Hearing loss
| Hearing loss | |
|---|---|
| Synonyms | Hard of hearing; anakusis or anacusis is total deafness[1] |
 | |
| The international symbol of deafness and hearing loss | |
| Specialty | Otorhinolaryngology, audiology |
| Complications | Loneliness[2] |
| Types | Conductive, Sensorineural, mixed[3] |
| Causes | Genetics, ageing, exposure to noise, some infections, birth complications, trauma to the ear, certain medications or toxins[2] |
| Prevention | Immunization, proper care around pregnancy, avoiding loud noise, avoiding certain medications[2] |
| Treatment | Hearing aids, sign language, cochlear implants, subtitles[2] |
| Frequency | 1.33 billion / 18.5% (2015)[4] |
Hearing loss, also known as hearing impairment, is a partial or total inability to hear.[5] A deaf person has little to no hearing.[2] Hearing loss may occur in one or both ears.[2] In children hearing problems can affect the ability to learn spoken language and in adults it can cause work related difficulties.[6] In some people, particularly older people, hearing loss can result in loneliness.[2] Hearing loss can be temporary or permanent.
Hearing loss may be caused by a number of factors, including: genetics, ageing, exposure to noise, some infections, birth complications, trauma to the ear, and certain medications or toxins.[2] A common condition that results in hearing loss is chronic ear infections.[2] Certain infections during pregnancy such as syphilis and rubella may also cause hearing loss.[2] Hearing loss is diagnosed when hearing testing finds that a person is unable to hear 25 decibels in at least one ear.[2] Testing for poor hearing is recommended for all newborns.[6] Hearing loss can be categorised as mild, moderate, moderate-severe, severe, or profound.[2] There are three main types of hearing loss, conductive hearing loss, sensorineural hearing loss, and mixed hearing loss.[3]
Half of hearing loss is preventable.[2] This includes by immunization, proper care around pregnancy, avoiding loud noise, and avoiding certain medications.[2] The World Health Organization recommends that young people limit the use of personal audio players to an hour a day in an effort to limit exposure to noise.[7] Early identification and support are particularly important in children.[2] For many hearing aids, sign language, cochlear implants and subtitles are useful.[2] Lip reading is another useful skill some develop.[2] Access to hearing aids, however, is limited in many areas of the world.[2]
As of 2013 hearing loss affects about 1.1 billion people to some degree.[8] It causes disability in 5% (360 to 538 million) and moderate to severe disability in 124 million people.[2][9][10] Of those with moderate to severe disability 108 million live in low and middle income countries.[9] Of those with hearing loss it began in 65 million during childhood.[11] Those who use sign language and are members of Deaf culture see themselves as having a difference rather than an illness.[12] Most members of Deaf culture oppose attempts to cure deafness[13][14][15] and some within this community view cochlear implants with concern as they have the potential to eliminate their culture.[16] The term hearing impairment is often viewed negatively as it emphasises what people cannot do.[12]
Definition
- Hearing loss exists when there is diminished sensitivity to the sounds normally heard.[11] The terms hearing impaired or hard of hearing are usually reserved for people who have relative insensitivity to sound in the speech frequencies. The severity of a hearing loss is categorized according to the increase in volume above the usual level necessary before the listener can detect it.
- Deafness is defined as a degree of loss such that a person is unable to understand speech even in the presence of amplification.[11] In profound deafness, even the loudest sounds produced by an audiometer (an instrument used to measure hearing by producing pure tone sounds through a range of frequencies) may not be detected. In total deafness, no sounds at all, regardless of amplification or method of production, are heard.
- Speech perception - Another aspect of hearing involves the perceived clarity of a word rather than the amplitude of sound made by the word. In humans, that aspect is usually measured by tests of speech perception. These tests measure one's ability to understand speech, not to merely detect sound. There are very rare types of hearing loss which affect speech perception alone.[17]
Use of the terms "hearing impaired," "deaf-mute," or "deaf and dumb" to describe deaf and hard of hearing people is discouraged by advocacy organizations as they are offensive to many deaf and hard of hearing people.[18]
Hearing standards
Human hearing extends in frequency from 20-20,000 Hz, and in amplitude from 0 dB to 130 dB or more. 0 dB does not represent absence of sound, but rather the softest sound an average unimpaired human ear can hear; some people can hear down to -5 or even -10 dB. 130 dB represents the threshold of pain. But the ear doesn't hear all frequencies equally well; hearing sensitivity peaks around 3000 Hz. There are many qualities of human hearing besides frequency range and amplitude that can't easily be measured quantitatively. But for many practical purposes, normative hearing is defined by a frequency versus amplitude graph, or audiogram, charting sensitivity thresholds of hearing at defined frequencies. Because of the cumulative impact of age and exposure to noise and other acoustic insults, 'typical' hearing may not be normative.[19][20]
Signs and symptoms
- difficulty using the telephone
- loss of directionality of sound
- difficulty understanding speech, especially of women and children
- difficulty in speech discrimination against background noise (cocktail party effect)
- sounds or speech becoming dull, muffled or attenuated
- need for increased volume on television, radio, music and other audio sources
Hearing loss is sensory, but may have accompanying symptoms:
- pain or pressure in the ears
- a blocked feeling
There may also be accompanying secondary symptoms:
- hyperacusis, heightened sensitivity to certain volumes and frequencies of sound, sometimes resulting from "recruitment"
- tinnitus, ringing, buzzing, hissing or other sounds in the ear when no external sound is present
- vertigo and disequilibrium
- tympanophonia, abnormal hearing of one's own voice and respiratory sounds, usually as a result of a patulous eustachian tube or dehiscent superior semicircular canals
- disturbances of facial movement (indicating possible tumour or stroke)
Causes
Hearing loss has multiple causes, including ageing, genetics, perinatal problems and acquired causes like noise and disease. For some kinds of hearing loss the cause may be classified as of unknown cause.
Age
There is a progressive loss of ability to hear high frequencies with aging known as presbycusis. For men, this can start as early as 25 and women at 30. Although genetically variable it is a normal concomitant of ageing and is distinct from hearing losses caused by noise exposure, toxins or disease agents.[21] Common conditions that can increase the risk of hearing loss in elderly people are high blood pressure, diabetes or the use of certain medications harmful to the ear.[22] While everyone loses hearing with age, the amount and type of hearing loss is variable.[23]
Noise
Noise exposure is the cause of approximately half of all cases of hearing loss, causing some degree of problems in 5% of the population globally.[24] The National Institute for Occupational Safety and Health (NIOSH) recognizes that the majority of hearing loss is not due to age, but due to noise exposure. By correcting for age in assessing hearing, one tends to overestimate the hearing loss due to noise for some and underestimate it for others.[25]
Hearing loss due to noise may be temporary, called a 'temporary threshold shift', a reduced sensitivity to sound over a wide frequency range resulting from exposure to a brief but very loud noise like a gunshot, firecracker, jet engine, jackhammer, etc. or to exposure to loud sound over a few hours such as during a pop concert or nightclub session.[26] Recovery of hearing is usually within 24 hours, but may take up to a week.[27] Both constant exposure to loud sounds (85 dB(A) or above) and one-time exposure to extremely loud sounds (120 dB(A) or above) may cause permanent hearing loss.[28]
Noise-induced hearing loss (NIHL) typically manifests as elevated hearing thresholds (i.e. less sensitivity or muting) between 3000 and 6000 Hz, centered at 4000 Hz. As noise damage progresses, damage spreads to affect lower and higher frequencies. On an audiogram, the resulting configuration has a distinctive notch, called a 'noise' notch. As aging and other effects contribute to higher frequency loss (6–8 kHz on an audiogram), this notch may be obscured and entirely disappear.
Various governmental, industry and standards organizations set noise standards.[29]
The U.S. Environmental Protection Agency has identified the level of 70 dB(A) (40% louder to twice as loud as normal conversation; typical level of TV, radio, stereo; city street noise) for 24‑hour exposure as the level necessary to protect the public from hearing loss and other disruptive effects from noise, such as sleep disturbance, stress-related problems, learning detriment, etc.[30] Noise levels are typically in the 65 to 75 dB (A) range for those living near airports of freeways and may result in hearing damage if sufficient time is spent outdoors.[31]
Louder sounds cause damage in a shorter period of time. Estimation of a "safe" duration of exposure is possible using an exchange rate of 3 dB. As 3 dB represents a doubling of intensity of sound, duration of exposure must be cut in half to maintain the same energy dose. For workplace noise regulation, the "safe" daily exposure amount at 85 dB A, known as an exposure action value, is 8 hours, while the "safe" exposure at 91 dB(A) is only 2 hours.[32] Different standards use exposure action values between 80dBA and 90dBA. Note that for some people, sound may be damaging at even lower levels than 85 dB A. Exposures to other ototoxins (such as pesticides, some medications including chemotherapy agents, solvents, etc.) can lead to greater susceptibility to noise damage, as well as causing its own damage. This is called a synergistic interaction. Since noise damage is cumulative over long periods of time, persons who are exposed to non-workplace noise, like recreational activities or environmental noise, may have compounding damage from all sources.
Some national and international organizations and agencies use an exchange rate of 4 dB or 5 dB.[33] While these exchange rates may indicate a wider zone of comfort or safety, they can significantly underestimate the damage caused by loud noise. For example, at 100 dB (nightclub music level), a 3 dB exchange rate would limit exposure to 15 minutes; the 5 dB exchange rate allows an hour.
Many people are unaware of the presence of environmental sound at damaging levels, or of the level at which sound becomes harmful. Common sources of damaging noise levels include car stereos, children's toys, motor vehicles, crowds, lawn and maintenance equipment, power tools, gun use, musical instruments, and even hair dryers. Noise damage is cumulative; all sources of damage must be considered to assess risk. If one is exposed to loud sound (including music) at high levels or for extended durations (85 dB A or greater), then hearing loss will occur. Sound intensity (sound energy, or propensity to cause damage to the ears) increases dramatically with proximity according to an inverse square law: halving the distance to the sound quadruples the sound intensity.
