers; it is thought that the four-chambered heart of archosaurs evolved independently from that of mammals. In crocodilians, there is a small opening, the foramen of Panizza, at the base of the arterial trunks and there is some degree of mixing between the blood in each side of the heart, during a dive underwater;[125][126] thus, only in birds and mammals are the two streams of blood – those to the pulmonary and systemic circulations – permanently kept entirely separate by a physical barrier.[121]
Fish

Fish have what is often described as a two-chambered heart,[127] consisting of one atrium to receive blood and one ventricle to pump it,[128] However, the fish heart has entry and exit compartments that may be called chambers, so it is also sometimes described as three-chambered[128] or four-chambered,[129] depending on what is counted as a chamber. The atrium and ventricle are sometimes considered "true chambers", while the others are considered "accessory chambers".[130]
Primitive fish have a four-chambered heart, but the chambers are arranged sequentially so that this primitive heart is quite unlike the four-chambered hearts of mammals and birds. The first chamber is the sinus venosus, which collects deoxygenated blood, from the body, through the hepatic and cardinal veins. From here, blood flows into the atrium and then to the powerful muscular ventricle where the main pumping action will take place. The fourth and final chamber is the conus arteriosus which contains several valves and sends blood to the ventral aorta. The ventral aorta delivers blood to the gills where it is oxygenated and flows, through the dorsal aorta, into the rest of the body. (In tetrapods, the ventral aorta has divided in two; one half forms the ascending aorta, while the other forms the pulmonary artery).[121]
In the adult fish, the four chambers are not arranged in a straight row but, instead form an S-shape with the latter two chambers lying above the former two. This relatively simpler pattern is found in cartilaginous fish and in the ray-finned fish. In teleosts, the conus arteriosus is very small and can more accurately be described as part of the aorta rather than of the heart proper. The conus arteriosus is not present in any amniotes, presumably having been absorbed into the ventricles over the course of evolution. Similarly, while the sinus venosus is present as a vestigial structure in some reptiles and birds, it is otherwise absorbed into the right atrium and is no longer distinguishable.[121]
Invertebrates


Arthropods and most mollusks have an open circulatory system. In this system, deoxygenated blood collects around the heart in cavities (sinuses). This blood slowly permeates the heart through many small one-way channels. The heart then pumps the blood into the hemocoel, a cavity between the organs. The heart in arthropods is typically a muscular tube that runs the length of the body, under the back and from the base of the head. Instead of blood the circulatory fluid is haemolymph which carries the most commonly used respiratory pigment, copper-based haemocyanin as the oxygen transporter; iron-based haemoglobin is used by only a few arthropods.[131]
In some other invertebrates such as earthworms, the circulatory system is not used to transport oxygen and so is much reduced, having no veins or arteries and consisting of two connected tubes. Oxygen travels by diffusion and there are five small muscular vessels that connect these vessels that contract at the front of the animals that can be thought of as "hearts".[131]
Squids and other cephalopods have two "gill hearts" also known as branchial hearts, and one "systemic heart". The brachial hearts have two atria and one ventricle each, and pump to the gills, whereas the systemic heart pumps to the body.[132][133]
Additional images
 The human heart viewed from the front
The human heart viewed from the front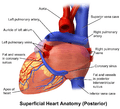 The human heart viewed from behind
The human heart viewed from behind
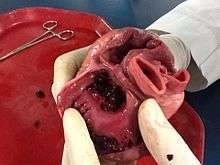
- An anatomical specimen of the heart
 Heart Illustration with circulatory system
Heart Illustration with circulatory system
Notes
- ↑ From the heart to the body
- ↑ Arteries that contain deoxygenated blood, from the heart to the lungs
- ↑ Supplying blood to the heart itself
- ↑ From the body to the heart
- ↑ Veins containing oxygenated blood from the lungs to the heart
- ↑ Veins that drain blood from the cardiac tissue itself
- ↑ Note the muscles do not cause the valves to open. The pressure difference between the blood in the atria and the ventricles does this.
- ↑ Depolarisation of the ventricles occurs concurrently, but is not significant enough to be detected on an ECG.[77]
References
This article incorporates text from the CC-BY book: OpenStax College, Anatomy & Physiology. OpenStax CNX. 30 jul 2014..
- ↑ Taber, Clarence Wilbur; Venes, Donald (2009). Taber's cyclopedic medical dictionary. F. A. Davis Co. pp. 1018–23. ISBN 0-8036-1559-0.
