Health effects of tobacco

Tobacco use has predominantly negative effects on human health and concern about health effects of tobacco has a long history. Research has focused primarily on cigarette tobacco smoking.[1][2] In 1950, Richard Doll published research in the British Medical Journal showing a close link between smoking and lung cancer.[3] Four years later, in 1954, the British Doctors Study, a study of some 40,000 doctors over 20 years, confirmed the suggestion, based on which the government issued advice that smoking and lung cancer rates were related.[4][5]
Tobacco use is the single greatest cause of preventable death globally.[6] As many as half of people who use tobacco die from the results of this use.[7] The World Health Organization (WHO) estimates that each year tobacco causes about 6 million deaths (about 10% of all deaths) with 600,000 of these occurring in non smokers due to second hand smoke.[7][8] In the 20th century tobacco is estimated to have caused 100 million deaths.[7] Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."[9]
Tobacco use leads most commonly to diseases affecting the heart, liver and lungs. Smoking is a major risk factor for heart attacks, strokes, chronic obstructive pulmonary disease (COPD) (including emphysema and chronic bronchitis), and cancer (particularly lung cancer, cancers of the larynx and mouth, and pancreatic cancer). It also causes peripheral vascular disease and hypertension. The effects depend on the number of years that a person smokes and on how much the person smokes. Starting smoking earlier in life and smoking cigarettes higher in tar increases the risk of these diseases. Also, environmental tobacco smoke, or secondhand smoke, has been shown to cause adverse health effects in people of all ages.[10] Tobacco use is a significant factor in miscarriages among pregnant smokers, and it contributes to a number of other health problems of the fetus such as premature birth, low birth weight, and increases by 1.4 to 3 times the chance of sudden infant death syndrome (SIDS).[11] Incidence of erectile dysfunction is approximately 85 percent higher in male smokers compared to non-smokers.[12][13]
Several countries have taken measures to control the consumption of tobacco with usage and sales restrictions as well as warning messages printed on packaging. Additionally smoke free laws are useful, do not have negative economic effects for restaurants or bars and help people who smoke to quit.[7] Taxing tobacco products in an effort to increase the price is also effective, especially in developing countries.[7] Tobacco smoke contains more than fifty chemicals that cause cancer.[7] Tobacco also contains nicotine, which is a highly addictive psychoactive drug. When tobacco is smoked, nicotine causes physical and psychological dependency. Cigarettes sold in underdeveloped countries tend to have higher tar content, and are less likely to be filtered, potentially increasing vulnerability to tobacco smoking related disease in these regions.[14]
| Part of a series on |
| Tobacco |
|---|
 |
| History |
| Biology |
| Personal and social impact |
| Production |
Health effects of smoking

Smoking most commonly leads to diseases affecting the heart and lungs and will most commonly affect areas such as hands or feet with first signs of smoking related health issues showing up as numbness, with smoking being a major risk factor for heart attacks, chronic obstructive pulmonary disease (COPD), emphysema, and cancer, particularly lung cancer, cancers of the larynx and mouth, and pancreatic cancer.[16] Overall life expectancy is also reduced in long term smokers, with estimates ranging from 10[5] to 17.9.[17] years fewer than nonsmokers.[18] About one half of long term male smokers will die of illness due to smoking.[19] The association of smoking with lung cancer is strongest, both in the public perception and etiologically. Among male smokers, the lifetime risk of developing lung cancer is 17.2%; among female smokers, the risk is 11.6%. This risk is significantly lower in nonsmokers: 1.3% in men and 1.4% in women.[20] Historically, lung cancer was considered to be a rare disease prior to World War I and was perceived as something most physicians would never see during their career. With the postwar rise in popularity of cigarette smoking came a virtual epidemic of lung cancer.[21][22]
A person's increased risk of contracting disease is directly proportional to the length of time that a person continues to smoke as well as the amount smoked. However, if someone stops smoking, then these chances gradually decrease as the damage to their body is repaired. A year after quitting, the risk of contracting heart disease is half that of a continuing smoker.[23] The health risks of smoking are not uniform across all smokers. Risks vary according to the amount of tobacco smoked, with those who smoke more at greater risk. Smoking so-called "light" cigarettes does not reduce the risk.[24]
Mortality
Smoking is the cause of about 5 million deaths per year.[25] This makes it the most common cause of preventable early death.[26] One study found that male and female smokers lose on average of 13.2 and 14.5 years of life, respectively.[27] Another found a loss of life of 6.8 years.[28] Each cigarette that is smoked is estimated to shorten life by an average of 11 minutes.[29][30][31] At least half of all lifelong smokers die earlier as a result of smoking.[5] Smokers are three times as likely to die before the age of 60 or 70 as non-smokers.[5][32][33]
In the United States, cigarette smoking and exposure to tobacco smoke accounts for roughly one in five,[34] or at least 443,000 premature deaths annually.[35] To put this into context, ABC's Peter Jennings famously reported that in the US alone, tobacco kills the equivalent of three jumbo jets full of people crashing every day, with no survivors.[36] On a worldwide basis, this equates to a single jumbo jet every hour.[37]
A 2015 study found that about 17% of mortality due to cigarette smoking in the United States is due to diseases other than those usually believed to be related.[38]
Cancer
The primary risks of tobacco usage include many forms of cancer, particularly lung cancer,[39] kidney cancer,[40] cancer of the larynx and head and neck,[41][42] bladder cancer,[43] cancer of the esophagus,[44] cancer of the pancreas[45] and stomach cancer.[46] Studies have established a relationship between tobacco smoke, including secondhand smoke, and cervical cancer in women.[47] There is some evidence suggesting a small increased risk of myeloid leukaemia,[48] squamous cell sinonasal cancer, liver cancer, colorectal cancer, cancers of the gallbladder, the adrenal gland, the small intestine, and various childhood cancers.[46] The possible connection between breast cancer and tobacco is still uncertain.[49]
The risk of dying from lung cancer before age 85 is 22.1% for a male smoker and 11.9% for a female smoker, in the absence of competing causes of death. The corresponding estimates for lifelong nonsmokers are a 1.1% probability of dying from lung cancer before age 85 for a man of European descent, and a 0.8% probability for a woman.[50]
Pulmonary

In smoking, long term exposure to compounds found in the smoke (e.g., carbon monoxide and cyanide) are believed to be responsible for pulmonary damage and for loss of elasticity in the alveoli, leading to emphysema and COPD. Chronic obstructive pulmonary disease (COPD) caused by smoking, is a permanent, incurable (often terminal) reduction of pulmonary capacity characterised by shortness of breath, wheezing, persistent cough with sputum, and damage to the lungs, including emphysema and chronic bronchitis.[51] The carcinogen acrolein and its derivatives also contribute to the chronic inflammation present in COPD.[52]
Cardiovascular disease

Inhalation of tobacco smoke causes several immediate responses within the heart and blood vessels. Within one minute the heart rate begins to rise, increasing by as much as 30 percent during the first 10 minutes of smoking. Carbon monoxide in tobacco smoke exerts negative effects by reducing the blood’s ability to carry oxygen.[53]
Smoking also increases the chance of heart disease, stroke,[54] atherosclerosis, and peripheral vascular disease.[55] Several ingredients of tobacco lead to the narrowing of blood vessels, increasing the likelihood of a blockage, and thus a heart attack or stroke. According to a study by an international team of researchers, people under 40 are five times more likely to have a heart attack if they smoke.[56]
Recent research by American biologists has shown that cigarette smoke also influences the process of cell division in the cardiac muscle and changes the heart's shape.[57]
The usage of tobacco has also been linked to Buerger's disease (thromboangiitis obliterans) the acute inflammation and thrombosis (clotting) of arteries and veins of the hands and feet.[58]
Although cigarette smoking causes a greater increase in the risk of cancer than cigar smoking, cigar smokers still have an increased risk for many health problems, including cancer, when compared to non-smokers.[59][60] As for second-hand smoke, the NIH study points to the large amount of smoke generated by one cigar, saying "cigars can contribute substantial amounts of tobacco smoke to the indoor environment; and, when large numbers of cigar smokers congregate in a cigar smoking event, the amount of ETS [i.e. second-hand smoke] produced is sufficient to be a health concern for those regularly required to work in those environments."[61]
Smoking tends to increase blood cholesterol levels. Furthermore, the ratio of high-density lipoprotein (the "good" cholesterol) to low-density lipoprotein (the "bad" cholesterol) tends to be lower in smokers compared to non-smokers. Smoking also raises the levels of fibrinogen and increases platelet production (both involved in blood clotting) which makes the blood viscous. Carbon monoxide binds to haemoglobin (the oxygen-carrying component in red blood cells), resulting in a much stabler complex than haemoglobin bound with oxygen or carbon dioxide—the result is permanent loss of blood cell functionality. Blood cells are naturally recycled after a certain period of time, allowing for the creation of new, functional erythrocytes. However, if carbon monoxide exposure reaches a certain point before they can be recycled, hypoxia (and later death) occurs. All these factors make smokers more at risk of developing various forms of arteriosclerosis. As the arteriosclerosis progresses, blood flows less easily through rigid and narrowed blood vessels, making the blood more likely to form a thrombosis (clot). Sudden blockage of a blood vessel may lead to an infarction (stroke). However, it is also worth noting that the effects of smoking on the heart may be more subtle. These conditions may develop gradually given the smoking-healing cycle (the human body heals itself between periods of smoking), and therefore a smoker may develop less significant disorders such as worsening or maintenance of unpleasant dermatological conditions, e.g. eczema, due to reduced blood supply. Smoking also increases blood pressure and weakens blood vessels.[62]
Renal
In addition to increasing the risk of kidney cancer, smoking can also contribute to additional renal damage. Smokers are at a significantly increased risk for chronic kidney disease than non-smokers.[63] A history of smoking encourages the progression of diabetic nephropathy.[64]
Influenza
A study of an outbreak of an (H1N1) influenza in an Israeli military unit of 336 healthy young men to determine the relation of cigarette smoking to the incidence of clinically apparent influenza, revealed that, of 168 smokers, 68.5 percent had influenza, as compared with 47.2 percent of nonsmokers. Influenza was also more severe in the smokers; 50.6 percent of the smokers lost work days or required bed rest, or both, as compared with 30.1 percent of the nonsmokers.[65]
According to a study of 1,900 male cadets after the 1968 Hong Kong A2 influenza epidemic at a South Carolina military academy, compared with nonsmokers, heavy smokers (more than 20 cigarettes per day) had 21% more illnesses and 20% more bed rest, light smokers (less than 20 cigarettes per day) had 10% more illnesses and 7% more bed rest.[66]
The effect of cigarette smoking upon epidemic influenza was studied prospectively among 1,811 male college students. Clinical influenza incidence among those who daily smoked 21 or more cigarettes was 21% higher than that of non-smokers. Influenza incidence among smokers of 1 to 20 cigarettes daily was intermediate between non-smokers and heavy cigarette smokers.[66]
Surveillance of a 1979 influenza outbreak at a military base for women in Israel revealed that influenza symptoms developed in 60.0% of the current smokers vs. 41.6% of the nonsmokers.[67]
Smoking seems to cause a higher relative influenza-risk in older populations than in younger populations. In a prospective study of community-dwelling people 60–90 years of age, during 1993, of unimmunized people 23% of smokers had clinical influenza as compared with 6% of non-smokers.[68]
Smoking may substantially contribute to the growth of influenza epidemics affecting the entire population.[65] However the proportion of influenza cases in the general non-smoking population attributable to smokers has not yet been calculated.