In the USA, 12.5% of children aged 6–19 years have permanent hearing damage from excessive noise exposure.[34] The World Health Organization estimates that half of those between 12 and 35 are at risk from using personal audio devices that are too loud.[7]
Hearing loss due to noise has been described as primarily a condition of modern society.[35] In preindustrial times, humans had far less exposure to loud sounds. Studies of primitive peoples indicate that much of what has been attributed to age-related hearing loss may be long term cumulative damage from all sources, especially noise. People living in preindustrial societies have considerably less hearing loss than similar populations living in modern society. Among primitive people who have migrated into modern society, hearing loss is proportional to the number of years spent in modern society.[36][37][38] Military service in World War II, the Korean War, and the Vietnam War, has likely also caused hearing loss in large numbers of men from those generations, though proving that hearing loss was a direct result of military service is problematic without entry and exit audiograms.[39]
Hearing loss in adolescents may be caused by loud noise from toys, music by headphones, and concerts or events.[40]
Genetic
Hearing loss can be inherited. Around 75–80% of all these cases are inherited by recessive genes, 20–25% are inherited by dominant genes, 1–2% are inherited by X-linked patterns, and fewer than 1% are inherited by mitochondrial inheritance.[41]
When looking at the genetics of deafness, there are 2 different forms, syndromic and nonsyndromic. Syndromic deafness occurs when there are other signs or medical problems aside from deafness in an individual. This accounts for around 30% of deaf individuals who are deaf from a genetic standpoint.[41] Nonsyndromic deafness occurs when there are no other signs or medical problems associated with an individual other than deafness. From a genetic standpoint, this accounts for the other 70% of cases, and represents the majority of hereditary hearing loss.[41] Syndromic cases occur with diseases such as Usher syndrome, Stickler syndrome, Waardenburg syndrome, Alport's syndrome, and neurofibromatosis type 2. These are diseases that have deafness as one of the symptoms or as a common feature associated with it. Many of the genetic mutations giving rise to syndromic deafness have been identified. In nonsyndromic cases, where deafness is the only finding, it is more difficult to identify the genetic mutation although some have been discovered.
- Recent gene mapping has identified several nonsyndromic dominant (DFNA#) and recessive (DFNB#) forms of deafness. The first gene mapped for non-syndromic deafness, DFNA1, involves a splice site mutation in the formin related homolog diaphanous 1 (DIAPH1). A single base change in a large Costa Rican family was identified as causative in a rare form of low frequency onset progressive hearing loss with autosomal dominant inheritance exhibiting variable age of onset and complete penetrance by age 30.[42] The most common type of congenital hearing loss in developed countries is DFNB1, also known as connexin 26 deafness or GJB2-related deafness.
- The most common dominant syndromic forms of hearing loss include Stickler syndrome and Waardenburg syndrome.
- The most common recessive syndromic forms of hearing loss are Pendred syndrome and Usher syndrome.
- The congenital defect microtia, deformed or unformed outer ear, can be associated with partial or complete conductive deafness, depending upon the severity of the deformity and whether the middle ear is also affected. It can also be associated with abnormalities of the inner ear giving rise to an additional sensorineural component to the hearing loss (mixed deafness).
- Mutations in PTPRQ are a cause of autosomal-recessive nonsyndromic hearing loss.[43]
Perinatal problems
- Fetal alcohol spectrum disorders are reported to cause hearing loss in up to 64% of infants born to alcoholic mothers, from the ototoxic effect on the developing fetus plus malnutrition during pregnancy from the excess alcohol intake.
- Premature birth can be associated with sensorineural hearing loss because of an increased risk of hypoxia, hyperbilirubinaemia, ototoxic medication and infection as well as noise exposure in the neonatal units. The risk of hearing loss is greatest for those weighing less than 1500 g at birth.
Disorders
- strokes - Depending on what blood vessels are affected by the stroke, one of the symptoms can be deafness.
- multiple sclerosis can have an effect on hearing as well. Multiple sclerosis, or MS, is an autoimmune disease where the immune system attacks the myelin sheath, a covering that protects the nerves. If the auditory nerve becomes damaged, the affected person will become completely deaf in one or both ears. There is no cure for MS.
- perilymph fistula - a microtear in either the round or oval window (membranes separating the middle and inner ear) of the cochlea causing perilymph to leak into the middle ear. This usually occurs as a consequence of trauma, including barotrauma, and can give rise to vertigo as well as hearing loss.
- viral - viral infections of the ear can cause sensorineural hearing loss usually as the consequence of a labyrinthitis. The patient may be generally unwell at the time.
- Measles may cause auditory nerve damage but usually gives rise to a chronic middle ear problem giving rise to a mixed hearing loss.
- Mumps (Epidemic parotitis) may result in profound sensorineural hearing loss (90 dB or more), unilateral (one ear) or bilateral (both ears).
- congenital rubella (also called German measles) syndrome, can cause deafness in newborns
- several varieties of herpes viruses that cause other diseases can also infect the ear, and can result in hearing loss: congenital infection with cytomegalovirus is responsible for deafness in newborn children and also progressive sensorineural hearing loss in childhood; herpes simplex type 1, oral herpes associated with cold sores; Epstein Barr virus that causes mononucleosis; varicella zoster oticus that causes facial paralysis (Ramsay Hunt syndrome)[44]
- People with HIV/AIDS may develop hearing problems due to medications they take for the disease, the HIV virus, or due to an increased rate of other infections.[45]
- West Nile virus, which can cause a variety of neurological disorders, can also cause hearing loss by attacking the auditory nerve
- Meningitis may damage the auditory nerve or the cochlea.
- Syphilis is commonly transmitted from pregnant women to their fetuses, and about a third of infected children will eventually become deaf.
- inherited
- People with Down syndrome are more likely to have hearing loss.[46] This is usually due to middle ear effusions in childhood but towards the end of the second decade they may develop a high frequency sensorineural hearing loss which can get progressively worse with time.
- Charcot–Marie–Tooth disease variant 1E (CMT1E) is noted for demyelinating in addition to deafness.[47]
- Autoimmune disease is recognized as a cause for cochlear damage. Although rare, it is possible for autoimmune processes to target the cochlea specifically as a first presentation. Granulomatosis with polyangiitis is one of the autoimmune conditions that may precipitate hearing loss. Cogan's syndrome commonly presents with hearing loss.
- Otosclerosis is a condition that can cause fixation of the stapes (or stirrup) in the middle ear preventing its movement and causing a conductive hearing loss.
- Vestibular schwannoma, erroneously known as Acoustic neuromas, and other types of brain tumors can cause hearing loss by infringement of the tumor on the vestibulocochlear nerve
- Congenital problems
- Superior semicircular canal dehiscence, a gap in the bone cover above the inner ear, can lead to low-frequency conductive hearing loss, autophony and vertigo.
- recurring ear infections or concommitant secondary infections (such as bacterial infection subsequent to viral infection) can result in hearing loss
Medications
Some medications may reversibly affect hearing. These medications are considered ototoxic. This includes loop diuretics such as furosemide and bumetanide, non-steroidal anti-inflammatory drugs (NSAIDs) both over-the-counter (aspirin, ibuprofen, naproxen) as well as prescription (celecoxib, diclofenac, etc.), paracetamol, quinine, and macrolide antibiotics. The link between NSAIDs and hearing loss tends to be greater in women, especially those who take ibuprofen six or more times a week.[48] Others may cause permanent hearing loss.[49] The most important group is the aminoglycosides (main member gentamicin) and platinum based chemotherapeutics such as cisplatin and carboplatin.
On October 18, 2007, the U.S. Food and Drug Administration (FDA) announced that a warning about possible sudden hearing loss would be added to drug labels of PDE5 inhibitors, which are used for erectile dysfunction.[50]
Chemicals
In addition to medications, hearing loss can also result from specific chemicals: metals, such as lead; solvents, such as toluene (found in crude oil, gasoline[51] and automobile exhaust,[51] for example); and asphyxiants.[52] Combined with noise, these ototoxic chemicals have an additive effect on a person’s hearing loss.[52]
Hearing loss due to chemicals starts in the high frequency range and is irreversible. It damages the cochlea with lesions and degrades central portions of the auditory system.[52] For some ototoxic chemical exposures, particularly styrene,[53] the risk of hearing loss can be higher than being exposed to noise alone.
- Solvents
- Asphyxiants
- Heavy metals
- lead, mercury, cadmium, arsenic, tin-hydrocarbon compounds (trimethyltin)
- Pesticides and herbicides - The evidence is weak regarding association between herbicides and hearing loss; hearing loss in such circumstances may be due to concommitant exposure to insecticides.
Physical trauma
There can be damage either to the ear itself or to the brain centers that process the aural information conveyed by the ears. People who sustain head injury are especially vulnerable to hearing loss or tinnitus, either temporary or permanent.[55][56]
Pathophysiology
From a neurobiological perspective, there are three reasons that could cause a person to have hearing loss: either there is something wrong with the mechanical portion of the process, meaning the conductive portions of the ear (external and middle ear), or there is something wrong with the sensory portion of the process (inner ear or cochlea and related structures) or there is something wrong with the neural portion of the process, meaning the nerves or brain.
The process of understanding how sound travels to the brain is imperative in understanding how and why disease can cause a person to develop hearing loss. The process is as follows: sound waves are transmitted to the outer ear, sound waves are conducted down to ear canal, bringing the sound waves to the eardrum which they cause to vibrate, these vibrations are now passed through the 3 tiny ear bones in the middle ear, which transfer the vibrations to the fluid in the inner ear, the fluid moves the hair cells, the movement of the hair cells cause the vibrations to be converted into nerve impulses, the nerve impulses are taken to the brain by the auditory nerve,[57] the auditory nerve takes the impulses to the medulla oblongata, the brainstem send the impulses to the midbrain, which finally goes to the auditory cortex of the temporal lobe to be interpreted as sound.[58]
This process is complex and involves several steps that depend on the previous step in order for the vibrations or nerve impulses to be passed on. This is why if anything goes wrong at either the mechanical or neural portion of the process, it could result in sound not being processed by the brain, hence, leading to hearing loss.
Lesions to the auditory association cortex produced by physical trauma can result in deafness and other problems in auditory perception. The place where the lesion occurs on the auditory cortex plays an important role in what type of hearing deficit will occur in a person. A study conducted by Clarke et al. (2000) tested three subjects for the ability to identify a produced environmental sound, the source of the sound, and whether or not the source is moving. All three subjects had trauma to different parts of the auditory cortex, and each patient demonstrated a different set of auditory deficits, suggesting that different parts of the auditory cortex controlled different parts of the hearing process.[59] This means, lesion one part of auditory cortex and it could result in one or two deficits. It would take larger lesions at the right parts to produce deafness.
Diagnosis
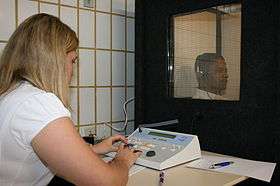
Identification of a hearing loss is usually conducted by a general practitioner medical doctor, otolaryngologist, certified and licensed audiologist, school or industrial audiometrist, or other audiology technician. Diagnosis of the cause of a hearing loss is carried out by a specialist physician (audiovestibular physician) or otorhinolaryngologist.
Case history
A case history (usually a written form, with questionnaire) can provide valuable information about the context of the hearing loss, and indicate what kind of diagnostic procedures to employ. Case history will include such items as:
- major concern
- birth and pregnancy information
- medical history
- development history
- family history
- workplace environment
- home environment
Examination
- otoscopy, visual examination of the outer ear, ear canal, eardrum, and middle ear (through the translucent eardrum) using an optical instrument inserted into the ear canal called an otoscope
- tympanometry
- differential testing - the Weber, Rinne, Bing and Schwabach tests are simple manual tests of auditory function conducted with a low frequency (usually 512 Hz) tuning fork that can provide a quick indication of type of hearing loss: unilateral/bilateral, conductive, or other
Laboratory testing
In case of infection or inflammation, blood or other body fluids may be submitted for laboratory analysis.