- ↑ Guyton & Hall 2011, p. 157.
- 1 2 3 Moore, Keith L.; Dalley, Arthur F.; Agur, Anne M. R. "1". Clinically Oriented Anatomy. Wolters Kluwel Health/Lippincott Williams & Wilkins. pp. 127–73. ISBN 978-1-60547-652-0.
- ↑ Starr, Cecie; Evers, Christine; Starr, Lisa (2 January 2009). Biology: Today and Tomorrow With Physiology. Cengage Learning. p. 422. ISBN 978-0-495-56157-6.
- 1 2 Reed, C. Roebuck; Brainerd, Lee Wherry; Lee,, Rodney; Inc, the staff of Kaplan, (2008). CSET : California Subject Examinations for Teachers (3rd ed.). New York, NY: Kaplan Pub. p. 154. ISBN 978-1-4195-5281-6.
- 1 2 Gray's Anatomy 2008, p. 960.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 Betts, J. Gordon (2013). Anatomy & physiology. pp. 787–846. ISBN 1-938168-13-5. Retrieved 11 August 2014.
- ↑ Guyton & Hall 2011, pp. 101, 157.
- 1 2 3 4 Guyton & Hall 2011, pp. 105–07.
- ↑ Guyton & Hall 2011, pp. 1039–41.
- 1 2 3 "Cardiovascular diseases (CVDs) Fact sheet N°317 March 2013". WHO. World Health Organization. Retrieved 20 September 2014.
- 1 2 3 Longo, Dan; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Jameson, J.; Loscalzo, Joseph (August 11, 2011). Harrison's Principles of Internal Medicine (18 ed.). McGraw-Hill Professional. p. 1811. ISBN 978-0-07-174889-6.
- ↑ Graham, I; Atar, D; Borch-Johnsen, K; Boysen, G; Burell, G; Cifkova, R; Dallongeville, J; De Backer, G; Ebrahim, S; Gjelsvik, B; Herrmann-Lingen, C; Hoes, A; Humphries, S; Knapton, M; Perk, J; Priori, SG; Pyorala, K; Reiner, Z; Ruilope, L; Sans-Menendez, S; Scholte op Reimer, W; Weissberg, P; Wood, D; Yarnell, J; Zamorano, JL; Walma, E; Fitzgerald, T; Cooney, MT; Dudina, A; European Society of Cardiology (ESC) Committee for Practice Guidelines, (CPG) (Oct 2007). "European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts).". European Heart Journal. 28 (19): 2375–414. PMID 17726041. doi:10.1093/eurheartj/ehm316.
- ↑ "Gray's Anatomy of the Human Body – 6. Surface Markings of the Thorax". Bartleby.com. Retrieved 2010-10-18.
- ↑ Dorland's (2012). Dorland's Illustrated Medical Dictionary (32nd ed.). Elsevier. p. 1461. ISBN 978-1-4160-6257-8.
- ↑ Bianco, Carl. "How Your Heart Works". HowStuffWorks. Retrieved 14 August 2016.
- 1 2 Gray's Anatomy 2008, pp. 960–62.
- ↑ Gray's Anatomy 2008, pp. 964–67.
- ↑ Pocock, Gillian (2006). Human Physiology. Oxford University Press. p. 264. ISBN 978-0-19-856878-0.
- 1 2 3 Gray's Anatomy 2008, pp. 966–67.
- ↑ Gray's Anatomy 2008, p. 970.
- ↑ University of Minnesota. "Papillary Muscles". Atlas of Human Cardiac Anatomy. Retrieved 7 March 2016.
- ↑ "pectinate muscle". The Free Dictionary. Retrieved 2016-07-31.
- ↑ Gray's Anatomy 2008, p. 959.
- ↑ Davidson's 2010, p. 525.
- ↑ Gray's Anatomy 2008, p. 981.
- 1 2 Gray's Anatomy 2008, p. 982.
- ↑ Davidson's 2010, p. 526.
- ↑ Gray's Anatomy 2008, p. 945.
- ↑ "Main Frame Heart Development". Meddean.luc.edu. Retrieved 2010-10-17.
- ↑ DuBose, T. J.; Cunyus, J. A.; Johnson, L. (1990). "Embryonic Heart Rate and Age". J Diagn Med Sonography. 6 (3): 151–57. doi:10.1177/875647939000600306.