Oral
Perhaps the most serious oral condition that can arise is that of oral cancer. However, smoking also increases the risk for various other oral diseases, some almost completely exclusive to tobacco users. The National Institutes of Health, through the National Cancer Institute, determined in 1998 that "cigar smoking causes a variety of cancers including cancers of the oral cavity (lip, tongue, mouth, throat), esophagus, larynx, and lung."[61] Pipe smoking involves significant health risks,[69][70] particularly oral cancer.[71][72] Roughly half of periodontitis or inflammation around the teeth cases are attributed to current or former smoking. Smokeless tobacco causes gingival recession and white mucosal lesions. Up to 90% of periodontitis patients who are not helped by common modes of treatment are smokers. Smokers have significantly greater loss of bone height than nonsmokers, and the trend can be extended to pipe smokers to have more bone loss than nonsmokers.[73] Smoking has been proven to be an important factor in the staining of teeth.[74][75] Halitosis or bad breath is common among tobacco smokers.[76] Tooth loss has been shown to be 2[77] to 3 times[78] higher in smokers than in non-smokers.[79] In addition, complications may further include leukoplakia, the adherent white plaques or patches on the mucous membranes of the oral cavity, including the tongue.[80]
Infection
Smoking is also linked to susceptibility to infectious diseases, particularly in the lungs. Smoking more than 20 cigarettes a day increases the risk of by two to four times,[81][82] and being a current smoker has been linked to a fourfold increase in the risk of invasive pneumococcal disease.[83] It is believed that smoking increases the risk of these and other pulmonary and respiratory tract infections both through structural damage and through effects on the immune system. The effects on the immune system include an increase in CD4+ cell production attributable to nicotine, which has tentatively been linked to increased HIV susceptibility.[84]
Smoking increases the risk of Kaposi's sarcoma in people without HIV infection.[85] One study found this only with the male population and could not draw any conclusions for the female participants in the study.[86]
Impotence
Incidence of impotence is approximately 85 percent higher in male smokers compared to non-smokers,[87] and it is a key cause of erectile dysfunction (ED).[12][87] Smoking causes impotence because it promotes arterial narrowing.[88]
Female infertility
Smoking is harmful to the ovaries, potentially causing female infertility, and the degree of damage is dependent upon the amount and length of time a woman smokes. Nicotine and other harmful chemicals in cigarettes interfere with the body’s ability to create estrogen, a hormone that regulates folliculogenesis and ovulation. Also, cigarette smoking interferes with folliculogenesis, embryo transport, endometrial receptivity, endometrial angiogenesis, uterine blood flow and the uterine myometrium.[89] Some damage is irreversible, but stopping smoking can prevent further damage.[90][91] Smokers are 60% more likely to be infertile than non-smokers.[92] Smoking reduces the chances of IVF producing a live birth by 34% and increases the risk of an IVF pregnancy miscarrying by 30%.[92]
Psychological
The American Psychologist stated "Smokers often report that cigarettes help relieve feelings of stress. However, the stress levels of adult smokers are slightly higher than those of nonsmokers, adolescent smokers report increasing levels of stress as they develop regular patterns of smoking, and smoking cessation leads to reduced stress. Far from acting as an aid for mood control, nicotine dependency seems to exacerbate stress. This is confirmed in the daily mood patterns described by smokers, with normal moods during smoking and worsening moods between cigarettes. Thus, the apparent relaxant effect of smoking only reflects the reversal of the tension and irritability that develop during nicotine depletion. Dependent smokers need nicotine to remain feeling normal."[93]
Immediate effects
Users report feelings of relaxation, sharpness, calmness, and alertness.[94] Those new to smoking may experience nausea, dizziness, increased blood pressure, narrowed arteries, and rapid heart beat. Generally, the unpleasant symptoms will eventually vanish over time, with repeated use, as the body builds a tolerance to the chemicals in the cigarettes, such as nicotine.
Stress
Smokers report higher levels of everyday stress.[95] Several studies have monitored feelings of stress over time and found reduced stress after quitting.[96][97]
The deleterious mood effects of abstinence explain why smokers suffer more daily stress than non-smokers and become less stressed when they quit smoking. Deprivation reversal also explains much of the arousal data, with deprived smokers being less vigilant and less alert than non-deprived smokers or non-smokers.[95]
Recent studies have shown a positive relationship between psychological distress and salivary cotinine levels in smoking and non-smoking adults, indicating that both firsthand and secondhand smoke exposure may lead to higher levels of mental stress.[98]
Social and behavioral
Medical researchers have found that smoking is a predictor of divorce.[99] Smokers have a 53% greater chance of divorce than nonsmokers.[100]
Cognitive function
The usage of tobacco can also create cognitive dysfunction. There seems to be an increased risk of Alzheimer's disease, although "case–control and cohort studies produce conflicting results as to the direction of the association between smoking and AD".[101] Smoking has been found to contribute to dementia and cognitive decline,[102] reduced memory and cognitive abilities in adolescents,[103] and brain shrinkage (cerebral atrophy).[104][105]
Most notably, some studies have found that patients with Alzheimer's disease are more likely not to have smoked than the general population, which has been interpreted to suggest that smoking offers some protection against Alzheimer's. However, the research in this area is limited and the results are conflicting; some studies show that smoking increases the risk of Alzheimer's disease.[106] A recent review of the available scientific literature concluded that the apparent decrease in Alzheimer risk may be simply because smokers tend to die before reaching the age at which Alzheimer normally occurs. "Differential mortality is always likely to be a problem where there is a need to investigate the effects of smoking in a disorder with very low incidence rates before age 75 years, which is the case of Alzheimer's disease," it stated, noting that smokers are only half as likely as non-smokers to survive to the age of 80.[101]
Some older analyses have claimed that non-smokers are up to twice as likely as smokers to develop Alzheimer's disease.[107] However, a more current analyse found that most of the studies, which showed a preventing effect, had a close affiliation to the tobacco industry. Researches without tobacco lobby influence have concluded the complete opposite: Smokers are almost twice as likely as non smokers to develop Alzheimer's disease.[108]
Former and current smokers have a lower incidence of Parkinson's disease compared to people who have never smoked,[109][110] although the authors stated that it was more likely that the movement disorders which are part of Parkinson's disease prevented people from being able to smoke than that smoking itself was protective. Another study considered a possible role of nicotine in reducing Parkinson's risk: nicotine stimulates the dopaminergic system of the brain, which is damaged in Parkinson's disease, while other compounds in tobacco smoke inhibit MAO-B, an enzyme which produces oxidative radicals by breaking down dopamine.[111]
In many respects, nicotine acts on the nervous system in a similar way to caffeine. Some writings have stated that smoking can also increase mental concentration; one study documents a significantly better performance on the normed Advanced Raven Progressive Matrices test after smoking.[112]
Most smokers, when denied access to nicotine, exhibit symptoms such as irritability, jitteriness, dry mouth, and rapid heart beat.[113] The onset of these symptoms is very fast, nicotine's half-life being only 2 hours.. The psychological dependence may linger for months or even many years. Unlike some recreational drugs, nicotine does not measurably alter a smoker's motor skills, judgement, or language abilities while under the influence of the drug. Tobacco withdrawal has been shown to cause clinically significant distress.[114]
A very large percentage of schizophrenics smoke tobacco as a form of self-medication.[115][116][117][118] The high rate of tobacco use by the mentally ill is a major factor in their decreased life expectancy, which is about 25 years shorter than the general population.[119] Following the observation that smoking improves condition of people with schizophrenia, in particular working memory deficit, nicotine patches had been proposed as a way to treat schizophrenia.[120] Some studies suggest that a link exists between smoking and mental illness, citing the high incidence of smoking amongst those suffering from schizophrenia[121] and the possibility that smoking may alleviate some of the symptoms of mental illness,[122] but these have not been conclusive. In 2015, a meta-analysis found that smokers were at greater risk of developing psychotic illness.[123]
Recent studies have linked smoking to anxiety disorders, suggesting the correlation (and possibly mechanism) may be related to the broad class of anxiety disorders, and not limited to just depression. Current and ongoing research attempt to explore the addiction-anxiety relationship. Data from multiple studies suggest that anxiety disorders and depression play a role in cigarette smoking.[124] A history of regular smoking was observed more frequently among individuals who had experienced a major depressive disorder at some time in their lives than among individuals who had never experienced major depression or among individuals with no psychiatric diagnosis.[125] People with major depression are also much less likely to quit due to the increased risk of experiencing mild to severe states of depression, including a major depressive episode.[126] Depressed smokers appear to experience more withdrawal symptoms on quitting, are less likely to be successful at quitting, and are more likely to relapse.[127]
Pregnancy
A number of studies have shown that tobacco use is a significant factor in miscarriages among pregnant smokers, and that it contributes to a number of other threats to the health of the fetus. It slightly increases the risk of neural tube defects.[128]
Environmental tobacco smoke exposure and maternal smoking during pregnancy have been shown to cause lower infant birth weights.[129]
Studies have shown an association between prenatal exposure to environmental tobacco smoke and conduct disorder in children. As well, post-natal tobacco smoke exposure may cause similar behavioral problems in children.[130]
Women who smoke have about a 50% higher chance of giving birth to a child with behavioral disorders, such as ADHD, but a recent study in a book called "Attention Deficit Disorder: A Different Perception" overturns this, saying that ADHD is a genetic trait. Proof of this comes from a study showing that the people with ADHD had higher levels of certain hormones, as Thom Hartman explains with the hunter vs. farmer hypothesis.[131]
Drug interactions
Smoking is known to increase levels of liver enzymes that break down drugs and toxins. That means that drugs cleared by these enzymes are cleared more quickly in smokers, which may result in the drugs not working. Specifically, levels of CYP1A2 and CYP2A6 are induced:[132][133] substrates for 1A2 include caffeine and tricyclic antidepressants such as amitriptyline; substrates for 2A6 include the anticonvulsant, valproic acid.