Hearing tests
Hearing loss is generally measured by playing generated or recorded sounds, and determining whether the person can hear them. Hearing sensitivity varies according to the frequency of sounds. To take this into account, hearing sensitivity can be measured for a range of frequencies and plotted on an audiogram.
Another method for quantifying hearing loss is a speech-in-noise test. As the name implies, a speech-in-noise test gives an indication of how well one can understand speech in a noisy environment. A person with a hearing loss will often be less able to understand speech, especially in noisy conditions. This is especially true for people who have a sensorineural loss – which is by far the most common type of hearing loss. As such, speech-in-noise tests can provide valuable information about a person's hearing ability, and can be used to detect the presence of a sensorineural hearing loss. A recently developed digit-triple speech-in-noise test may be a more efficient screening test.[60]
Otoacoustic emissions test is an objective hearing test that may be administered to toddlers and children too young to cooperate in a conventional hearing test. The test is also useful in older children and adults.
Auditory brainstem response testing is an electrophysiological test used to test for hearing deficits caused by pathology within the ear, the cochlear nerve and also within the brainstem. This test can be used to identify delay in the conduction of neural impulses due to tumours or inflammation but can also be an objective test of hearing thresholds. Other electophysiological tests, such as cortical evoked responses, can look at the hearing pathway up to the level of the auditory cortex.
Scans
MRI and CT scans can be useful to identify the pathology of many causes of hearing loss. They are only needed in selected cases.
Classification
Hearing loss is categorized by type, severity, and configuration. Furthermore, a hearing loss may exist in only one ear (unilateral) or in both ears (bilateral). Hearing loss can be temporary or permanent, sudden or progressive.
Severity
The severity of a hearing loss is ranked according to ranges of nominal thresholds in which a sound must be so it can be detected by an individual. It is measured in decibels of hearing loss, or dB HL. The measurement of hearing loss in an individual is conducted over several frequencies, mostly 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz. The hearing loss of the individual is the average of the hearing loss values over the different frequencies. Hearing loss can be ranked differently according to different organisations; and so, in different countries are different systems in use.
Hearing loss may be ranked as slight, mild, moderate, moderately severe, severe or profound as defined below:
- Slight: between 16 and 25 dB HL
- Mild:
- for adults: between 26 and 40 dB HL
- for children: between 20 and 40 dB HL[11]
- Moderate: between 41 and 54 dB HL[11]
- Moderately severe: between 55 and 70 dB HL[11]
- Severe: between 71 and 90 dB HL[11]
- Profound: 91 dB HL or greater[11]
- Totally deaf: Have no hearing at all. This is called anacusis.
The 'Audiometric Classifications of Hearing Impairment' according to the International Bureau Audiophonology (BIAP) in Belgium is as follows:[61]
- Normal or subnormal hearing: average tone loss is below 20 dB HL
- Mild hearing loss: average tone loss between 21 and 40 dB HL
- Moderate hearing loss
- First degree: average tone loss between 41 and 55 dB HL
- Second degree: average tone loss between 56 and 70 dB HL
- Severe hearing loss
- First degree: average tone loss between 71 and 80 dB HL
- Second degree: average tone loss between 81 and 90 dB HL
- Very severe hearing loss
- First degree: average tone loss between 91 and 100 dB HL
- Second degree: average tone loss between 101 and 110 dB HL
- Third degree: average tone loss between 111 and 119 dB HL
- Total hearing loss or Cophosis: average tone loss is more than 120 dB HL
Hearing loss may affect one or both ears. If both ears are affected, then one ear may be more affected than the other. Thus it is possible, for example, to have normal hearing in one ear and none at all in the other, or to have mild hearing loss in one ear and moderate hearing loss in the other.
For certain legal purposes such as insurance claims, hearing loss is described in terms of percentages. Given that hearing loss can vary by frequency and that audiograms are plotted with a logarithmic scale, the idea of a percentage of hearing loss is somewhat arbitrary, but where decibels of loss are converted via a legally recognized formula, it is possible to calculate a standardized "percentage of hearing loss", which is suitable for legal purposes only.
Type
There are four main types of hearing loss, conductive hearing loss, sensorineural hearing loss, central deafness and combinations of conductive and sensorienural hearing losses which is called mixed hearing loss.[11] An additional problem which is increasingly recognised is auditory processing disorder which is not a hearing loss as such but a difficulty perceiving sound.
- Conductive hearing loss
Conductive hearing loss is present when the sound is not reaching the inner ear, the cochlea. This can be due to external ear canal malformation, dysfunction of the eardrum or malfunction of the bones of the middle ear. The ear drum may show defects from small to total resulting in hearing loss of different degree. Scar tissue after ear infections may also make the ear drum dysfunction as well as when it is retracted and adherent to the medial part of the middle ear.
Dysfunction of the three small bones of the middle ear – malleus, incus, and stapes – may cause conductive hearing loss. The mobility of the ossicles may be impaired for different reasons and disruption of the ossicular chain due to trauma, infection or ankylosis may also cause hearing loss.
- Sensorineural hearing loss
Sensorineural hearing loss is one caused by dysfunction of the inner ear, the cochlea or the nerve that transmits the impulses from the cochlea to the hearing centre in the brain. The most common reason for sensorineural hearing loss is damage to the hair cells in the cochlea. Depending on the definition it could be estimated that more than 50% of the population over the age of 70 has impaired hearing.[62]
- Central deafness
Damage to the brain can lead to a central deafness. The peripheral ear and the auditory nerve may function well but the central connections are damaged by tumour, trauma or other disease and the patient is unable to hear.
- Mixed hearing loss
Mixed hearing loss is a combination of conductive and sensorineural hearing loss. Chronic ear infection (a fairly common diagnosis) can cause a defective ear drum or middle-ear ossicle damages, or both. In addition to the conductive loss, a sensory component may be present.
- Central auditory processing disorder
This is not an actual hearing loss but gives rise to significant difficulties in hearing. One kind of auditory processing disorder is King-Kopetzky syndrome, which is characterized by an inability to process out background noise in noisy environments despite normal performance on traditional hearing tests.
Configuration
The shape of an audiogram shows the relative configuration of the hearing loss, such as a Carhart notch for otosclerosis, 'noise' notch for noise-induced damage, high frequency rolloff for presbycusis, or a flat audiogram for conductive hearing loss. In conjunction with speech audiometry, it may indicate central auditory processing disorder, or the presence of a schwannoma or other tumor. There are four general configurations of hearing loss:
1. Flat: thresholds essentially equal across test frequencies.
2. Sloping: lower (better) thresholds in low-frequency regions and higher (poorer) thresholds in high-frequency regions.
3. Rising: higher (poorer) thresholds in low-frequency regions and lower (better) thresholds in higher-frequency regions.
4. Trough-shaped ("cookie-bite" or "U" shaped): greatest hearing loss in the mid-frequency range, with lower (better) thresholds in low- and high-frequency regions.
Unilateral and bilateral
People with unilateral hearing loss or single-sided deafness (SSD) have difficulty in:
- hearing conversation on their impaired side
- localizing sound
- understanding speech in the presence of background noise.
In quiet conditions, speech discrimination is approximately the same for normal hearing and those with unilateral deafness; however, in noisy environments speech discrimination varies individually and ranges from mild to severe.
One reason for the hearing problems these patients often experience is due to the head shadow effect. Newborn children with no hearing on one side but one normal ear could still have problems.[63] Speech development could be delayed and difficulties to concentrate in school are common. More children with unilateral hearing loss have to repeat classes than their peers. Taking part in social activities could be a problem. Early aiding is therefore of utmost importance.[64][65]
Prevention
It is estimated that half of cases of hearing loss are preventable.[66] A number of preventative strategies are effective including: immunisation against rubella to prevent congenital rubella syndrome, immunization against H. influenza and S. pneumoniae to reduce cases of meningitis, and avoiding or protecting against excessive noise exposure.[11] The World Health Organization also recommends immunization against measles, mumps, and meningitis, efforts to prevent premature birth, and avoidance of certain medication as prevention.[67]
Noise exposure is the most significant risk factor for noise-induced hearing loss that can be prevented. Different programs exist for specific populations such as school-age children, adolescents and workers.[68] Education regarding noise exposure increases the use of hearing protectors.[69] The use of antioxidants is being studied for the prevention of noise-induced hearing loss, particularly for scenarios in which noise exposure cannot be reduced, such as during military operations.[70]
Workplace noise regulation
Noise is widely recognized as an occupational hazard. In the United States, the National Institute for Occupational Safety and Health (NIOSH) and the Occupational Safety and Health Administration (OSHA) work together to provide standards and enforcement on workplace noise levels.[71][72] The hierarchy of hazard controls demonstrates the different levels of controls to reduce or eliminate exposure to noise and prevent hearing loss, including engineering controls and personal protective equipment (PPE).[73] Other programs and initiative have been created to prevent hearing loss in the workplace. For example, the Safe-in-Sound Award was created to recognize organizations with successful noise control implementations.[74] Additionally, the Buy Quiet program was created to encourage employers to purchase quieter machinery and tools.[75] By purchasing less noisy power tools like those found on the NIOSH Power Tools Database and limiting exposure to ototoxic chemicals, great strides can be made in preventing hearing loss.[76]
Companies can also provide personal hearing protector devices tailored to both the worker and type of employment. Some hearing protectors universally block out all noise, and some allow for certain noises to be heard. Workers are more likely to wear hearing protector devices when they are properly fitted.[77]
Better enforcement of laws can decrease levels of noise at work.[78]
Screening
The United States Preventive Services Task Force recommends screening for all newborns.[6]
The American Academy of Pediatrics advises that children should have their hearing tested several times throughout their schooling:[34]
- When they enter school
- At ages 6, 8, and 10
- At least once during middle school
- At least once during high school
While the American College of Physicians indicated that there is not enough evidence to determine the utility of screening in adults over 50 years old who do not have any symptoms,[79] the American Language, Speech Pathology and Hearing Association recommends that adults should be screened at least every decade through age 50 and at 3-year intervals thereafter, to minimize the detrimental effects of the untreated condition on quality of life.[80] For the same reason, the US Office of Disease Prevention and Health Promotion included as one of Healthy People 2020 objectives: to increase the proportion of persons who have had a hearing examination.[81]
Treatment
Treatment depends on the specific cause if known as well as the extent, type and configuration of the hearing loss. Most hearing loss, that resulting from age and noise, is progressive and irreversible, and there are currently no approved or recommended treatments; management is by hearing aid. A few specific kinds of hearing loss are amenable to surgical treatment. In other cases, treatment is addressed to underlying pathologies, but any hearing loss incurred may be permanent.