- ↑ DuBose, TJ (1996) Fetal Sonography, pp. 263–74; Philadelphia: WB Saunders ISBN 0-7216-5432-0
- ↑ DuBose, Terry J. (2011-07-26) Sex, Heart Rate and Age. obgyn.net
- ↑ Guyton & Hall 2011, pp. 110–13.
- 1 2 Berry, William; McKenzie, Catherine (1 Jan 2010). "Use of inotropes in critical care". Clinical Pharmacist. 2: 395.
- 1 2 Bersten, Andrew (2013). Oh's Intensive Care Manual. (7. ed.). London: Elsevier Health Sciences. pp. 912–22. ISBN 978-0-7020-4762-6.
- ↑ Pocock, Gillian (2006). Human Physiology (Third ed.). Oxford University Press. p. 266. ISBN 978-0-19-856878-0.
- ↑ Antz, Matthias; et al. (1998). "Electrical Conduction Between the Right Atrium and the Left Atrium via the Musculature of the Coronary Sinus". Circulation. 98 (17): 1790–95. PMID 9788835. doi:10.1161/01.CIR.98.17.1790.
- ↑ De Ponti, Roberto; et al. (2002). "Electroanatomic Analysis of Sinus Impulse Propagation in Normal Human Atria". Journal of Cardiovascular Electrophysiology. 13 (1): 1–10. PMID 11843475. doi:10.1046/j.1540-8167.2002.00001.x.
- ↑ "Definition of SA node". MedicineNet.com. 27 April 2011. Retrieved 7 June 2012.
- ↑ "Purkinje Fibers". About.com. 9 April 2012. Retrieved 7 June 2012.
- ↑ Guyton & Hall 2011, pp. 115–20.
- ↑ Davis, J. P.; Tikunova, S. B. (2008). "Ca2+ exchange with troponin C and cardiac muscle dynamics". Cardiovascular Research. 77 (4): 619–26. PMID 18079104. doi:10.1093/cvr/cvm098.
- ↑ Ostchega, Y; Porter, K. S.; Hughes, J; Dillon, C. F.; Nwankwo, T (2011). "Resting pulse rate reference data for children, adolescents and adults, United States 1999–2008" (PDF). National health statistics reports (41): 1–16. PMID 21905522.
- ↑ Hall, Arthur C. Guyton, John E. (2005). Textbook of medical physiology (11th ed.). Philadelphia: W.B. Saunders. pp. 116–22. ISBN 978-0-7216-0240-0.
- ↑ Guyton & Hall 2011, p. 208.
- ↑ Guyton & Hall 2011, p. 212.
- 1 2 Talley, Nicholas J.; O'Connor, Simon. Clinical Examination. Churchill Livingstone. pp. 76–82. ISBN 978-0-7295-4198-5.
- ↑ Dorland's (2012). Dorland's Illustrated Medical Dictionary (32nd ed.). Elsevier Saunders. p. 1189. ISBN 978-1-4160-6257-8.
- ↑ Newburger, Jane (2006). Nadas' Pediatric Cardiology 2nd Edition. Philadelphia: Elsevier. p. 358. ISBN 978-1-4160-2390-6.
- ↑ Cantarini L, Lopalco G; et al. (Oct 2014). "Autoimmunity and autoinflammation as the yin and yang of idiopathic recurrent acute pericarditis". Autoimmun Rev. 14 (2): 90–97. PMID 25308531. doi:10.1016/j.autrev.2014.10.005.
- 1 2 3 "Cardiovascular diseases (CVDs)". World Health Organization. Retrieved 2016-03-09.
- ↑ "Your Heart Failure Healthcare Team". www.heart.org. Retrieved 2016-03-09.
- 1 2 3 "Different heart diseases". World Heart Federation. Retrieved 2016-03-09.
- ↑ Harrison's 2011, p. 1501.
- ↑ Davidson's 2010, p. 554.
- ↑ Davidson's 2010, p. 544.
- ↑ Davidson's 2010, pp. 543–45.
- ↑ Davidson's 2010, pp. 635–37.
- 1 2 3 Davidson's 2010, pp. 556–59.
- ↑ Davidson's 2010, pp. 556–559.
- ↑ Davidson's 2010, pp. 624–25.
- ↑ Davidson's 2010, pp. 612–13.
- 1 2 3 Davidson's 2010, pp. 560–70.