Other harm
Studies suggest that smoking decreases appetite, but did not conclude that overweight people should smoke or that their health would improve by smoking. This is also a cause of heart diseases.[134] Smoking also decreases weight by overexpressing the gene AZGP1 which stimulates lipolysis.[135]
Smoking causes about 10% of the global burden of fire deaths,[136] and smokers are placed at an increased risk of injury-related deaths in general, partly due to also experiencing an increased risk of dying in a motor vehicle crash.[137]
Smoking increases the risk of symptoms associated with Crohn's disease (a dose-dependent effect with use of greater than 15 cigarettes per day).[138][139][140][141] There is some evidence for decreased rates of endometriosis in infertile smoking women,[142] although other studies have found that smoking increases the risk in infertile women.[143] There is little or no evidence of a protective effect in fertile women. Some preliminary data from 1996 suggested a reduced incidence of uterine fibroids,[144] but overall the evidence is unconvincing.[145]
Current research shows that tobacco smokers who are exposed to residential radon are twice as likely to develop lung cancer as non-smokers.[146] As well, the risk of developing lung cancer from asbestos exposure is twice as likely for smokers than for non-smokers.[147]
New research has found that women who smoke are at significantly increased risk of developing an abdominal aortic aneurysm, a condition in which a weak area of the abdominal aorta expands or bulges, and is the most common form of aortic aneurysm.[148]
Smoking leads to an increased risk of bone fractures, especially hip fractures.[149] It also leads to slower wound-healing after surgery, and an increased rate of postoperative healing complication.[150]
Benefits
In addition to the numerous documented negative health effects of smoking, several types of "smoker's paradoxes" (cases where smoking appears to have specific beneficial effects) have been observed.[151] Smoking may prevent Parkinson's disease.[152]
Mechanism
Chemical carcinogens
Smoke, or any partially burnt organic matter, contains carcinogens (cancer-causing agents). The potential effects of smoking, such as lung cancer, can take up to 20 years to manifest themselves. Historically, women began smoking en masse later than men, so an increased death rate caused by smoking amongst women did not appear until later. The male lung cancer death rate decreased in 1975 — roughly 20 years after the initial decline in cigarette consumption in men. A fall in consumption in women also began in 1975[154] but by 1991 had not manifested in a decrease in lung cancer-related mortalities amongst women.[155]
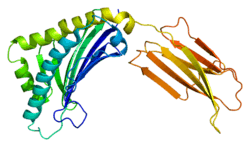
Smoke contains several carcinogenic pyrolytic products that bind to DNA and cause genetic mutations. Particularly potent carcinogens are polycyclic aromatic hydrocarbons (PAH), which are toxicated to mutagenic epoxides. The first PAH to be identified as a carcinogen in tobacco smoke was benzopyrene, which has been shown to toxicate into an epoxide that irreversibly attaches to a cell's nuclear DNA, which may either kill the cell or cause a genetic mutation. If the mutation inhibits programmed cell death, the cell can survive to become a cancer cell. Similarly, acrolein, which is abundant in tobacco smoke, also irreversibly binds to DNA, causes mutations and thus also cancer. However, it needs no activation to become carcinogenic.[156]
There are over 19 known carcinogens in cigarette smoke.[157] The following are some of the most potent carcinogens:
- Polycyclic aromatic hydrocarbons are tar components produced by pyrolysis in smoldering organic matter and emitted into smoke. Several of these PAH's are already toxic in their normal form, however, many of then can become more toxic to the liver. Due to the hydrophobic nature of PAH's they do not dissolve in water and are hard to expel from the body. In order to make the PAH more soluble in water, the liver creates an enzyme called Cytochrome P450 which adds an additional oxygen to the PAH, turning it into a mutagenic epoxides, which is more soluble, but also more reactive.[158] The first PAH to be identified as a carcinogen in tobacco smoke was benzopyrene, which been shown to toxicate into a diol epoxide and then permanently attach to nuclear DNA, which may either kill the cell or cause a genetic mutation. The DNA contains the information on how the cell function; in practice, it contains the recipes for protein synthesis. If the mutation inhibits programmed cell death, the cell can survive to become a cancer cell, a cell that does not function like a normal cell. The carcinogenicity is radiomimetic, i.e. similar to that produced by ionizing nuclear radiation. Tobacco manufacturers have experimented with combustion less vaporizer technology to allow cigarettes to be consumed without the formation of carcinogenic benzopyrenes.[159] Although such products have become increasingly popular, they still represent a very small fraction of the market, and no conclusive evidence has shown to prove or disprove the positive health claims.
- Acrolein is a pyrolysis product that is abundant in cigarette smoke. It gives smoke an acrid smell and an irritating, lachrymatory effect and is a major contributor to its carcinogenicity. Like PAH metabolites, acrolein is also an electrophilic alkylating agent and permanently binds to the DNA base guanine, by a conjugate addition followed by cyclization into a hemiaminal. The acrolein-guanine adduct induces mutations during DNA copying and thus causes cancers in a manner similar to PAHs. However, acrolein is 1000 times more abundant than PAHs in cigarette smoke and is able to react as is, without metabolic activation. Acrolein has been shown to be a mutagen and carcinogen in human cells. The carcinogenicity of acrolein has been difficult to study by animal experimentation, because it has such a toxicity that it tends to kill the animals before they develop cancer.[156] Generally, compounds able to react by conjugate addition as electrophiles (so-called Michael acceptors after Michael reaction) are toxic and carcinogenic, because they can permanently alkylate DNA, similarly to mustard gas or aflatoxin. Acrolein is only one of them present in cigarette smoke; for example, crotonaldehyde has been found in cigarette smoke.[160] Michael acceptors also contribute to the chronic inflammation present in tobacco disease.[52]
- Nitrosamines are a group of carcinogenic compounds found in cigarette smoke but not in uncured tobacco leaves. Nitrosamines form on flue-cured tobacco leaves during the curing process through a chemical reaction between nicotine and other compounds contained in the uncured leaf and various oxides of nitrogen found in all combustion gasses. Switching to Indirect fire curing has been shown to reduce nitrosamine levels to less than 0.1 parts per million.[161][162]
Sidestream tobacco smoke, or exhaled mainstream smoke, is particularly harmful. Because exhaled smoke exists at lower temperatures than inhaled smoke, chemical compounds undergo changes which can cause them to become more dangerous. As well, smoke undergoes changes as it ages, which causes the transformation of the compound NO into the more toxic NO2. Further, volatilization causes smoke particles to become smaller, and thus more easily embedded deep into the lung of anyone who later breathes the air.[163]
Radioactive carcinogens
In addition to chemical, nonradioactive carcinogens, tobacco and tobacco smoke contain small amounts of lead-210(210Pb) and polonium-210 (210Po) both of which are radioactive carcinogens. The presence of polonium-210 in mainstream cigarette smoke has been experimentally measured at levels of 0.0263–0.036 pCi (0.97–1.33 mBq),[164][165] which is equivalent to about 0.1 pCi per milligram of smoke (4 mBq/mg); or about 0.81 pCi of lead-210 per gram of dry condensed smoke (30 Bq/kg).