There are a number of devices that can improve hearing in those who are deaf or hard of hearing or allow people with these conditions to manage better in their lives.
Hearing aids
Hearing aids are devices that work to improve the hearing and speech comprehension of those with hearing loss.[82] It works by magnifying the sound vibrations in the ear so that one can understand what is being said around them.[82] The use of this technological device may or may not have an effect on one's sociability. Some people feel as if they cannot live without one because they say it is the only thing that keeps them engaged with the public. Conversely, there are many people who choose not to wear their hearing aids for a multitude of reasons. The vast majority of these reasons stem from either poor performance of the aid, in which the user notices more amplification of background noises instead of the sounds they intended, or from issues with comfort, care, or maintenance of the device; financial factors have also been reported.[83] A comparatively small fraction of people choose not to wear hearing aids due to aesthetic concerns and/or stigma around wearing the device.[83]
Assistive devices
Many deaf and hard of hearing individuals use assistive devices in their daily lives:
- Individuals can communicate by telephone using telephone typewriters (TTY). Other common names are textphone, minicom and telecommunications device for the deaf (TDD). These devices look like typewriters or word processors and transmit typed text over regular telephone lines. This allows communication through visual messaging. TTYs can transmit messages to individuals who don’t have TTY by using the National Relay service which is an operator that acts as a messenger to each caller.[84] For mobile phones, software apps are available to provide TDD/textphone functionality on some carriers/models to provide 2-way communications.
- There are several new telecommunications relay service technologies including IP Relay and captioned telephone technologies. A deaf or hard of hearing person can communicate over the phone with a hearing person via a human translator. Phone captioning is a service in which a hearing person's speech is captioned by a third party, enabling a deaf or hard of hearing person to conduct a conversation with a hearing person over the phone.[85] Wireless, Internet and mobile phone/SMS text messaging are beginning to take over the role of the TDD.
- Real-time text technologies, involving streaming text that is continuously transmitted as it is typed or otherwise composed. This allows conversational use of text. Software programs are now available that automatically generate a closed-captioning of conversations. Examples include discussions in conference rooms, teleconference calls, classroom lectures, and/or religious services.
- Instant messaging software.
- Videophones and similar video technologies can be used for distance communication using sign language. Video conferencing technologies permit signed conversations as well as permitting a sign language–English interpreter to voice and sign conversations between a deaf or hard of hearing person and that person's hearing party, negating the use of a TTY device or computer keyboard.
- Video relay service and video remote interpreting (VRI) services also use a third-party telecommunication service to allow a deaf or hard-of-hearing person to communicate quickly and conveniently with a hearing person, through a sign language interpreter.
- Hearing dogs are a specific type of assistance dog specifically selected and trained to assist the deaf and hard of hearing by alerting their handler to important sounds, such as doorbells, smoke alarms, ringing telephones, or alarm clocks.
- The advent of the Internet's World Wide Web and closed captioning has given the deaf and hard of hearing unprecedented access to information. Electronic mail and online chat have reduced the need for deaf and hard-of-hearing people to use a third-party Telecommunications Relay Service to communicate with the hearing and other deaf people.
- A person with hearing loss cannot always hear the phone or distinguish their own ringtone from another. A signalling transmitter can be attached to a phone that will cause a light or a vibration device to activate. Transmitters can also be used to activate visuals cues to represent fire alarms.[84]
- Individuals with hearing loss require phones with amplifiers that have a higher power of amplification when compared to a regular phone. The Hearing Aid Telephone Interconnect System is a hands free amplification system which allows people to amplify sound when using telephones, cell phones, computer and pay phones by way of the attachment of a portable unit.[84]
Wireless hearing aids
A wireless device has two main components: a transmitter and a receiver. The transmitter broadcasts the captured sound, and the receiver detects the broadcast audio and enables the incoming audio stream to be connected to accommodations such as hearing aids or captioning systems.
Three types of wireless systems are commonly used: FM, audio induction loop, and InfraRed. Each system has advantages and benefits for particular uses. FM systems can be battery operated or plugged into an electrical outlet. FM system produce an analog audio signal, meaning they have extremely high fidelity. Many FM systems are very small in size, allowing them to be used in mobile situations. The audio induction loop permits the listener with hearing loss to be free of wearing a receiver provided that the listener has a hearing aid or cochlear implant processor with an accessory called a "telecoil". If the listener does not have a telecoil, then he or she must carry a receiver with an earpiece. As with FM systems, the infrared (IR) system also requires a receiver to be worn or carried by the listener. An advantage of IR wireless systems is that people in adjoining rooms cannot listen in on conversations, making it useful for situations where privacy and confidentiality are required. Another way to achieve confidentiality is to use a hardwired amplifier, which contains or is connected to a microphone and transmits no signal beyond the earpiece plugged directly into it.[86]
Surgical

There is no treatment surgical or otherwise for hearing lost due to the most common causes (age, noise and genetic defects). For a few specific conditions, surgical intervention can provide a remedy:
- surgical correction of superior canal dehiscence
- myringotomy, surgical insertion of drainage ventilation tubes in the tympanic membrane. Such placement is usually temporary until the underlying pathology (infection or other inflammation) can be resolved.
- radiotherapy or surgical excision of vestibular schwannoma or acoustic neuroma, though, in most cases, it is unlikely that hearing will be preserved
- Stapedectomy and stapedotomy for otosclerosis - replacement or reshaping of the stapes bone of the middle ear can restore hearing in cases of conductive hearing loss
Surgical and implantable hearing aids are an alternative to conventional external hearing aids. If the ear is dry and not infected, an air conduction aid could be tried; if the ear is draining, a direct bone condition hearing aid is often the best solution. If the conductive part of the hearing loss is more than 30–35 dB, an air conduction device could have problems overcoming this gap. A bone-anchored hearing aid could, in this situation, be a good option. The active bone conduction hearing implant Bonebridge is also an option. This implant is invisible under the intact skin and therefore minimises the risk of skin irritations.[65]
Cochlear implants improve outcomes in people with hearing loss in either one or both ears.[87] They work by artificial stimulation of the cochlear nerve by providing an electric impulse substitution for the firing of hair cells. They are expensive, and require programming along with extensive training for effectiveness.
Cochlear implants as well as bone conduction implants can help with single sided deafness. Middle ear implants or bone conduction implants can help with conductive hearing loss.[65]
People with cochlear implants are at a higher risk for bacterial meningitis. Thus, meningitis vaccination is recommended.[88] People who have hearing loss, especially those who develop a hearing problem in childhood or old age, may need support and technical adaptations as part of the rehabilitation process. Recent research shows variations in efficacy but some studies[89] show that if implanted at a very young age, some profoundly impaired children can acquire effective hearing and speech, particularly if supported by appropriate rehabilitation.
Classroom
For a classroom setting, children with hearing loss often benefit from direct instruction and communication. One option for students is to attend a school for the Deaf, where they will have access to the language, communication, and education. Another option is to have the child attend a mainstream program, with special accommodation such as providing favorable seating for the child. Having the student sit as close to the teacher as possible improves the student's ability to hear the teacher's voice and to more easily read the teacher's lips. When lecturing, teachers can help the student by facing them and by limiting unnecessary noise in the classroom. In particular, the teacher can avoid talking when their back is turned to the classroom, such as while writing on a whiteboard.
Some other approaches for classroom accommodations include pairing deaf or hard of hearing students with hearing students. This allows the deaf or hard of hearing student to ask the hearing student questions about concepts that they have not understood. The use of CART (Communication Access Real Time) systems, where an individual types a captioning of what the teacher is saying, is also beneficial.[90] The student views this captioning on their computer. Automated captioning systems are also becoming a popular option.[91] In an automated system, software, instead of a person, is used to generate the captioning. Unlike CART systems, automated systems generally do not require an Internet connection and thus they can be used anywhere and anytime. Another advantage of automated systems over CART is that they are much lower in cost. However, automated systems are generally designed to only transcribe what the teacher is saying and to not transcribe what other students say. An automated system works best for situations where just the teacher is speaking, whereas a CART system will be preferred for situations where there is a lot of classroom discussion.
For those students who are completely deaf, one of the most common interventions is having the child communicate with others through an interpreter using sign language.[92]
Epidemiology
_world_map_-_DALY_-_WHO2004.svg.png)
|
no data
<250
250–295
295–340
340–385
385–430
430–475
|
475–520
520–565
565–610
610–655
655–700
>700
|
Globally, hearing loss affects about 10% of the population to some degree.[24] It caused moderate to severe disability in 124.2 million people as of 2004 (107.9 million of whom are in low and middle income countries).[9] Of these 65 million acquired the condition during childhood.[11] At birth ~3 per 1000 in developed countries and more than 6 per 1000 in developing countries have hearing problems.[11]
Hearing loss increases with age. In those between 20 and 35 rates of hearing loss are 3% while in those 44 to 55 it is 11% and in those 65 to 85 it is 43%.[6]
United States
Data from the United States in 2011-2012 found that rates of hearing loss has declined among adults aged 20 to 69 years, when compared with the results from an earlier time period (1999-2004). It also found that adult hearing loss is associated with increasing age, sex, race/ethnicity, educational level, and noise exposure.[93]
Nearly one in four adults had audiometric results suggesting noise-induced hearing loss. Almost one in four adults who reported excellent or good hearing had a similar pattern (5.5% on both sides and 18% on one side). Among people who reported exposure to loud noise at work, almost one third had such changes.[94]
History
Abbé Charles-Michel de l'Épée opened the first school for the deaf in Paris at the deaf school. The American Thomas Gallaudet witnessed a demonstration of deaf teaching skills from Épée's successor Abbé Sicard and two of the school's deaf faculty members, Laurent Clerc and Jean Massieu; accompanied by Clerc, he returned to the United States, where in 1817 they founded American School for the Deaf in Hartford, Connecticut. American Sign Language (ASL) started to evolve from primarily French Sign Language (LSF), and other outside influences.[95]
Society and culture
After language
Post-lingual deafness is hearing loss that is sustained after the acquisition of language, which can occur due to disease, trauma, or as a side-effect of a medicine. Typically, hearing loss is gradual and often detected by family and friends of affected individuals long before the patients themselves will acknowledge the disability. Post-lingual deafness is far more common than pre-lingual deafness. Those who lose their hearing later in life, such as in late adolescence or adulthood, face their own challenges, living with the adaptations that allow them to live independently.