- ↑ Davidson's 2010, p. 542.
- ↑ Davidson's 2010, pp. 638–639.
- ↑ "Patent Foramen Ovale (PFO)". www.heart.org. Retrieved 2016-03-09.
- 1 2 Davidson's 2010, pp. 628–30.
- 1 2 Harrison's 2011, p. 1458–65.
- ↑ Davidson's 2010, pp. 527–34.
- ↑ Britton, the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert (2010). Davidson's principles and practice of medicine. (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. pp. 522–36. ISBN 978-0-7020-3084-0.
- 1 2 3 4 Davidson's 2010, pp. 522–36.
- ↑ Coven, David; Yang, Eric. "Acute Coronary Syndrome Workup". Medscape. Retrieved 14 August 2016.
- ↑ Davidson's 2010, pp. 531.
- ↑ Harrison's 2011, p. 1534.
- 1 2 3 4 5 6 Davidson's 2010, pp. 521–640.
- 1 2 3 4 Davidson's 2010, pp. 528–30.
- ↑ Armstrong, William F.; Ryan, Thomas; Feigenbaum, Harvey (2010). Feigenbaum's Echocardiography. Lippincott Williams & Wilkins. ISBN 978-0-7817-9557-9.
- ↑ Gheorghiade, M. (22 June 2004). "Digoxin in the Management of Cardiovascular Disorders". Circulation. 109 (24): 2959–64. PMID 15210613. doi:10.1161/01.CIR.0000132482.95686.87.
- 1 2 3 Davidson's 2010, pp. 585–88, 614–23.
- 1 2 3 "Anatomy of the Heart". University of Sydney Online Museum. Retrieved 2 August 2016.
- 1 2 3 4 Meletis, John; Konstantopoulos, Kostas (2010). "The Beliefs, Myths, and Reality Surrounding the Word Hema (Blood) from Homer to the Present". Anemia. 2010: 1–6. doi:10.1155/2010/857657.
- ↑ Katz, A. M. (1 May 2008). "The "Modern" View of Heart Failure: How Did We Get Here?". Circulation: Heart Failure. 1 (1): 63–71. doi:10.1161/CIRCHEARTFAILURE.108.772756.
- 1 2 3 4 5 6 7 Aird, W. C. (July 2011). "Discovery of the cardiovascular system: from Galen to William Harvey". Journal of Thrombosis and Haemostasis. 9: 118–29. PMID 21781247. doi:10.1111/j.1538-7836.2011.04312.x.
- ↑ Michelakis, E. D. (19 June 2014). "Pulmonary Arterial Hypertension: Yesterday, Today, Tomorrow". Circulation Research. 115 (1): 109–14. doi:10.1161/CIRCRESAHA.115.301132.
- ↑ West, John (2008). "Ibn al-Nafis, the pulmonary circulation, and the Islamic Golden Age". Journal of Applied Physiology. 105 (6): 1877–80. PMC 2612469
 . PMID 18845773. doi:10.1152/japplphysiol.91171.2008.
. PMID 18845773. doi:10.1152/japplphysiol.91171.2008. - ↑ Bondke Persson, A.; Persson, P. B. (2014). "Form and function in the vascular system". Acta Physiologica. 211 (3): 468–70. doi:10.1111/apha.12309.
- 1 2 West, J. B. (30 May 2014). "Galen and the beginnings of Western physiology". AJP: Lung Cellular and Molecular Physiology. 307 (2): L121–L128. doi:10.1152/ajplung.00123.2014.
- ↑ Silverman, M. E. (13 June 2006). "Why Does the Heart Beat?: The Discovery of the Electrical System of the Heart". Circulation. 113 (23): 2775–81. PMID 16769927. doi:10.1161/CIRCULATIONAHA.106.616771.
- ↑ Cooley, Denton A. (2011). "Recollections of the Early Years of Heart Transplantation and the Total Artificial Heart". Artificial Organs. 35 (4): 353–57. PMID 21501184. doi:10.1111/j.1525-1594.2011.01235.x.
- ↑ Miniati, Douglas N.; Robbins, Robert C. (2002). "Heart transplantation: a thirty-year perspective: A Thirty-Year Perspective". Annual Review of Medicine. 53 (1): 189–205. doi:10.1146/annurev.med.53.082901.104050.
- ↑ Neubauer, Stefan (15 March 2007). "The Failing Heart – An Engine Out of Fuel". New England Journal of Medicine. 356 (11): 1140–51. PMID 17360992. doi:10.1056/NEJMra063052.