Research by NCAR radiochemist Ed Martell suggested that radioactive compounds in cigarette smoke are deposited in "hot spots" where bronchial tubes branch, that tar from cigarette smoke is resistant to dissolving in lung fluid and that radioactive compounds have a great deal of time to undergo radioactive decay before being cleared by natural processes. Indoors, these radioactive compounds can linger in secondhand smoke, and greater exposure would occur when these radioactive compounds are inhaled during normal breathing, which is deeper and longer than when inhaling cigarettes. Damage to the protective epithelial tissue from smoking only increases the prolonged retention of insoluble polonium-210 compounds produced from burning tobacco. Martell estimated that a carcinogenic radiation dose of 80–100 rads is delivered to the lung tissue of most smokers who die of lung cancer.[166][167][168]
Smoking an average of 1.5 packs per day gives a radiation dose of 60-160 mSv/year,[169][170] compared with living near a nuclear power station (0.0001 mSv/year)[171][172] or the 3.0 mSv/year average dose for Americans.[172][173] Some of the mineral apatite in Florida used to produce phosphate for U.S.A. tobacco crops contains uranium, radium, lead-210 and polonium-210 and radon.[174][175] The radioactive smoke from tobacco fertilized this way is deposited in lungs and releases radiation even if a smoker quits the habit. The combination of carcinogenic tar and radiation in a sensitive organ such as lungs increases the risk of cancer.
In contrast, a 1999 review of tobacco smoke carcinogens published in the Journal of the National Cancer Institute states that "levels of polonium-210 in tobacco smoke are not believed to be great enough to significantly impact lung cancer in smokers."[176] In 2011 Hecht has also stated that the "levels of 210Po in cigarette smoke are probably too low to be involved in lung cancer induction ..."[177]
Nicotine

Nicotine, which is contained in cigarettes and other smoked tobacco products, is a stimulant and is one of the main factors leading to continued tobacco smoking. Nicotine is a highly addictive psychoactive chemical. When tobacco is smoked, most of the nicotine is pyrolyzed; a dose sufficient to cause mild somatic dependency and mild to strong psychological dependency remains. The amount of nicotine absorbed by the body from smoking depends on many factors, including the type of tobacco, whether the smoke is inhaled, and whether a filter is used. There is also a formation of harmane (a MAO inhibitor) from the acetaldehyde in cigarette smoke, which seems to play an important role in nicotine addiction[178] probably by facilitating dopamine release in the nucleus accumbens in response to nicotine stimuli. According to studies by Henningfield and Benowitz, nicotine is more addictive than cannabis, caffeine, ethanol, cocaine, and heroin when considering both somatic and psychological dependence. However, due to the stronger withdrawal effects of ethanol, cocaine and heroin, nicotine may have a lower potential for somatic dependence than these substances.[179][180] About half of Canadians who currently smoke have tried to quit.[181] McGill University health professor Jennifer O'Loughlin stated that nicotine addiction can occur as soon as five months after the start of smoking.[182]
Ingesting a compound by smoking is one of the most rapid and efficient methods of introducing it into the bloodstream, second only to injection, which allows for the rapid feedback which supports the smokers' ability to titrate their dosage. On average it takes about ten seconds for the substance to reach the brain. As a result of the efficiency of this delivery system, many smokers feel as though they are unable to cease. Of those who attempt cessation and last three months without succumbing to nicotine, most are able to remain smoke-free for the rest of their lives.[183] There exists a possibility of depression in some who attempt cessation, as with other psychoactive substances. Depression is also common in teenage smokers; teens who smoke are four times as likely to develop depressive symptoms as their nonsmoking peers.[184]
Although nicotine does play a role in acute episodes of some diseases (including stroke, impotence, and heart disease) by its stimulation of adrenaline release, which raises blood pressure,[62] heart and respiration rate, and free fatty acids, the most serious longer term effects are more the result of the products of the smouldering combustion process. This has led to the development of various nicotine delivery systems, such as the nicotine patch or nicotine gum, that can satisfy the addictive craving by delivering nicotine without the harmful combustion by-products. This can help the heavily dependent smoker to quit gradually, while discontinuing further damage to health.
Recent evidence has shown that smoking tobacco increases the release of dopamine in the brain, specifically in the mesolimbic pathway, the same neuro-reward circuit activated by drugs of abuse such as heroin and cocaine. This suggests nicotine use has a pleasurable effect that triggers positive reinforcement.[185] One study found that smokers exhibit better reaction-time and memory performance compared to non-smokers, which is consistent with increased activation of dopamine receptors.[186] Neurologically, rodent studies have found that nicotine self-administration causes lowering of reward thresholds—a finding opposite that of most other drugs of abuse (e.g. cocaine and heroin). This increase in reward circuit sensitivity persisted months after the self-administration ended, suggesting that nicotine's alteration of brain reward function is either long lasting or permanent. Furthermore, it has been found that nicotine can activate long-term potentiation in vivo and in vitro. These studies suggest nicotine’s "trace memory" may contribute to difficulties in nicotine abstinence.
The carcinogenity of tobacco smoke is not explained by nicotine per se, which is not carcinogenic or mutagenic, although it is a metabolic precursor for several compounds which are. In addition, it inhibits apoptosis, therefore accelerating existing cancers.[187] Also, NNK, a nicotine derivative converted from nicotine, can be carcinogenic.
It is worth noting that nicotine, although frequently implicated in producing tobacco addiction, is not significantly addictive when administered alone.[188] The addictive potential manifests itself after co-administration of an MAOI, which specifically causes sensitization of the locomotor response in rats, a measure of addictive potential.[189]
Forms of exposure
Second-hand smoke

Second-hand smoke is a mixture of smoke from the burning end of a cigarette, pipe or cigar, and the smoke exhaled from the lungs of smokers. It is involuntarily inhaled, lingers in the air hours after cigarettes have been extinguished, and may cause a wide range of adverse health effects, including cancer, respiratory infections and asthma.[190] Non-smokers who are exposed to second-hand smoke at home or work are thought, due to a wide variety of statistical studies, to increase their heart disease risk by 25–30% and their lung cancer risk by 20–30%. Second-hand smoke has been estimated to cause 38,000 deaths per year, of which 3,400 are deaths from lung cancer in non-smokers.[191]
The current US Surgeon General’s Report concludes that there is no established risk-free level of exposure to second-hand smoke. Short exposures to second-hand smoke are believed to cause blood platelets to become stickier, damage the lining of blood vessels, decrease coronary flow velocity reserves, and reduce heart rate variability, potentially increasing the risk of heart attack. New research indicates that private research conducted by cigarette company Philip Morris in the 1980s showed that second-hand smoke was toxic, yet the company suppressed the finding during the next two decades.[190]
Chewing tobacco
Chewing tobacco has been known to cause cancer, particularly of the mouth and throat.[192] According to the International Agency for Research on Cancer, "Some health scientists have suggested that smokeless tobacco should be used in smoking cessation programmes and have made implicit or explicit claims that its use would partly reduce the exposure of smokers to carcinogens and the risk for cancer. These claims, however, are not supported by the available evidence."[192] Oral and spit tobacco increase the risk for leukoplakia a precursor to oral cancer.[193]
Cigars
Like other forms of smoking, cigar smoking poses a significant health risk depending on dosage: risks are greater for those who inhale more when they smoke, smoke more cigars, or smoke them longer.[194] The risk of dying from any cause is significantly greater for cigar smokers, with the risk particularly higher for smokers less than 65 years old, and with risk for moderate and deep inhalers reaching levels similar to cigarette smokers.[195] The increased risk for those smoking 1–2 cigars per day is too small to be statistically significant,[196] and the health risks of the 3/4 of cigar smokers who smoke less than daily are not known[197] and are hard to measure. Although it has been claimed that people who smoke few cigars have no increased risk, a more accurate statement is that their risks are proportionate to their exposure.[59] Health risks are similar to cigarette smoking in nicotine addiction, periodontal health, tooth loss, and many types of cancer, including cancers of the mouth, throat, and esophagus. Cigar smoking also can cause cancers of the lung and larynx, where the increased risk is less than that of cigarettes. Many of these cancers have extremely low cure rates. Cigar smoking also increases the risk of lung and heart diseases such as chronic obstructive pulmonary disease.[194]
Hookahs
A common belief among users is that the smoke of a hookah (waterpipe, narghile) is significantly less dangerous than that from cigarettes.[198] The water moisture induced by the hookah makes the smoke less irritating and may give a false sense of security and reduce concerns about true health effects.[199] Doctors at institutions including the Mayo Clinic have stated that use of hookah can be as detrimental to a person's health as smoking cigarettes,[200][201] and a study by the World Health Organization also confirmed these findings.[202]
Each hookah session typically lasts more than 40 minutes, and consists of 50 to 200 inhalations that each range from 0.15 to 0.50 liters of smoke.[203][204] In an hour-long smoking session of hookah, users consume about 100 to 200 times the smoke of a single cigarette;[203][205] A study in the Journal of Periodontology found that water pipe smokers were marginally more likely than regular smokers to show signs of gum disease, showing rates 5-fold higher than non-smokers rather than the 3.8-fold risk that regular smokers show.[206] According to USA Today, people who smoked water pipes had five times the risk of lung cancer of non-smokers.[207]
A study on hookah smoking and cancer in Pakistan was published in 2008. Its objective was "to find serum CEA levels in ever/exclusive hookah smokers, i.e. those who smoked only hookah (no cigarettes, bidis, etc.), prepared between 1 and 4 times a day with a quantity of up to 120 g of a tobacco-molasses mixture each (i.e. the tobacco weight equivalent of up to 60 cigarettes of 1 g each) and consumed in 1 to 8 sessions". Carcinoembryonic antigen (CEA) is a marker found in several forms of cancer. Levels in exclusive hookah smokers were lower compared to cigarette smokers although the difference was not as statistically significant as that between a hookah smoker and a non-smoker. Also, the study concluded that heavy hookah smoking (2–4 daily preparations; 3–8 sessions a day ; >2 hrs to ≤ 6 hours) substantially raises CEA levels.[208] Hookah smokers were nearly 6 times more likely to develop lung cancer as compared to healthy non-smokers in Kashmir (India).[209]
Dipping tobacco
Dipping tobacco, commonly referred to as snuff, is also put in the mouth, but it is a flavored powder. it is placed between the cheek and gum. Dipping tobacco doesn't need to be chewed for the nicotine to be absorbed into your body. First-time users of these products often become nauseated and dizzy. Long-term effects include bad breath, yellowed teeth, and an increased risk of oral cancer.