Before language
Prelingual deafness is hearing loss that is sustained before the acquisition of language, which can occur due to a congenital condition or through hearing loss in early infancy. Prelingual deafness impairs an individual's ability to acquire a spoken language. Children born into signing families rarely have delays in language development, but most prelingual hearing loss is acquired via either disease or trauma rather than genetically inherited, so families with deaf children nearly always lack previous experience with sign language. Cochlear implants allow prelingually deaf children to acquire an oral language with remarkable success if implantation is performed within the first 2–4 years.[96]
Jack Gannon, a professor at Gallaudet University, said this about Deaf culture. "Deaf culture is a set of learned behaviors and perceptions that shape the values and norms of deaf people based on their shared or common experiences." Some doctors believe that being deaf makes a person more social. Bill Vicar, from ASL University, shared his experiences as a deaf person, "[deaf people] tend to congregate around the kitchen table rather than the living room sofa… our good-byes take nearly forever, and our hellos often consist of serious hugs. When two of us meet for the first time we tend to exchange detailed biographies."[97] Deaf culture is not about contemplating what deaf people cannot do and how to fix their problems, an approach known as the "pathological view of the deaf."[98] Instead deaf people celebrate what they can do. There is a strong sense of unity between deaf people as they share their experiences of suffering through a similar struggle. This celebration creates a unity between even deaf strangers. Bill Vicars expresses the power of this bond when stating, "if given the chance to become hearing most [deaf people] would choose to remain deaf."[99]
Views of treatments
There has been considerable controversy within the culturally deaf community over cochlear implants. For the most part, there is little objection to those who lost their hearing later in life, or culturally deaf adults choosing to be fitted with a cochlear implant.[16]
Many in the deaf community strongly object to a deaf child being fitted with a cochlear implant (often on the advice of an audiologist); new parents may not have sufficient information on raising deaf children and placed in an oral-only program that emphasizes the ability to speak and listen over other forms of communication such as sign language or total communication. Many Deaf people view cochlear implants and other hearing devices as confusing to one's identity. A Deaf person will never be a hearing person and therefore would be trying to fit into a way of living that is not their own. Other concerns include loss of Deaf culture and identity and limitations on hearing restoration.[16]
The U.S. National Association of the Deaf has a statement on its website regarding cochlear implants.[100] The NAD asserts that the choice to implant is up to the individual (or the parents), yet strongly advocates a fully informed decision in all aspects of a cochlear implant. Much of the negative reaction to cochlear implants stems from the medical viewpoint that deafness is a condition that needs to be "cured," while the Deaf community instead regards deafness a defining cultural characteristic.
Many other assistive devices are more acceptable to the Deaf community, including but not limited to, hearing aids, closed captioning, email and the Internet, text telephones, and video relay services.
Sign language
Sign languages convey meaning through manual communication and body language instead of acoustically conveyed sound patterns. This involves the simultaneous combination of hand shapes, orientation and movement of the hands, arms or body, and facial expressions to express a speaker's thoughts. "Sign languages are based on the idea that vision is the most useful tool a deaf person has to communicate and receive information".[101]
Government policies
Those who are deaf (by either state or federal standards) have access to a free and appropriate public education. If a child does qualify as being deaf or hard of hearing and receives an individualized education plan, the IEP team must consider, "the child's language and communication needs. The IEP must include opportunities for direct communication with peers and professionals. It must also include the student’s academic level, and finally must include the students full range of needs"[102][103]
In part, the Department of Education defines deafness as "… a hearing impairment that is so severe that the child is impaired in processing linguistic information through hearing, with or without amplification …." Hearing impairment is defined as "… an impairment in hearing, whether permanent or fluctuating, that adversely affects a child's educational performance but that is not included under the definition of deafness …."[104]
Inclusion versus pullout

It is commonly misunderstood that least restrictive environment means mainstreaming or inclusion. Sometimes the resources available at the public schools do not match up to the resources at a residential school for the deaf. Many hearing parents choose to have their deaf child educated in the general education classroom as much as possible because they are told that mainstreaming is the least restrictive environment, which is not always the case. However, there are parents that live in Deaf communities who feel that the general education classroom is not the least restrictive environment for their child. These parents feel that placing their child in a residential school where all children are deaf may be more appropriate for their child because the staff tend to be more aware of the needs and struggles of deaf children. Another reason that these parents feel a residential school may be more appropriate is because in a general education classroom, the student will not be able to communicate with their classmates due to the language barrier.
In a residential school where all the children use the same communication system (whether it is a school using ASL, Total Communication or Oralism), students will be able to interact normally with other students, without having to worry about being criticized. An argument supporting inclusion, on the other hand, exposes the student to people who are not just like them, preparing them for adult life. Through interacting, children with hearing disabilities can expose themselves to other cultures which in the future may be beneficial for them when it comes to finding jobs and living on their own in a society where their disability may put them in the minority. These are some reasons why a person may or may not want to put their child in an inclusion classroom.[103]
Communication barriers
The most predominant forms of communication barriers originate from one's own personal self and they are directly the result of the hearing loss condition. These barriers are associated specifically with speech and language. In terms of speech, hearing loss has an effect on speech sound production, for example distortion caused by the omission of various letters from words. The pitch of their voice may sound too high or low and their volume may be louder or quieter than is intended. Resonance of voice is also affected, as it can be hypernasal or denasal. Prosody, which represents the patterns of stress and rhythm in the voice, will often become irregular. As a result of such changes to speech, the receiver during a conversation is likely to deem the communicator's speech unintelligible. The placement of improper stresses on syllables makes it more difficult for the receiver to clearly perceive and hear the intended words. Three major problems in terms of language are present for those with hearing loss. First, there are problems with language formation, where individuals may overuse nouns and verbs and they may improperly place words within a sentence. Second, the actual content of the language is troubling, for example the interpretation of synonyms and antonyms. This results in a limited vocabulary. The third major problem is associated with Pragmatics, which includes the inability of individuals to recognize that a message has been delivered to them, therefore resulting in inappropriate questions being asked. All of these speech and language barriers make it difficult for those with hearing loss to control their own speech and understand what others have to say, therefore making it quite hard to hold a conversation altogether.[105]
Family
The communication limitations between people who are deaf and their hearing family members can often cause difficulties in family relationships, and affect the strength of relationships among individual family members. It was found that most people who are deaf have hearing parents, which means that the channel that the child and parents communicate through can be very different, often affecting their relationship in a negative way. If a parent communicates best verbally, and their child communicates best using sign language, this could result in ineffective communication between parents and children. Ineffective communication can potentially lead to fights caused by misunderstanding, less willingness to talk about life events and issues, and an overall weaker relationship. Even if individuals in the family made an effort to learn deaf communication techniques such as sign language, a deaf family member often will feel excluded from casual banter; such as the exchange of daily events and news at the dinner table. It is often difficult for people who are deaf to follow these conversations due to the fast paced and overlapping nature of these exchanges. This can cause a deaf individual to become frustrated and take part in less family conversations. This can potentially result in weaker relationships between the hearing individual and their immediate family members. This communication barrier can have a particularly negative effect on relationships with extended family members as well. Communication between a deaf individual and their extended family members can be very difficult due to the gap in verbal and non-verbal communication. This can cause the individuals to feel frustrated and unwilling to put effort into communicating effectively. The lack of effort put into communicating can result in anger, miscommunication, and unwillingness to build a strong relationship.[106]
Community
People who have hearing loss can often experience many difficulties as a result of communication barriers among them and other hearing individuals in the community. Some major areas that can be impacted by this are involvement in extracurricular activities and social relationships. For young people, extracurricular activities are vehicles for physical, emotional, social, and intellectual development. However, it is often the case that communication barriers between people who are deaf and their hearing peers and coaches/club advisors limit them from getting involved. These communication barriers make it difficult for someone with a hearing loss to understand directions, take advice, collaborate, and form bonding relationships with other team or club members. As a result, extracurricular activities such as sports teams, clubs, and volunteering are often not as enjoyable and beneficial for individuals who have hearing loss, and they may engage in them less often. A lack of community involvement through extracurricular activities may also limit the individual’s social network. In general, it can be difficult for someone who is deaf to develop and maintain friendships with their hearing peers due to the communication gap that they experience. They can often miss the jokes, informal banter, and "messing around" that is associated with the formation of many friendships among young people. Conversations between people who are deaf and their hearing peers can often be limited and short due to their differences in communication methods and lack of knowledge on how to overcome these differences. Deaf individuals can often experience rejection by hearing peers who are not willing to make an effort to find their way around communication difficulties. Patience and motivation to overcome such communication barriers is required by both the deaf or hard of hearing and hearing individuals in order to establish and maintain good friendships.[106]
Many people tend to forget about the difficulties that deaf children encounter, as they view the deaf child differently from a deaf adult. Deaf children grow up being unable to fully communicate with their parents, siblings and other family members. Examples include being unable to tell their family what they have learned, what they did, asking for help, or even simply being unable to interact in daily conversation. Deaf children have to learn sign language and to read lips at a young age, however they cannot communicate with others using it unless the others are educated in sign language as well. Children who are deaf or hard of hearing are faced with many complications while growing up, for example some children have to wear hearing aids and others require assistance from sign language (ASL) interpreters. The interpreters help them to communicate with other individuals until they develop the skills they need to efficiently communicate on their own. Although growing up for deaf children may entitle more difficulties than for other children, there are many support groups that allow deaf children to interact with other children. This is where they develop friendships. There are also classes for young children to learn sign language in an environment that has other children in their same situation and around their same age. These groups and classes can be very beneficial in providing the child with the proper knowledge and not to mention the societal interactions that they need in order to live a healthy, young, playful and carefree life that any child deserves.
There are three typical adjustment patterns adopted by adults with hearing loss. The first one is to remain withdrawn into your own self. This provides a sense of safety and familiarity which can be a comforting way to lead your life. The second is to act "as if" one does not even have hearing loss. A positive attitude will help people to live a life with no barriers and thus, engage in optimal interaction. The final and third pattern is for the person to accept their hearing loss as a part of them without undervaluing oneself. This means understanding that one is forced to live life with this disability, however it is not the only thing that constitutes life’s meaning. Furthermore, many feel as if their inability to hear others during conversation is their fault. It's important that these individuals learn how to become more assertive individuals who do not lack fear when it comes to asking someone to repeat something or to speak a little louder. Although there is much fatigue and frustration that is produced from one’s inability to hear, it is important to learn from personal experiences in order to improve on one’s communication skills. In essence, these patterns will help adults with hearing loss deal with the communication barriers that are present.[107]
Workplace
In most instances, people who are deaf find themselves working with hearing colleagues, where they can often be cut off from the communication going on around them. Interpreters can be provided for meetings and workshops, however are seldom provided for everyday work interactions. Communication of important information needed for jobs typically comes in the form of written or verbal summaries, which do not convey subtle meanings such as tone of voice, side conversations during group discussions, and body language. This can result in confusion and misunderstanding for the worker who is deaf, therefore making it harder to do their job effectively. Additionally, deaf workers can be unintentionally left out of professional networks, informal gatherings, and casual conversations among their collogues. Information about informal rules and organizational culture in the workplace is often communicated though these types of interactions, which puts the worker who is deaf at a professional and personal disadvantage. This could sever their job performance due to lack of access to information and therefore, reduce their opportunity to form relationships with their co-workers. Additionally, these communication barriers can all affect a deaf person’s career development. Since being able to effectively communicate with one's co-workers and other people relevant to one's job is essential to managerial positions, people with hearing loss can often be denied such opportunities.[106]
To avoid these situations in the workplace, individuals can take full-time or part-time sign language courses. In this way, they can become better able to communicate with the deaf and hard of hearing. Such courses teach the American Sign Language (ASL) language as most North Americans use this particular language to communicate. It is a visual language made up of specific gestures (signs), hand shapes, and facial expressions that contain their own unique grammatical rules and sentence structures [108] By completing sign language courses, it ensures that deaf individuals feel a part of the workplace and have the ability to communicate with their co-workers and employer in the manner as other hearing employees do.