- 1 2 3 "Heart". The Watkins Dictionary of Symbols. ISBN 978-1-78028-357-9.
- ↑ Rosner, Fred (1995). Medicine in the Bible and the Talmud : selections from classical Jewish sources (Augm. ed.). Hoboken, NJ: KTAV Pub. House. pp. 87–96. ISBN 978-0-88125-506-5.
- ↑ Britannica, Ib; Slider, Ab, Egyptian heart and soul conception. The word was also transcribed by Wallis Budge as Ab.
- ↑ Allen, James P. (2014). Middle Egyptian : an introduction to the language and culture of hieroglyphs (3rd ed.). pp. 453, 465. ISBN 978-1-107-66328-2.
- ↑ Taylor, John H. (2001). Death and the afterlife in ancient Egypt. Chicago: The University of Chicago Press. pp. 35–38. ISBN 978-0-226-79164-7.
- ↑ Xigui, Qiu; Mattos, Gilbert L (2000). Chinese writing = Wenzi-xue-gaiyao. Berkeley: Society for the Study of Early China [u.a.] p. 176. ISBN 1-55729-071-7.
- ↑ MDBG online dictionary. "心".
- ↑ Rogers, Flaws, Bob (2007). Statements of fact in traditional Chinese medicine (3rd ed.). Boulder, Colo.: Blue Poppy Press. p. 47. ISBN 978-0-936185-52-1.
- ↑ Wiseman, Nigel and Ye, Feng (1998). A practical dictionary of Chinese medicine (1st ed.). Brookline, Mass.: Paradigm Publications. p. 260. ISBN 978-0-912111-54-4.
- ↑ Sellmer, Sven (2004), "The Heart in the Ŗg veda", in Piotr Balcerowicz; Marek Mejor, Essays in Indian Philosophy, Religion and Literature, Delhi: Motilal Banarsidass Publishers, pp. 71–83, ISBN 978-81-208-1978-8
- ↑ Lanman, Charles Rockwell (1996). A Sanskrit reader : text and vocabulary and notes (repr ed.). Delhi: Motilal Banarsidass. p. 287. ISBN 978-81-208-1363-2.
- ↑ Aristotle. On the Parts of Animals. book 3, ch. 4(De partibus animalium)
- ↑ Galen, De usu partium corporis humani ("The Use of the Parts of the Human Body"), book 6.
- ↑ Sandstrom, Alan (1991) Corn is Our Blood. University of Oklahoma Press. pp. 239–40. ISBN 0-8061-2403-2.
- ↑ Kurian G (2001). "Sacred Heart of Jesus". Nelson's Dictionary of Christianity: The Authoritative Resource on the Christian World. Thomas Nelson Inc. ISBN 978-1-4185-3981-8.
- ↑ Murray, Tom Devonshire Jones; Linda Murray; Peter (2013). "Heart". The Oxford dictionary of christian art and architecture (Second ed.). Corby: Oxford University Press. ISBN 978-0-19-968027-6.
- ↑ Indonesia Magazine, 25 (1994), p. 67
- ↑ Abdennour, Samia (2010) "Firakh mahshiya wi mihammara", recipe 117, Egyptian Cooking: And Other Middle Eastern Recipes, American University in Cairo Press. ISBN 977-424-926-7.
- ↑ Kennedy, Diana (2013) My Mexico: A Culinary Odyssey with Recipes, University of Texas Press. p. 100. ISBN 0-292-74840-X.
- ↑ Sacharow, Alla (1993) Classic Russian Cuisine: A Magnificent Selection of More Than 400 Traditional Recipes. ISBN 1-55970-174-9
- ↑ Rombauer, Irma S.; Becker, Marion Rombauer; Becker, Ethan (1975). The Joy of Cooking. The Bobbs-Merrill Company. p. 508. ISBN 978-0-02-604570-4.
- ↑ Schwabe, Calvin W. (1979) Unmentionable Cuisine, University of Virginia Press, ISBN 0-8139-1162-1, p. 96
- ↑ Rombauer, Irma S. and Rombauer Becker, Marion (1975) The Joy of Cooking, p. 508
- ↑ Torode, John (2009) Beef: And Other Bovine Matters, Taunton Press, ISBN 1-60085-126-6, p. 230
- ↑ Milsom, Jennie (2009) The Connoisseur's Guide to Meat. Sterling Publishing Company. p. 171. ISBN 1-4027-7050-2
- ↑ Dobson, Geoffrey P (August 2003). "On Being the Right Size: Heart Design, Mitochondrial Efficiency and Lifespan Potential". Clinical and Experimental Pharmacology and Physiology. 30 (8): 590–97. doi:10.1046/j.1440-1681.2003.03876.x.