Users of dipping tobacco are believed to face less risk of some cancers than smokers but are still at greater risk than people who do not use any tobacco products.[210] They also have an equal risk of other health problems directly linked to nicotine such as increased rate of atherosclerosis.
Prevention
Education and counselling by physicians of children and adolescents has been found to be effective in decreasing the risk of tobacco use.[211]
Usage

Though tobacco may be consumed by either smoking or other smokeless methods such as chewing, the World Health Organization (WHO) only collects data on smoked tobacco.[1] Smoking has therefore been studied more extensively than any other form of tobacco consumption.[2]
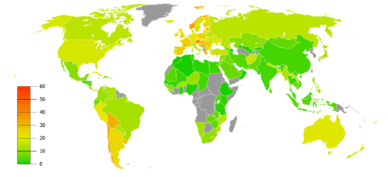
In 2000, smoking was practiced by 1.22 billion people, predicted to rise to 1.45 billion people in 2010 and 1.5 to 1.9 billion by 2025. If prevalence had decreased by 2% a year since 2000 this figure would have been 1.3 billion in 2010 and 2025.[212] Despite dropping by 0.4 percent from 2009 to 2010, the United States still reports an average of 17.9 percent usage.[34]
As of 2002, about twenty percent of young teens (13–15) smoke worldwide, with 80,000 to 100,000 children taking up the addiction every day—roughly half of whom live in Asia. Half of those who begin smoking in adolescent years are projected to go on to smoke for 15 to 20 years.[213]
The WHO states that "Much of the disease burden and premature mortality attributable to tobacco use disproportionately affect the poor". Of the 1.22 billion smokers, 1 billion of them live in developing or transitional nations. Rates of smoking have leveled off or declined in the developed world.[214] In the developing world, however, tobacco consumption is rising by 3.4% per year as of 2002.[213]
The WHO in 2004 projected 58.8 million deaths to occur globally,[215]:8 from which 5.4 million are tobacco-attributed,[215]:23 and 4.9 million as of 2007.[216] As of 2002, 70% of the deaths are in developing countries.[216]
The shift in prevalence of tobacco smoking to a younger demographic, mainly in the developing world, can be attributed to several factors. The tobacco industry spends up to $12.5 billion annually on advertising, which is increasingly geared towards adolescents in the developing world because they are a very vulnerable audience for the marketing campaigns. Adolescents have more difficulty understanding the long-term health risks that are associated with smoking and are also more easily influenced by "images of romance, success, sophistication, popularity, and adventure which advertising suggests they could achieve through the consumption of cigarettes". This shift in marketing towards adolescents and even children in the tobacco industry is debilitating to organizations’ and countries’ efforts to improve child health and mortality in the developing world. It reverses or halts the effects of the work that has been done to improve health care in these countries, and although smoking is deemed as a "voluntary" health risk, the marketing of tobacco towards very impressionable adolescents in the developing world makes it less of a voluntary action and more of an inevitable shift.[14]
Many government regulations have been passed to protect citizens from harm caused by public environmental tobacco smoke. The "Pro-Children Act of 2001" prohibits smoking within any facility that provides health care, day care, library services, or elementary and secondary education to children in the USA.[217] On May 23, 2011, New York City enforced a smoking ban for all parks, beaches, and pedestrian malls in an attempt to eliminate threats posed to civilians by environmental tobacco smoke.[218]
History
Concern about health effects of tobacco has a long history. Gideon Lincecum, an American naturalist and practitioner of botanical medicine, wrote in the early 19th century on tobacco: "This poisonous plant has been used a great deal as a medicine by the old school faculty, and thousands have been slain by it. ... It is a very dangerous article, and use it as you will, it always diminishes the vital energies in exact proportion to the quantity used - it may be slowly, but it is very sure."[219]
The late-19th-century invention of automated cigarette-making machinery in the American South made it possible to mass-produce cigarettes at low cost, and cigarettes became elegant and fashionable among society men as the Victorian era gave way to the Edwardian. In 1912, American Dr. Isaac Adler was the first to strongly suggest that lung cancer is related to smoking.[220] In 1924, economist Irving Fisher wrote an anti-smoking article for the Readers Digest, which said "... tobacco lowers the whole tone of the body and decreases its vital power and resistance ... tobacco acts like a narcotic poison, like opium, and like alcohol, though usually in a less degree".[221] In 1929, Fritz Lickint of Dresden, Germany, published a formal statistical evidence of a lung cancer-tobacco link, based on a study showing that lung cancer sufferers were likely to be smokers.[222] Lickint also argued that tobacco use was the best way to explain the fact that lung cancer struck men four or five times more often than women (since women smoked much less).[222]
Prior to World War I, lung cancer was considered to be a rare disease, which most physicians would never see during their career.[21][223] With the postwar rise in popularity of cigarette smoking, however, came an epidemic of lung cancer.
In 1950, Richard Doll and Austin Bradford Hill published research in the British Medical Journal showing a close link between smoking and lung cancer.[3] Four years later, in 1954, the British Doctors Study, a study of some 40,000 doctors over 20 years, confirmed the suggestion, based on which the government issued advice that smoking and lung cancer rates were related.[4] The British Doctors Study lasted until 2001, with results published every ten years and final results published in 2004 by Doll and Richard Peto.[5] Much early research was also done by Alton Ochsner. Reader's Digest magazine for many years published frequent anti-smoking articles. On January 11, 1964, the United States Surgeon General's Report on Smoking and Health was published; this led millions of American smokers to quit, the banning of certain advertising, and the requirement of warning labels on tobacco products.
Studies
In the 1930s German scientists showed that cigarette smoking caused lung cancer.[224] In 1938 a study in the USA by a Johns Hopkins University scientist suggested a strongly negative correlation between smoking and lifespan. In 1950 five studies were published in which "smoking was powerfully implicated in the causation of lung cancer".[225] These included the now classic paper "Smoking and Carcinoma of the Lung" which appeared in the British Medical Journal. This paper reported that "heavy smokers were fifty times as likely as non-smokers to contract lung cancer".[3][225]
In 1953, scientists at the Sloan-Kettering Institute in New York City demonstrated that cigarette tar painted on the skin of mice caused fatal cancers.[224] This work attracted much media attention; the New York Times and Life both covered the issue. The Reader's Digest published an article entitled "Cancer by the Carton".[224]:14
A team of British scientists headed by Richard Doll carried out a longitudinal study of 34,439 medical specialists from 1951 to 2001, generally called the "British Doctors Study."[5] The study demonstrated that about half of the persistent cigarette smokers born in 1900–1909 were eventually killed by their addiction (calculated from the logarithms of the probabilities of surviving from 35–70, 70–80, and 80–90) and about two thirds of the persistent cigarette smokers born in the 1920s would eventually be killed by their addiction.
The health effects of smoking have been significant for the development of the science of epidemiology. As the mechanism of carcinogenicity is radiomimetic or radiological, the effects are stochastic. Definite statements can be made only on the relative increased or decreased probabilities of contracting a given disease. For a particular individual, it is impossible to definitively prove a direct causal link between exposure to a radiomimetic poison such as tobacco smoke and the cancer that follows; such statements can only be made at the aggregate population level. Tobacco companies have capitalized on this philosophical objection and exploited the doubts of clinicians, who consider only individual cases, on the causal link in the stochastic expression of the toxicity as actual disease.[226]
There have been multiple court cases on the issue that tobacco companies have researched the health effects of tobacco, but suppressed the findings or formatted them to imply lessened or no hazard.[226]
The term "smoker" is given to a person who habitually smokes tobacco on a daily basis. This category has been the focus of the vast majority of tobacco studies. However, the health effects of less-than-daily smoking are far less well understood. Studies have often taken the data of "occasional smokers" (those who have never smoked daily) and grouped them with those who have never smoked.[227] A 2006 European study on occasional smoking published findings that the risk of the major smoking-related cancers for occasional smokers was 1.24 times that of those who have never smoked at all but the result was not statistically significant. (For a confidence interval of 95%, this data showed an incidence rate ratio of 0.80 to 1.94.)[227] (Data reduction used Cox proportional hazard model, stratified by gender and country.) This compares to studies showing that habitual heavy smokers have greater than 50 times the incidence of smoking-related cancers.