Health care
Not only can communication barriers between deaf and hearing people affect family relationships, work, and school, but they can also have a very significant effect on a deaf individual’s health care. As a result of poor communication between the health care professional and the deaf or hard of hearing patient, many patients report that they are not properly informed about their disease and prognosis. [109] This lack of or poor communication could also lead to other issues such as misdiagnosis, poor assessments, mistreatment, and even possibly harm to patients. Poor communication in this setting is often the result of health care providers having the misconception that all people who are deaf or hard of hearing have the same type of hearing loss, and require the same type of communication methods. In reality, there are many different types and range of hearing loss, and in order to communicate effectively a health care provider needs to understand that each individual with hearing loss has unique needs. This affects how individuals have been educated to communicate, as some communication methods work better depending on an individual’s severity of hearing loss. For example, assuming every deaf or hard of hearing patient knows American Sign Language would be incorrect because there are different types of sign language, each varying in signs and meanings. A patient could have been educated to use cued speech which is entirely different from ASL.[109] Therefore, in order to communicate effectively, a health care provider needs to understand that each individual has unique needs when communicating.
Although there are specific laws and rules to govern communication between health care professionals and people who are deaf, they are not always followed due to the health care professional’s insufficient knowledge of communication techniques. This lack of knowledge can lead them to make assumptions about communicating with someone who is deaf, which can in turn cause them to use an unsuitable form of communication. Acts in countries such as the Americans with Disabilities Act (ADA) state that all health care providers are required to provide reasonable communication accommodations when caring for patients who are deaf. These accommodations could include qualified sign language interpreters, CDIs, and technology such as Internet interpretation services. A qualified sign language interpreter will enhance communication between a deaf individual and a health care professional by interpreting not only a health professional’s verbal communication, but also their non-verbal such as expressions, perceptions, and body language. A Certified Deaf Interpreter (CDI) is a sign language interpreter who is also a member of the Deaf community.[110] They accompany a sign language interpreter and are useful for communication with deaf individuals who also have language or cognitive deficits. A CDI will transform what the health care professional communicates into basic, simple language. This method takes much longer, however it can also be more effective than other techniques. Internet interpretation services are convenient and less costly, but can potentially pose significant risks. They involve the use of a sign language interpreter over a video device rather than directly in the room. This can often be an inaccurate form of communication because the interpreter may not be licensed, is often unfamiliar with the patient and their signs, and can lack knowledge of medical terminology.[111]
Aside from utilizing interpreters, healthcare professionals can improve their communication with deaf or hard of hearing patients by educating themselves on common misconceptions and proper practices depending on the patient’s needs. For example, a common misconception is that exaggerating words and speaking loudly will help the patient understand more clearly. However, many individuals with hearing loss depend on lip-reading to identify words. Exaggerated pronunciation and a raised voice can distort the lips, making it even more difficult to understand. Another common mistake health care professionals make are the use of single words rather than full sentences. Although language should be kept simple and short, keeping context is important because certain homophonous words are difficult to distinguish by lip-reading. Health care professionals can further improve their own communication with their patients by eliminating any background noise and positioning themselves in a way where their face is clearly visible to the patient, and suitably lit. The healthcare professional should know how to use body language and facial expressions to properly communicate different feelings.[109]
Research
Stem cell transplant and gene therapy
A 2005 study achieved successful regrowth of cochlea cells in guinea pigs.[112] However, the regrowth of cochlear hair cells does not imply the restoration of hearing sensitivity, as the sensory cells may or may not make connections with neurons that carry the signals from hair cells to the brain. A 2008 study has shown that gene therapy targeting Atoh1 can cause hair cell growth and attract neuronal processes in embryonic mice. Some hope that a similar treatment will one day ameliorate hearing loss in humans.[113]
Recent research, reported in 2012 achieved growth of cochlear nerve cells resulting in hearing improvements in gerbils,[114] using stem cells. Also reported in 2013 was regrowth of hair cells in deaf adult mice using a drug intervention resulting in hearing improvement.[115] The Hearing Health Foundation in the US has embarked on a project called the Hearing Restoration Project.[116] Also Action on Hearing Loss in the UK is also aiming to restore hearing.[117]
Researchers reported in 2015 that genetically deaf mice which were treated with TMC1 gene therapy recovered some of their hearing.[118][119] In 2017, additional studies were performed to treat Usher syndrome[120] and here, a recombinant adeno-associated virus seemed to outperform the older vectors.[121][122]
Audition
Besides research studies seeking to improve hearing, such as the ones listed above, research studies on the deaf have also been carried out in order to understand more about audition. Pijil and Shwarz (2005) conducted their study on the deaf who lost their hearing later in life and, hence, used cochlear implants to hear. They discovered further evidence for rate coding of pitch, a system that codes for information for frequencies by the rate that neurons fire in the auditory system, especially for lower frequencies as they are coded by the frequencies that neurons fire from the basilar membrane in a synchronous manner. Their results showed that the subjects could identify different pitches that were proportional to the frequency stimulated by a single electrode. The lower frequencies were detected when the basilar membrane was stimulated, providing even further evidence for rate coding.[59]
References
- ↑ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 "Deafness and hearing loss Fact sheet N°300". March 2015. Retrieved 23 May 2015.
- 1 2 Smith, RJH; Shearer, AE; Hildebrand, MS; Van Camp, G; Pagon, RA; Adam, MP; Ardinger, HH; Wallace, SE; Amemiya, A; Bean, LJH; Bird, TD; Fong, CT; Mefford, HC; Smith, RJH; Stephens, K (2014). "Deafness and Hereditary Hearing Loss Overview". PMID 20301607.
- ↑ GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015.". Lancet (London, England). 388 (10053): 1545–1602. PMC 5055577
 . PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/S0140-6736(16)31678-6. - ↑ "Deafness". Encyclopædia Britannica Online. Encyclopædia Britannica Inc. 2011. Retrieved 2012-02-22.
- 1 2 3 4 Lasak, JM; Allen, P; McVay, T; Lewis, D (Mar 2014). "Hearing loss: diagnosis and management.". Primary care. 41 (1): 19–31. PMID 24439878. doi:10.1016/j.pop.2013.10.003.
- 1 2 "1.1 billion people at risk of hearing loss WHO highlights serious threat posed by exposure to recreational noise" (PDF). who.int. 27 February 2015. Retrieved 2 March 2015.
- ↑ Global Burden of Disease Study 2013, Collaborators (22 August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet (London, England). 386 (9995): 743–800. PMC 4561509
 . PMID 26063472. doi:10.1016/s0140-6736(15)60692-4.
. PMID 26063472. doi:10.1016/s0140-6736(15)60692-4. - 1 2 3 WHO (2008). The global burden of disease: 2004 update (PDF). Geneva, Switzerland: World Health Organization. p. 35. ISBN 9789241563710.
- ↑ Olusanya, BO; Neumann, KJ; Saunders, JE (1 May 2014). "The global burden of disabling hearing impairment: a call to action.". Bulletin of the World Health Organization. 92 (5): 367–73. PMC 4007124
 . PMID 24839326. doi:10.2471/blt.13.128728.
. PMID 24839326. doi:10.2471/blt.13.128728. - 1 2 3 4 5 6 7 8 9 10 11 12 Elzouki, Abdelaziz Y (2012). Textbook of clinical pediatrics (2 ed.). Berlin: Springer. p. 602. ISBN 9783642022012.
- 1 2 "Community and Culture - Frequently Asked Questions". nad.org. National Association of the Deaf. Retrieved 31 July 2014.
- ↑ "Sound and Fury - Cochlear Implants - Essay". www.pbs.org. PBS. Retrieved 2015-08-01.
- ↑ "Understanding Deafness: Not Everyone Wants to Be 'Fixed'". www.theatlantic.com. The Atlantic. Retrieved 2015-08-01.
- ↑ "Why not all deaf people want to be cured". www.telegraph.co.uk. The Daily Telegraph. Retrieved 2015-08-02.
- 1 2 3 Sparrow, Robert (2005). "Defending Deaf Culture: The Case of Cochlear Implants" (PDF). The Journal of Political Philosophy. 13 (2). Retrieved 30 November 2014.
- ↑ eBook: Current Diagnosis & Treatment in Otolaryngology: Head & Neck Surgery, Lalwani, Anil K. (Ed.) Chapter 44: Audiologic Testing by Brady M. Klaves, PhD, Jennifer McKee Bold, AuD, Access Medicine
- ↑ "Community and Culture - Frequently Asked Questions". nad.org. National Association of the Deaf. Retrieved 27 Jan 2016.
- ↑ ANSI 7029:2000/BS 6951 Acoustics - Statistical distribution of hearing thresholds as a function of age
- ↑ ANSI S3.5-1997 Speech Intelligibility Index (SII)
- ↑ Robinson, DW; Sutton, GJ (1979). "Age effect in hearing – a comparative analysis of published threshold data". Audiology. 18 (4): 320–34. PMID 475664. doi:10.3109/00206097909072634.
- ↑ Worrall, L.,& Hickson, L. M. (2003). "Communication activity limitations", pp. 141–142 in Linda E. Worrall & Louise M. Hickson (Eds.). Communication disability in aging: from prevention to intervention. Clifton Park, NY: Delmar Learning
- ↑ "Hearing Loss and Older Adults" (Last Updated June 3, 2016). National Institute on Deafness and Other Communication Disorders. Retrieved September 11, 2016.
- 1 2 Oishi, N.; Schacht, J. (June 2011). "Emerging treatments for noise-induced hearing loss". Expert opinion on emerging drugs. 16 (2): 235–45. PMC 3102156
 . PMID 21247358. doi:10.1517/14728214.2011.552427.
. PMID 21247358. doi:10.1517/14728214.2011.552427. - ↑ "CDC - NIOSH Science Blog – A Story of Impact….". cdc.gov.
- ↑ "Noise and Hearing Conservation: Effects of Excessive Exposure". Occupational Safety & Health Administration. Retrieved July 14, 2016.