- ↑ Hyman, L. Henrietta (15 September 1992). Hyman's Comparative Vertebrate Anatomy. University of Chicago Press. pp. 448–. ISBN 978-0-226-87013-7.
- ↑ Shuttleworth, Trevor J., ed. (1988). Physiology of Elasmobranch Fishes. Berlin, Heidelberg: Springer Berlin Heidelberg. p. 3. ISBN 978-3-642-73336-9.
- 1 2 3 4 5 6 Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 437–42. ISBN 0-03-910284-X.
- ↑ Osborne, June (1998). The Ruby-Throated Hummingbird. University of Texas Press. p. 14. ISBN 0-292-76047-7.
- 1 2 Grimm, Kurt A.; Lamont, Leigh A.; Tranquilli, William J.; Greene, Stephen A.; Robertson, Sheilah A. (2015-03-16). Veterinary Anesthesia and Analgesia. John Wiley & Sons. p. 418. ISBN 978-1-118-52620-0.
- ↑ Colville, Thomas P.; Bassert, Joanna M. (2015-03-10). Clinical Anatomy and Physiology for Veterinary Technicians. Elsevier Health Sciences. p. 547. ISBN 978-0-323-35620-6.
- ↑ Crigg, Gordon; Johansen, Kjell (1987). "Cardiovascular Dynamics In Crocodylus Porosus Breathing Air And During Voluntary Aerobic Dives" (PDF). Journal of Comparative Physiology B. Springer-Verlag. 157 (3): 381–92. doi:10.1007/BF00693365. Archived from the original on 3 July 2012. Retrieved 3 July 2012.
- ↑ Axelsson, Michael; Craig, Franklin; Löfman, Carl; Nilsson, Stefan; Crigg, Gordon (1996). "Dynamic Anatomical Study Of Cardiac Shunting In Crocodiles Using High-Resolution Angioscopy" (PDF). The Journal of Experimental Biology. The Company of Biologists Limited. 199 (2): 359–65. PMID 9317958. Retrieved 3 July 2012.
- ↑ Jurd, Richard David (January 2004). Instant Notes Animal Biology. Garland Science. p. 134. ISBN 978-1-85996-325-8.
- 1 2 Ostrander, Gary Kent (2000). The Laboratory Fish. Elsevier. pp. 154–55. ISBN 978-0-12-529650-2.
- ↑ Farrell, Anthony P, ed. (1 June 2011). Encyclopedia of Fish Physiology: From Genome to Environment. Stevens, E Don; Cech, Jr., Joseph J; Richards, Jeffrey G. Academic Press. p. 2315. ISBN 978-0-08-092323-9.
- ↑ Shukla, J.P. Fish & Fisheries. Rastogi Publications. pp. 154–55. ISBN 978-81-7133-800-9.
- 1 2 Solomon, Eldra; Berg, Linda; Martin, Diana W. (2010-09-15). Biology. Cengage Learning. p. 939. ISBN 1-133-17032-3.
- ↑ "Meet our animals". Smithsonian National Zoological Park. Retrieved 14 August 2016.
- ↑ Ladd, Prosser C (18 March 1991). Comparative Animal Physiology, Environmental and Metabolic Animal Physiology. John Wiley & Sons. pp. 537–. ISBN 978-0-471-85767-9.
Bibliography
- Hall, John (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, Pa.: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Longo, Dan; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Jameson, J.; Loscalzo, Joseph (August 11, 2011). Harrison's Principles of Internal Medicine (18 ed.). McGraw-Hill Professional. ISBN 978-0-07-174889-6.
- Susan Standring; Neil R. Borley; et al., eds. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Nicki R. Colledge; Brian R. Walker; Stuart H. Ralston, eds. (2010). Davidson's principles and practice of medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
External links
- What Is the Heart? – NIH
- Atlas of Human Cardiac Anatomy
- Dissection review of the anatomy of the Human Heart including vessels, internal and external features
- Prenatal human heart development
- Animal hearts: fish, squid