After a ban on smoking in all enclosed public places was introduced in Scotland in March 2006, there was a 17 percent reduction in hospital admissions for acute coronary syndrome. 67% of the decrease occurred in non-smokers.[228]
A study published in the journal Pediatrics refers to the danger posed by what the authors call "third-hand smoke" — toxic substances that remain in areas where smoking has recently occurred.[229]
See also
References
- 1 2 "Prevalence of current tobacco use among adults aged=15 years (percentage)". World Health Organization. Retrieved 2009-01-02.
- 1 2 "Mayo report on addressing the worldwide tobacco epidemic through effective, evidence-based treatment". World Health Organization. p. 2. Retrieved 2009-01-02.
- 1 2 3 Doll R, Hill AB (Sep 1950). "Smoking and carcinoma of the lung; preliminary report". British Medical Journal. 2 (4682): 739–748. PMC 2038856
 . PMID 14772469. doi:10.1136/bmj.2.4682.739.
. PMID 14772469. doi:10.1136/bmj.2.4682.739. - 1 2 Doll R, Hill AB (Jun 2004). "The mortality of doctors in relation to their smoking habits: a preliminary report. 1954". BMJ. 328 (7455): 1529–33; discussion 1533. PMC 437141
 . PMID 15217868. doi:10.1136/bmj.328.7455.1529.
. PMID 15217868. doi:10.1136/bmj.328.7455.1529. - 1 2 3 4 5 6 Doll R, Peto R, Boreham J, Sutherland I (Jun 2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (7455): 1519. PMC 437139
 . PMID 15213107. doi:10.1136/bmj.38142.554479.AE.
. PMID 15213107. doi:10.1136/bmj.38142.554479.AE. - 1 2 World Health Organization (2008). WHO Report on the Global Tobacco Epidemic 2008: The MPOWER Package (PDF). Geneva: World Health Organization. p. 8. ISBN 92-4-159628-7.
- 1 2 3 4 5 6 "Tobacco Fact sheet N°339". May 2014. Retrieved 13 May 2015.
- ↑ "The top 10 causes of death". Retrieved 13 May 2015.
- ↑ "Nicotine: A Powerful Addiction." Centers for Disease Control and Prevention.
- ↑ Vainio H (Jun 1987). "Is passive smoking increasing cancer risk?". Scandinavian Journal of Work, Environment & Health. 13 (3): 193–6. PMID 3303311. doi:10.5271/sjweh.2066.
- ↑ "The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General" (PDF). Atlanta, U.S., page 93: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2006. Retrieved 2009-02-15.
- 1 2 Peate I (2005). "The effects of smoking on the reproductive health of men". British Journal of Nursing. 14 (7): 362–6. PMID 15924009. doi:10.12968/bjon.2005.14.7.17939.
- ↑ Korenman, Stanley G. (2004). "Epidemiology of erectile dysfunction". Endocrine. 23 (2–3): 87–91. ISSN 1355-008X. PMID 15146084. doi:10.1385/ENDO:23:2-3:087. Retrieved 5 November 2016.
- 1 2 Nichter M, Cartwright E; Cartwright (1991). "Saving the Children for the Tobacco Industry". Medical Anthropology Quarterly. 5 (3): 236–56. JSTOR 648675. doi:10.1525/maq.1991.5.3.02a00040.
- ↑ Nutt, D; King, LA; Saulsbury, W; Blakemore, C (24 March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse.". Lancet. 369 (9566): 1047–53. PMID 17382831. doi:10.1016/s0140-6736(07)60464-4.
- ↑ ASPA. "Health Effects of Tobacco". Retrieved 8 September 2014.
- ↑ "Life Expectancy at Age 30: Nonsmoking Versus Smoking Men". Tobacco Documents Online. Retrieved 2012-05-06.
- ↑ Ferrucci L, Izmirlian G, Leveille S, Phillips CL, Corti MC, Brock DB, Guralnik JM (Apr 1999). "Smoking, physical activity, and active life expectancy". American Journal of Epidemiology. 149 (7): 645–653. PMID 10192312. doi:10.1093/oxfordjournals.aje.a009865.
- ↑ Doll R, Peto R, Wheatley K, Gray R, Sutherland I (Oct 1994). "Mortality in relation to smoking: 40 years' observations on male British doctors". BMJ. 309 (6959): 901–11. PMC 2541142
 . PMID 7755693. doi:10.1136/bmj.309.6959.901.
. PMID 7755693. doi:10.1136/bmj.309.6959.901. - ↑ Villeneuve PJ, Mao Y (1994). "Lifetime probability of developing lung cancer, by smoking status, Canada". Canadian Journal of Public Health. 85 (6): 385–8. PMID 7895211.
- 1 2 Witschi H (Nov 2001). "A short history of lung cancer". Toxicological Sciences. 64 (1): 4–6. PMID 11606795. doi:10.1093/toxsci/64.1.4.
- ↑ Adler I. Primary malignant growths of the lungs and bronchi. New York: Longmans, Green, and Company; 1912., cited in Spiro SG, Silvestri GA (Sep 2005). "One hundred years of lung cancer". American Journal of Respiratory and Critical Care Medicine. 172 (5): 523–9. PMID 15961694. doi:10.1164/rccm.200504-531OE.
- ↑ "Benefits of Quitting - American Lung Association". Stop Smoking. American Lung Association. Retrieved 2012-05-06.
- ↑ "Light Cigarettes and Cancer Risk". National Cancer Institute. Retrieved 8 September 2014.
- ↑ Rizzuto, D; Fratiglioni, L (2014). "Lifestyle factors related to mortality and survival: a mini-review.". Gerontology. 60 (4): 327–35. PMID 24557026. doi:10.1159/000356771.
- ↑ Samet, JM (May 2013). "Tobacco smoking: the leading cause of preventable disease worldwide.". Thoracic surgery clinics. 23 (2): 103–12. PMID 23566962. doi:10.1016/j.thorsurg.2013.01.009.
- ↑ Centers for Disease Control and Prevention (CDC) (Apr 2002). "Annual smoking-attributable mortality, years of potential life lost, and economic costs--United States, 1995-1999". MMWR. Morbidity and Mortality Weekly Report. 51 (14): 300–3. PMID 12002168.
- ↑ Streppel MT, Boshuizen HC, Ocké MC, Kok FJ, Kromhout D (2007). "Mortality and life expectancy in relation to long-term cigarette, cigar and pipe smoking: the Zutphen Study". Tob Control. 16: 107–13. PMC 2598467
 . PMID 17400948. doi:10.1136/tc.2006.017715.
. PMID 17400948. doi:10.1136/tc.2006.017715. - ↑ http://www.nyc.gov/html/doh/downloads/pdf/chi/chi24-4-pktguide.pdf
- ↑ "HEALTH | Cigarettes 'cut life by 11 minutes'". BBC News. 1999-12-31. Retrieved 2012-03-25.
- ↑ "Time for a smoke? One cigarette reduces your life by 11 minutes". BMJ. Retrieved 2012-03-25.
- ↑ Mamun AA, Peeters A, Barendregt J, Willekens F, Nusselder W, Bonneux L (Mar 2004). "Smoking decreases the duration of life lived with and without cardiovascular disease: a life course analysis of the Framingham Heart Study". European Heart Journal. 25 (5): 409–415. PMID 15033253. doi:10.1016/j.ehj.2003.12.015.
- ↑ Thun MJ, Day-Lally CA, Calle EE, Flanders WD, Heath CW (Sep 1995). "Excess mortality among cigarette smokers: changes in a 20-year interval". American Journal of Public Health. 85 (9): 1223–30. PMC 1615570
 . PMID 7661229. doi:10.2105/AJPH.85.9.1223.
. PMID 7661229. doi:10.2105/AJPH.85.9.1223. - 1 2 "America’s Health Rankings - 2011" (PDF). United Health Foundation. December 2011. p. 12.
- ↑ Centers for Disease Control and Prevention (CDC) (Nov 2008). "Smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000-2004". MMWR. Morbidity and Mortality Weekly Report. 57 (45): 1226–8. PMID 19008791.
- ↑ Never Say Die, an ABC News special by Peter Jennings 6/27/1996
- ↑ "21st Century Could See a Billion Tobacco Victims" (PDF). Tobacco News Flash. Tobacco-Free Missouri Coalition. 3 (12): 1. 2007. Retrieved 2012-05-06.
- ↑ Carter BD, Abnet CC, Feskanich D, Freedman ND, Hartge P, Lewis CE, Ockene JK, Prentice RL, Speizer FE, Thun MJ, Jacobs EJ (Feb 2015). "Smoking and mortality--beyond established causes". The New England Journal of Medicine. 372 (7): 631–640. PMID 25671255. doi:10.1056/NEJMsa1407211.
- ↑ "Lung Cancer and Smoking" (PDF). Fact Sheet. www.LegacyForHealth.org. 2010-11-23. Retrieved 2012-05-06.
- ↑ Lipworth L, Tarone RE, McLaughlin JK (Dec 2006). "The epidemiology of renal cell carcinoma". The Journal of Urology. 176 (6 Pt 1): 2353–2358. PMID 17085101. doi:10.1016/j.juro.2006.07.130.
- ↑ "Risks and causes of laryngeal cancer". Cancer Research UK. Retrieved 21 June 2015.
- ↑ "Head and Neck Cancer: Risk Factors and Prevention". ASCO. Retrieved 21 June 2015.