- ↑ "Threshold Shift (TS)". Simon Fraser University. Retrieved 2016-07-14.
- ↑ "About Hearing Loss". Centers for Disease Control and Prevention. Retrieved 2016-07-15.
- ↑ In the United States, United States Environmental Protection Agency, Occupational Safety and Health Administration, National Institute for Occupational Safety and Health, Mine Safety and Health Administration, and numerous state government agencies among others, set noise standards.
- ↑ Information on Levels of Environmental Noise Requisite to Protect Public Health and Welfare with an Adequate Margin of Safety. Document ID: usepa-1974
- ↑ "Deafness". SANDRA: South African National Deaf Association. Retrieved 2016-07-14.
- ↑ Occupational Noise Exposure, National Institute for Occupational Safety and Health 98-126
- ↑ "Compliance Guide to MSHA's Occupational Noise Exposure Standard, APPENDIX B – GLOSSARY OF TERMS".
- 1 2 "Noise-Induced Hearing Loss: Promoting Hearing Health Among Youth". CDC Healthy Youth!. CDC. 2009-07-01.
- ↑ Goines, Lisa; Hagler, Louis (March 2007). "Noise Pollution: A Modern Plague". Southern Medical Journal. 100: 287–294. doi:10.1097/smj.0b013e3180318be5. Retrieved 26 November 2014.
- ↑ Rosen, S; et al. (1962). "Presbycusis study of a relatively noise-free population in the Sudan". Ann. Otol. Rhinol. Laryngol. 71: 727–743. doi:10.1177/000348946207100313.
- ↑ Bergman, Moe (1966). "Hearing in the Mabaans. A critical review of related Literature". Arch. Otolaryngol. 84: 411–415. doi:10.1001/archotol.1966.00760030413007.
- ↑ Goycoolea, MV; et al. (1986). "Effect of life in industrialized societies on hearing in natives of Easter Island". Laryngoscope. 96: 1391–1396. doi:10.1288/00005537-198612000-00015.
- ↑ Committee on Noise-Induced Hearing Loss and Tinnitus Associated with Military Service from World War II to the Present, Medical Follow-up Agency (2006). Humes, Larry; Joellenbeck, Lois; Durch, Jane, eds. Noise and military service : implications for hearing loss and tinnitus (eBook). 500 Fifth Street, N.W., Washington, DC 20001: THE NATIONAL ACADEMIES PRESS. pp. 72–111. ISBN 0-309-09949-8. Retrieved 26 November 2014.
- ↑ de Laat, JA; van Deelen, L; Wiefferink, K (September 2016). "Hearing Screening and Prevention of Hearing Loss in Adolescents.". The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 59 (3): 243–5. PMID 27562364. doi:10.1016/j.jadohealth.2016.06.017.
- 1 2 3 Rehm, Heidi. "The Genetics of Deafness; A Guide for Patients and Families" (PDF). Harvard Medical School Center For Hereditary Deafness. Harvard Medical School.
- ↑ Lynch, Eric D.; Lee, Ming K.; Morrow, Jan E.; Welcsh, Piri L.; León, Pedro E.; King, Mary-Claire (1997-11-14). "Nonsyndromic deafness DFNA1 associated with mutation of a human homolog of the Drosophila gene diaphanous". Science. 278 (5341): 1315–18. PMID 9360932. doi:10.1126/science.278.5341.1315.
- ↑ Schraders, M.; Oostrik, J.; Huygen, P.L.; Strom, T.M.; van Wijk, E.; Kunst, H.P.; Hoefsloot, L.H.; Cremers, C.W.; Admiraal, R.J.; Kremer, H. (March 2010). "Mutations in PTPRQ Are a Cause of Autosomal-Recessive Nonsyndromic Hearing Impairment DFNB84 and Associated with Vestibular Dysfunction". The American Journal of Human Genetics. 86 (4): 604–10. PMC 2850434
 . PMID 20346435. doi:10.1016/j.ajhg.2010.02.015.
. PMID 20346435. doi:10.1016/j.ajhg.2010.02.015. - ↑ Byl, et.al., FM (1977). "Auditory symptoms associated with herpes zoster or idiopathic facial paralysis". Laryngoscope. 87 (3): 372–9. doi:10.1288/00005537-197703000-00010.
- ↑ Araújo Eda, S; Zucki, F; Corteletti, LC; Lopes, AC; Feniman, MR; Alvarenga Kde, F (2012). "Hearing loss and acquired immune deficiency syndrome: systematic review.". Jornal da Sociedade Brasileira de Fonoaudiologia. 24 (2): 188–92. PMID 22832689. doi:10.1590/s2179-64912012000200017.
- ↑ Rodman, R; Pine, HS (Jun 2012). "The otolaryngologist's approach to the patient with Down syndrome.". Otolaryngologic clinics of North America. 45 (3): 599–629, vii–viii. PMID 22588039. doi:10.1016/j.otc.2012.03.010.
- ↑ http://omim.org/entry/118300
- ↑ Curhan, Sharon G.; Shargorodsky, Josef; Eavey, Roland; Curhan, Gary C. (2012-02-29). "Analgesic Use and the Risk of Hearing Loss in Women". Oxford Journals: American Journal of EPIDEMIOLOGY.
- ↑ Cone, Barbara; Dorn, Patricia; Konrad-Martin, Dawn; Lister, Jennifer; Ortiz, Candice; Schairer, Kim. "Ototoxic Medications (Medication Effects)". American Speech-Language-Hearing Association.
- ↑ "FDA Announces Revisions to Labels for Cialis, Levitra and Viagra". Food and Drug Administration. 2007-10-18. Retrieved 2011-10-30.
- 1 2 "Tox Town – Toluene – Toxic chemicals and environmental health risks where you live and work – Text Version". toxtown.nlm.nih.gov. Retrieved 2010-06-09.
- 1 2 3 Morata, Thais C. "Addressing the Risk for Hearing Loss from Industrial Chemicals". CDC. Retrieved 2008-06-05.
- ↑ Johnson, Ann-Christin (2008-09-09). "Occupational exposure to chemicals and hearing impairment – the need for a noise notation" (PDF). Karolinska Institutet: 1–48. Retrieved 2009-06-19.
- ↑ Sliwinska-Kowalska, M.; Zamyslowska-Szmytke, E.; Szymczak, W.; Kotylo, P.; Fiszer, M.; Wesolowski, W.; Pawlaczyk-Luszczynska, M. (May 2005). "Exacerbation of noise-induced hearing loss by co-exposure to workplace chemicals". Environmental Toxicology and Pharmacology. 19 (3): 547–553. doi:10.1016/j.etap.2004.12.018.
- ↑ Oesterle, EC (March 2013). "Changes in the adult vertebrate auditory sensory epithelium after trauma.". Hearing research. 297: 91–8. PMC 3637947
 . PMID 23178236. doi:10.1016/j.heares.2012.11.010.
. PMID 23178236. doi:10.1016/j.heares.2012.11.010. - ↑ Eggermont, JJ (24 May 2016). "Acquired hearing loss and brain plasticity.". Hearing research. PMID 27233916. doi:10.1016/j.heares.2016.05.008.
- ↑ U.S.C. (2012). How We Hear. Sc.edu. Retrieved from http://www.sc.edu/ehs/modules/Noise/hearing.htm
- ↑ Hayes, K. (2009). Hear. About.com. Retrieved from http://ent.about.com/od/entanatomybasics/ht/How We Hear.htm
- 1 2 Carlson, N. R. (2010). Physiology of behavior. (11 ed.). Upper Saddle River, New Jersey: Pearson Education, Inc.
- ↑ Jansen, et.al., S (2013). "Efficient hearing screening in noise-exposed listeners using the digit triplet test.". Ear Hear. 34 (6): 773–8. doi:10.1097/AUD.0b013e318297920b.
- ↑ "BIAP Recommendation 02/1 bis - AUDIOMETRIC CLASSIFICATION OF HEARING IMPAIRMENTS". biap.org. International Bureau Audiophonology. 26 October 1996. Retrieved 18 June 2017.
- ↑ Russell JL, Pine HS, Young DL (2013). "Pediatric cochlear implantation: expanding applications and outcomes.". Pediatric Clinics of North America. 60 (4): 841–863. PMID 23905823. doi:10.1016/j.pcl.2013.04.008.
- ↑ Lieu JE. Speech-language and educational consequences of unilateral hearing loss in children. Arch Otolaryngol Head Neck Surg. 2004: 130(5);524-30.
- ↑ Kitterick PT, O'Donoghue GM, Edmondson-Jones M, Marshall A, Jeffs E, Craddock L, Riley A, Green K, O'Driscoll M, Jiang D, Nunn T, Saeed S, Aleksy W, Seeber BU (Aug 11, 2014). "Comparison of the benefits of cochlear implantation versus contra-lateral routing of signal hearing aids in adult patients with single-sided deafness: study protocol for a prospective within-subject longitudinal trial.". BMC Ear Nose Throat Disord. 14 (1): 7. PMC 4141989
 . PMID 25152694. doi:10.1186/1472-6815-14-7.
. PMID 25152694. doi:10.1186/1472-6815-14-7. - 1 2 3 Riss D, Arnoldner C, Baumgartner WD, Blineder M, Flak S, Bachner A, Gstoettner W, Hamzavi JS (2014). "Indication criteria and outcomes with the Bonebridge transcutaneous bone-conduction implant.". Laryngoscope. 124: 2802–2806. PMID 25142577. doi:10.1002/lary.24832.
- ↑ Graham, edited by John M.; Baguley, David M. (2009). Ballantyne's Deafness. (7th ed.). Chichester: John Wiley & Sons. p. 16. ISBN 978-0-470-74441-3.
- ↑ "Childhood hearing loss: act now, here's how!" (PDF). WHO. 2016. p. 6. Retrieved 2 March 2016.
Over 30% of childhood hearing loss is caused by diseases such as measles, mumps, rubella, meningitis and ear infections. These can be prevented through immunization and good hygiene practices. Another 17% of childhood hearing loss results from complications at birth, including prematurity, low birth weight, birth asphyxia and neonatal jaundice. Improved maternal and child health practices would help to prevent these complications. The use of ototoxic medicines in expectant mothers and newborns, which is responsible for 4% of childhood hearing loss, could potentially be avoided.
- ↑ Davis, Adrian; McMahon, Catherine M.; Pichora-Fuller, Kathleen M.; Russ, Shirley; Lin, Frank; Olusanya, Bolajoko O.; Chadha, Shelly; Tremblay, Kelly L. (2016-04-01). "Aging and Hearing Health: The Life-course Approach". The Gerontologist. 56 (Suppl_2): S256–S267. ISSN 0016-9013. doi:10.1093/geront/gnw033.