- ↑ Boffetta P (Sep 2008). "Tobacco smoking and risk of bladder cancer". Scandinavian Journal of Urology and Nephrology. Supplementum. 42 (218): 45–54. PMID 18815916. doi:10.1080/03008880802283664.
- ↑ "Esophagus Cancer". American Cancer Society. 2011-08-11. Retrieved 2012-05-06.
- ↑ Iodice S, Gandini S, Maisonneuve P, Lowenfels AB (Jul 2008). "Tobacco and the risk of pancreatic cancer: a review and meta-analysis". Langenbeck's Archives of Surgery / Deutsche Gesellschaft Für Chirurgie. 393 (4): 535–545. PMID 18193270. doi:10.1007/s00423-007-0266-2.
- 1 2 Kuper H, Boffetta P, Adami HO (Sep 2002). "Tobacco use and cancer causation: association by tumour type". Journal of Internal Medicine. 252 (3): 206–224. PMID 12270001. doi:10.1046/j.1365-2796.2002.01022.x.
- ↑ Vineis, P; Alavanja, M; Buffler, P; Fontham, E; Franceschi, S; Gao, YT; Gupta, PC; Hackshaw, A; Matos, E; Samet, J; Sitas, F; Smith, J; Stayner, L; Straif, K; Thun, MJ; Wichmann, HE; Wu, AH; Zaridze, D; Peto, R; Doll, R (21 January 2004). "Tobacco and cancer: recent epidemiological evidence.". Journal of the National Cancer Institute. 96 (2): 99–106. PMID 14734699. doi:10.1093/jnci/djh014.
- ↑ Sasco, A.J.; Secretan, M.B.; Straif, K. (August 2004). "Tobacco smoking and cancer: a brief review of recent epidemiological evidence". Lung Cancer. 45: S3–S9. PMID 15552776. doi:10.1016/j.lungcan.2004.07.998.
- ↑ "What are the risk factors for breast cancer?". American Cancer Society. Retrieved 31 May 2015.
- ↑ Thun MJ, Hannan LM, Adams-Campbell LL, Boffetta P, Buring JE, Feskanich D, Flanders WD, Jee SH, Katanoda K, Kolonel LN, Lee IM, Marugame T, Palmer JR, Riboli E, Sobue T, Avila-Tang E, Wilkens LR, Samet JM (Sep 2008). "Lung cancer occurrence in never-smokers: an analysis of 13 cohorts and 22 cancer registry studies". PLoS Medicine. 5 (9): e185. PMC 2531137
 . PMID 18788891. doi:10.1371/journal.pmed.0050185.
. PMID 18788891. doi:10.1371/journal.pmed.0050185. - ↑ Devereux G (May 2006). "ABC of chronic obstructive pulmonary disease. Definition, epidemiology, and risk factors". BMJ. 332 (7550): 1142–1144. PMC 1459603
 . PMID 16690673. doi:10.1136/bmj.332.7550.1142.
. PMID 16690673. doi:10.1136/bmj.332.7550.1142. - 1 2 Facchinetti F, Amadei F, Geppetti P, Tarantini F, Di Serio C, Dragotto A, Gigli PM, Catinella S, Civelli M, Patacchini R (Nov 2007). "Alpha, beta-unsaturated aldehydes in cigarette smoke release inflammatory mediators from human macrophages". American Journal of Respiratory Cell and Molecular Biology. 37 (5): 617–623. PMID 17600310. doi:10.1165/rcmb.2007-0130OC.
- ↑ Glantz, SA; Parmley, WW (5 April 1995). "Passive smoking and heart disease. Mechanisms and risk.". JAMA. 273 (13): 1047–53. PMID 7897790. doi:10.1001/jama.1995.03520370089043.
- ↑ Shah, Reena S; Cole, John W (July 2010). "Smoking and stroke: the more you smoke the more you stroke". Expert Review of Cardiovascular Therapy. 8 (7): 917–932. doi:10.1586/erc.10.56.
- ↑ "How Does Smoking Affect the Heart and Blood Vessels?". NHLBI. Retrieved 9 September 2015.
- ↑ "Health : Young smokers' heart attack risk". BBC. 2004-08-24. Retrieved 2005-12-18.
- ↑ "Cigarette Smoke Changes Heart's Shape". InfoNIAC.com. Retrieved 2009-01-10.
- ↑ Joyce JW (May 1990). "Buerger's disease (thromboangiitis obliterans)". Rheumatic Diseases Clinics of North America. 16 (2): 463–70. PMID 2189162.
- 1 2 Burns DM (1998). "Cigar smoking: overview and current state of the science" (PDF). In Shopland DR, Burns DM, Hoffmann D, Cummings KM, Amacher RH. Cigars: Health Effects and Trends. Smoking and Tobacco Control Monograph No. 9. National Cancer Institute. pp. 1–20.
- ↑ Symm B, Morgan MV, Blackshear Y, Tinsley S (Jul 2005). "Cigar smoking: an ignored public health threat". The Journal of Primary Prevention. 26 (4): 363–375. PMID 15995804. doi:10.1007/s10935-005-5389-z.
- 1 2 National Institutes of Health (1998-04-10). "Background on Cigar Monograph: Cigars: Health Effects and Trends". Retrieved 2008-01-04.
- 1 2 Narkiewicz K, Kjeldsen SE, Hedner T (2005). "Is smoking a causative factor of hypertension?". Blood Pressure. 14 (2): 69–71. PMID 16036482. doi:10.1080/08037050510034202.
- ↑ Yacoub R, Habib H, Lahdo A, Al Ali R, Varjabedian L, Atalla G, Kassis Akl N, Aldakheel S, Alahdab S, Albitar S (2010). "Association between smoking and chronic kidney disease: a case control study". BMC Public Health. 10: 731. PMC 3004836
 . PMID 21108832. doi:10.1186/1471-2458-10-731.
. PMID 21108832. doi:10.1186/1471-2458-10-731. - ↑ Sawicki PT, Didjurgeit U, Mühlhauser I, Bender R, Heinemann L, Berger M (Feb 1994). "Smoking is associated with progression of diabetic nephropathy". Diabetes Care. 17 (2): 126–31. PMID 8137682. doi:10.2337/diacare.17.2.126.
- 1 2 Kark JD, Lebiush M, Rannon L (Oct 1982). "Cigarette smoking as a risk factor for epidemic a(h1n1) influenza in young men". The New England Journal of Medicine. 307 (17): 1042–6. PMID 7121513. doi:10.1056/NEJM198210213071702.
- 1 2 Finklea JF, Sandifer SH, Smith DD (Nov 1969). "Cigarette smoking and epidemic influenza". American Journal of Epidemiology. 90 (5): 390–9. PMID 5356947.
- ↑ Kark JD, Lebiush M (May 1981). "Smoking and epidemic influenza-like illness in female military recruits: a brief survey". American Journal of Public Health. 71 (5): 530–2. PMC 1619723
 . PMID 7212144. doi:10.2105/AJPH.71.5.530.
. PMID 7212144. doi:10.2105/AJPH.71.5.530. - ↑ Nicholson KG, Kent J, Hammersley V (Aug 1999). "Influenza A among community-dwelling elderly persons in Leicestershire during winter 1993-4; cigarette smoking as a risk factor and the efficacy of influenza vaccination". Epidemiology and Infection. 123 (1): 103–8. PMC 2810733
 . PMID 10487646. doi:10.1017/S095026889900271X.
. PMID 10487646. doi:10.1017/S095026889900271X. - ↑ American Cancer Society. "Questions About Smoking, Tobacco, and Health". Retrieved 2008-01-04.
- ↑ Henley SJ, Thun MJ, Chao A, Calle EE (Jun 2004). "Association between exclusive pipe smoking and mortality from cancer and other diseases". Journal of the National Cancer Institute. 96 (11): 853–861. PMID 15173269. doi:10.1093/jnci/djh144.
- ↑ Loren Stein. "Pipe Smoking". A Healthy Me!. Retrieved 2008-01-04.
- ↑ Commission on Life Sciences. "Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects (1986)". Retrieved 2008-01-04.
- ↑ Johnson GK, Slach NA (Apr 2001). "Impact of tobacco use on periodontal status". Journal of Dental Education. 65 (4): 313–21. PMID 11336116.
- ↑ Reibel J (2003). "Tobacco and oral diseases. Update on the evidence, with recommendations". Medical Principles and Practice. 12 Suppl 1: 22–32. PMID 12707498. doi:10.1159/000069845.
- ↑ Ness L, Rosekrans Dde L, Welford JF (Jan 1977). "An epidemiologic study of factors affecting extrinsic staining of teeth in an English population". Community Dentistry and Oral Epidemiology. 5 (1): 55–60. PMID 264419. doi:10.1111/j.1600-0528.1977.tb01617.x.
- ↑ "Helping you to Stop Smoking!". Retrieved 2008-01-04.
- ↑ Züllich G, Damm KH, Braun W, Lisboa BP (May 1975). "Studies on biliary excreted metabolites of [G-3H]digitoxin in rats". Archives Internationales de Pharmacodynamie et de Thérapie. 215 (1): 160–7. PMID 1156044.
- ↑ Dietrich T, Maserejian NN, Joshipura KJ, Krall EA, Garcia RI (Apr 2007). "Tobacco use and incidence of tooth loss among US male health professionals". Journal of Dental Research. 86 (4): 373–377. PMC 2582143
 . PMID 17384035. doi:10.1177/154405910708600414.