- ↑ El Dib, R.P.; Mathew, J.L.; Martins, R.H. (2012-04-18). El Dib, Regina P, ed. "Interventions to promote the wearing of hearing protection". Cochrane database of systematic reviews (Online). 4: CD005234. PMID 22513929. doi:10.1002/14651858.CD005234.pub5.
- ↑ Stucken, EZ; Hong, RS (October 2014). "Noise-induced hearing loss: an occupational medicine perspective.". Current Opinion in Otolaryngology & Head and Neck Surgery. 22 (5): 388–93. PMID 25188429. doi:10.1097/moo.0000000000000079.
- ↑ "Noise and Hearing Loss Prevention". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Retrieved July 15, 2016.
- ↑ "Safety and Health Topics: Occupational Noise Exposure". Occupational Safety and Health Administration. Retrieved July 15, 2015.
- ↑ "Controls for Noise Exposure". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Retrieved July 15, 2016.
- ↑ "Excellence in Hearing Loss Prevention Award". Safe-in-Sound. Retrieved July 15, 2016.
- ↑ "Buy Quiet". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Retrieved July 15, 2016.
- ↑ "PowerTools Database". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Retrieved July 15, 2016.
- ↑ "CDC - NIOSH Publications and Products - Occupationally-Induced Hearing Loss (2010-136)". cdc.gov.
- ↑ Verbeek, JH; Kateman, E; Morata, TC; Dreschler, WA; Mischke, C (17 October 2012). "Interventions to prevent occupational noise-induced hearing loss.". The Cochrane database of systematic reviews. 10: CD006396. PMID 23076923. doi:10.1002/14651858.CD006396.pub3.
- ↑ Moyer, Virginia A. (2012-11-06). "Screening for Hearing Loss in Older Adults: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. The American College of Physicians. pp. 655–661. Retrieved 2012-11-06.
- ↑ "Who Should be Screened for Hearing Loss". www.asha.org. Retrieved 2017-03-17.
- ↑ "Hearing and Other Sensory or Communication Disorders | Healthy People 2020". www.healthypeople.gov. Retrieved 2017-03-17.
- 1 2 National Institute on Deafness and Other Communication Disorders(NIDCD)(2013). Hearing Aids. Retrieved from http://www.nidcd.nih.gov/health/hearing/pages/hearingaid.aspx
- 1 2 McCormack, Abby; Fortnum, Heather (2013-05-01). "Why do people fitted with hearing aids not wear them?". International Journal of Audiology. 52 (5): 360–368. ISSN 1499-2027. PMC 3665209
 . PMID 23473329. doi:10.3109/14992027.2013.769066.
. PMID 23473329. doi:10.3109/14992027.2013.769066. - 1 2 3 Working with Hearing Loss. (2008). Retrieved October 31, 2014, from http://www.chha.ca/documents/Working_With_Hearing_Loss.pdf
- ↑ "Free Phone Caption Service for the Deaf and Hard of Hearing. [sic]". Phone Caption. Retrieved 2010-12-10.
- ↑ Meyers, Carol, Dr. "Infrared, Frequency/Digital Modulation, and Induction Hearing Loops : A comparison of assisted listening system technologies". Technology for Worship. INSPIRATION Technology Conferences, Inc. Retrieved 30 November 2014.
- ↑ "Cochlear Implantation in Adults A Systematic Review and Meta-analysis". JAMA Otolaryngol Head Neck Surgery. 139: 265. 2013. doi:10.1001/jamaoto.2013.1744.
- ↑ "FDA Public Health Notification: Risk of Bacterial Meningitis in Children with Cochlear Implants". FDA. 2002-07-24. Retrieved 2008-11-09.
- ↑ "Elliot & Oliver's Story – Research". cochlearimplant.net. 2006. Archived from the original on 2008-03-02.
- ↑ "CART Systems".
- ↑ "Auditory Sciences". Auditory Sciences.
- ↑ "An Educators Guide to Hearing Disability Issues. (n.d.).". UIUC. Retrieved 2009-07-19. | "Facts About Hearing Loss". Alexander Bell Association for the Deaf and Hard of Hearing. 2005. Retrieved 2009-07-19.
- ↑ Hoffman, Howard J.; Dobie, Robert A.; Losonczy, Katalin G.; Themann, Christa L.; Flamme, Gregory A. "Declining Prevalence of Hearing Loss in US Adults Aged 20 to 69 Years". JAMA Otolaryngology–Head & Neck Surgery. 143: 274. doi:10.1001/jamaoto.2016.3527.
- ↑ Carroll, Yulia I; Eichwald, John; Scinicariello, Franco; Hoffman, Howard J.; Deitchman, Scott; Radke, Marilyn S.; Themann, Christa L.; Breysse, Patrick (2017-01-01). "Vital Signs: Noise-Induced Hearing Loss Among Adults — United States 2011–2012". MMWR. Morbidity and Mortality Weekly Report. 66 (5): 139–144. ISSN 0149-2195. doi:10.15585/mmwr.mm6605e3.
- ↑ Frishberg, Nancy (September 1975). "Arbitrariness and Iconicity: Historical Change in American Sign Language". Language. 51 (3): 696. doi:10.2307/412894.
- ↑ Kral A, O'Donoghue GM (2010). "Profound Deafness in Childhood". New England J Medicine. 363: 1438–50. PMID 20925546. doi:10.1056/nejmra0911225.
- ↑ Deaf Heritage: A Narrative History of Deaf America by Jack Gannon (National Association of the Deaf, 1981)
- ↑ "American Deaf Culture". Sign Media, Incorporated. Sign Media, Inc. Retrieved 14 May 2013.
- ↑ Drolsbaugh, Mark. "Everything You've Wanted to Know About Deaf Culture (And Then Some)". Deaf Culture Online. Archived from the original on 2011-02-13. Retrieved 2011-11-28.
- ↑ NAD Cochlear Implant Committee. "NAD Position Statement on Cochlear Implants (2000)". Cochlear Implants %7c National Association of the Deaf. National Association of the Deaf. Retrieved 30 November 2014.
- ↑ "American Sign Language". NIDCD. Retrieved 17 November 2016.
- ↑ http://www2.ed.gov/about/offices/list/ocr/docs/hq9806.html
- 1 2 Smith, D. D., & Tyler, N. C. (2010). Introduction to Special Education. Columbus: Merrill.
- ↑ "Regulations: Part 300 / A / 300.8 / c". U. S. Department of Education. U. S. Department of Education. Retrieved 9 August 2015.
- ↑ Haynes, W. O., Moran, M. J., & Pindzola, R. H. (2012). Hearing Loss. Communication Disorders in Educational and Medical Settings An Introduction for Speech-Language Pathologists, Educators, and Health Professionals (pp. 280-282). Sudbury, MA: Jones & Bartlett Learning.
- 1 2 3 Foster, S. (1996). Communication experiences of deaf people: An ethnographic account. In I. Parasnis (Ed.), Cultural and language diversity of the deaf experience (pp. 117-136). New York: Cambridge University Press.
- ↑ Scherer, M. J. (2004). The Personal Meaning of Hearing or Vision Loss. Connecting To Learn Educational and Assistive Technology for People With Disabilities. (pp. 41-55). Washington, DC: American Psychological Association.
- ↑ Sign Language Classes for Individuals. (2013, January 1). Retrieved November 5, 2014.
- 1 2 3 Medicina Oral, Patología Oral y Cirugía Bucal. (2007, January 1). Retrieved October 31, 2014, from http://scielo.isciii.es/scielo.php?pid=S1698-69462007000800007&script=sci_arttext
- ↑ Ramstead, A. (2014, January 15). The Role of the Certified Deaf Interpreter. Retrieved November 2, 2014, from http://www.indemandinterpreting.com/role-certified-deaf-interpreter/
- ↑ Schuler, G., Mistler, L., Torrey, K., & Depukat, R. (2013). Bridging Communication Gaps with the Deaf. Nursing, 43(11), 24-30.
- ↑ Coghlan, Andy (2005-02-14). "Gene therapy is first deafness 'cure'". NewScientist.com News Service.
- ↑ Gubbels, SP; Woessner, DW; Mitchell, JC; Ricci, AJ; Brigande, JV (2008). "Functional auditory hair cells produced in the mammalian cochlea by in utero gene transfer". Nature. 455 (7212): 537–41. PMC 2925035
 . PMID 18754012. doi:10.1038/nature07265.
. PMID 18754012. doi:10.1038/nature07265. - ↑ Gewin, Virginia (2012-09-12). "Human embryonic stem cells restore gerbil hearing". Nature. doi:10.1038/nature.2012.11402. Retrieved 2013-01-22.
- ↑ Ander, Davida. "Drug may reverse permanent deafness by regenerating cells of inner ear: Harvard study". National Post. National Post.
- ↑ "Hearing Health Foundation". HHF. Retrieved 2013-01-22.
- ↑ "Biomedical research – Action On Hearing Loss". RNID. Retrieved 2013-01-22.
- ↑ Gallacher, James (9 July 2015). "Deafness could be treated by virus, say scientists". UK: BBC. Retrieved 9 July 2015.
- ↑ Askew, Charles; et al. (8 July 2015). "Tmc gene therapy restores auditory function in deaf mice". Science Translational Medicine. American Association for the Advancement of Science. 7 (295): 295ra108. PMID 26157030. doi:10.1126/scitranslmed.aab1996.
- ↑ Isgrig, K; Shteamer, JW; Belyantseva, IA; Drummond, MC; Fitzgerald, TS; Vijayakumar, S; Jones, SM; Griffith, AJ; Friedman, TB; Cunningham, LL; Chien, WW (March 2017). "Gene Therapy Restores Balance and Auditory Functions in a Mouse Model of Usher Syndrome". Molecular Therapy. 25 (3): 780–791. PMID 28254438. doi:10.1016/j.ymthe.2017.01.007.
- ↑ Landegger, LD; Pan, B; Askew, C; Wassmer, SJ; Gluck, SD; Galvin, A; Taylor, R; Forge, A; Stankovic, KM; Holt, JR; Vandenberghe, LH (March 2017). "A synthetic AAV vector enables safe and efficient gene transfer to the mammalian inner ear". Nature Biotechnology. 35 (3): 280–284. PMID 28165475. doi:10.1038/nbt.3781.
- ↑ Pan, B; Askew, C; Galvin, A; Heman-Ackah, S; Asai, Y; Indzhykulian, AA; Jodelka, FM; Hastings, ML; Lentz, JJ; Vandenberghe, LH; Holt, JR; Géléoc, GS (March 2017). "Gene therapy restores auditory and vestibular function in a mouse model of Usher syndrome type 1c". Nature Biotechnology. 35 (3): 264–272. PMID 28165476. doi:10.1038/nbt.3801.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
| Wikimedia Commons has media related to Hearing impairment. |
| Wikiquote has quotations related to: Hearing loss |
- Hearing loss at DMOZ
- "Hearing Loss in Children". Hearing Loss in Children Home. Retrieved 17 March 2017.