. PMID 17384035. doi:10.1177/154405910708600414. - ↑ Al-Bayaty FH, Wahid NA, Bulgiba AM (Feb 2008). "Tooth mortality in smokers and nonsmokers in a selected population in Sana'a, Yemen". Journal of Periodontal Research. 43 (1): 9–13. PMID 18230101. doi:10.1111/j.1600-0765.2007.00988.x.
- ↑ "Leukoplakia Causes". Mayo Clinic. Retrieved 31 May 2015.
- ↑ Davies PD, Yew WW, Ganguly D, Davidow AL, Reichman LB, Dheda K, Rook GA (Apr 2006). "Smoking and tuberculosis: the epidemiological association and immunopathogenesis". Transactions of the Royal Society of Tropical Medicine and Hygiene. 100 (4): 291–298. PMID 16325875. doi:10.1016/j.trstmh.2005.06.034.
- ↑ Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, Kumar R, Sinha DN, Dikshit RP, Parida DK, Kamadod R, Boreham J, Peto R (Mar 2008). "A nationally representative case-control study of smoking and death in India". The New England Journal of Medicine. 358 (11): 1137–1147. PMID 18272886. doi:10.1056/NEJMsa0707719.
- ↑ Nuorti JP, Butler JC, Farley MM, Harrison LH, McGeer A, Kolczak MS, Breiman RF (Mar 2000). "Cigarette smoking and invasive pneumococcal disease. Active Bacterial Core Surveillance Team". The New England Journal of Medicine. 342 (10): 681–9. PMID 10706897. doi:10.1056/NEJM200003093421002.
- ↑ Arcavi L, Benowitz NL (Nov 2004). "Cigarette smoking and infection". Archives of Internal Medicine. 164 (20): 2206–16. PMID 15534156. doi:10.1001/archinte.164.20.2206.
- ↑ Goedert JJ, Vitale F, Lauria C, Serraino D, Tamburini M, Montella M, Messina A, Brown EE, Rezza G, Gafà L, Romano N (Nov 2002). "Risk factors for classical Kaposi's sarcoma". Journal of the National Cancer Institute. 94 (22): 1712–8. PMID 12441327. doi:10.1093/jnci/94.22.1712.
- ↑ "MEDLINEplus: Smoking Cuts Risk of Rare Cancer". Retrieved 8 September 2014.
- 1 2 "The Tobacco Reference Guide". Retrieved 2006-07-15.
- ↑ Kendirci M, Nowfar S, Hellstrom WJ (Jan 2005). "The impact of vascular risk factors on erectile function". Drugs of Today. 41 (1): 65–74. PMID 15753970. doi:10.1358/dot.2005.41.1.875779.
- ↑ Dechanet C, Anahory T, Mathieu Daude JC, Quantin X, Reyftmann L, Hamamah S, Hedon B, Dechaud H (2011). "Effects of cigarette smoking on reproduction". Human Reproduction Update. 17 (1): 76–95. PMID 20685716. doi:10.1093/humupd/dmq033.
- ↑ FERTILITY FACT > Female Risks By the American Society for Reproductive Medicine (ASRM). Retrieved on Jan 4, 2009
- ↑ "protectyourfertility.com" (PDF). Retrieved 8 September 2014.
- 1 2 fertility services: a commissioning aid - June 2009, from the Department of Health UK
- ↑ Parrott AC (Oct 1999). "Does cigarette smoking cause stress?". The American Psychologist. 54 (10): 817–820. PMID 10540594. doi:10.1037/0003-066X.54.10.817.
- ↑ Lagrue G, Lebargy F, Cormier A (2001). "Des récepteurs nicotiniques à la dépendance tabagique : perspectives thérapeutiques" [From nicotinic receptors to smoking dependence: Therapeutic prospects]. Alcoologie et Addictologie (in French). 23 (2 Suppl): 39S–42S.
- 1 2 Parrott AC (Jan 1998). "Nesbitt's Paradox resolved? Stress and arousal modulation during cigarette smoking". Addiction. 93 (1): 27–39. PMID 9624709. doi:10.1046/j.1360-0443.1998.931274.x.
- ↑ Hughes JR (Oct 1992). "Tobacco withdrawal in self-quitters". Journal of Consulting and Clinical Psychology. 60 (5): 689–97. PMID 1401384. doi:10.1037/0022-006X.60.5.689.
- ↑ Cohen S, Lichtenstein E (1990). "Perceived stress, quitting smoking, and smoking relapse". Health Psychology. 9 (4): 466–78. PMID 2373070. doi:10.1037/0278-6133.9.4.466.
- ↑ Hamer M, Stamatakis E, Batty GD (Aug 2010). "Objectively assessed secondhand smoke exposure and mental health in adults: cross-sectional and prospective evidence from the Scottish Health Survey". Archives of General Psychiatry. 67 (8): 850–5. PMID 20529994. doi:10.1001/archgenpsychiatry.2010.76.
- ↑ Bachman JG, Wadsworth KN, O'Malley PM, Johnston LD, Schulenberg JE (1997). Smoking, drinking, and drug use in young adulthood: the impacts of new freedoms and new responsibilities. Hillsdale, N.J: L. Erlbaum Associates. p. 70. ISBN 0-8058-2547-9.
- ↑ Doherty EW, Doherty WJ (1998). "Smoke gets in your eyes: Cigarette smoking and divorce in a national sample of American adults". Families, Systems, & Health. 16 (4): 393–400. doi:10.1037/h0089864.
- 1 2 Almeida OP, Hulse GK, Lawrence D, Flicker L (Jan 2002). "Smoking as a risk factor for Alzheimer's disease: contrasting evidence from a systematic review of case-control and cohort studies". Addiction. 97 (1): 15–28. PMID 11895267. doi:10.1046/j.1360-0443.2002.00016.x.
- ↑ Anstey KJ, von Sanden C, Salim A, O'Kearney R (Aug 2007). "Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies". American Journal of Epidemiology. 166 (4): 367–378. PMID 17573335. doi:10.1093/aje/kwm116.
- ↑ Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR (Jan 2005). "Effects of smoking and smoking abstinence on cognition in adolescent tobacco smokers". Biological Psychiatry. 57 (1): 56–66. PMID 15607301. doi:10.1016/j.biopsych.2004.10.022.
- ↑ Brody AL, Mandelkern MA, Jarvik ME, Lee GS, Smith EC, Huang JC, Bota RG, Bartzokis G, London ED (Jan 2004). "Differences between smokers and nonsmokers in regional gray matter volumes and densities". Biological Psychiatry. 55 (1): 77–84. PMID 14706428. doi:10.1016/S0006-3223(03)00610-3.
- ↑ Akiyama H, Meyer JS, Mortel KF, Terayama Y, Thornby JI, Konno S (Nov 1997). "Normal human aging: factors contributing to cerebral atrophy". Journal of the Neurological Sciences. 152 (1): 39–49. PMID 9395125. doi:10.1016/S0022-510X(97)00141-X.
- ↑ Cataldo, JK; Prochaska, JJ; Glantz, SA (2010). "Cigarette smoking is a risk factor for Alzheimer's Disease: an analysis controlling for tobacco industry affiliation.". Journal of Alzheimer's disease : JAD. 19 (2): 465–80. PMC 2906761
 . PMID 20110594. doi:10.3233/JAD-2010-1240.
. PMID 20110594. doi:10.3233/JAD-2010-1240. - ↑ Fratiglioni L, Wang HX (Aug 2000). "Smoking and Parkinson's and Alzheimer's disease: review of the epidemiological studies". Behavioural Brain Research. 113 (1–2): 117–20. PMID 10942038. doi:10.1016/S0166-4328(00)00206-0.
- ↑ Cataldo J, Prochaska J, Glantz S (Jul 2010). "Cigarette smoking is a risk factor for Alzheimer’s disease: An analysis controlling for tobacco industry affiliation". Journal of Alzheimer's Disease. 19 (2): 465–480. PMC 2906761
 . PMID 20110594. doi:10.3233/JAD-2010-1240.
. PMID 20110594. doi:10.3233/JAD-2010-1240. - ↑ Allam MF, Campbell MJ, Hofman A, Del Castillo AS, Fernández-Crehuet Navajas R (Jun 2004). "Smoking and Parkinson's disease: systematic review of prospective studies". Movement Disorders. 19 (6): 614–621. PMID 15197698. doi:10.1002/mds.20029.
- ↑ Allam MF, Campbell MJ, Del Castillo AS, Fernández-Crehuet Navajas R (2004). "Parkinson's disease protects against smoking?". Behavioural Neurology. 15 (3–4): 65–71. PMID 15706049. doi:10.1155/2004/516302.
- ↑ Quik M (Sep 2004). "Smoking, nicotine and Parkinson's disease". Trends in Neurosciences. 27 (9): 561–568. PMID 15331239. doi:10.1016/j.tins.2004.06.008.
- ↑ Stough C, Mangan G, Bates T, Pellett O (Nov 1994). "Smoking and Raven IQ". Psychopharmacology. 116 (3): 382–4. PMID 7892431. doi:10.1007/BF02245346.
- ↑ Jarvis MJ (Jan 2004). "Why people smoke". BMJ. 328 (7434): 277–279. PMC 324461
 . PMID 14751901. doi:10.1136/bmj.328.7434.277.
. PMID 14751901. doi:10.1136/bmj.328.7434.277. - ↑ Hughes JR (Apr 2006). "Clinical significance of tobacco withdrawal". Nicotine & Tobacco Research. 8 (2): 153–156. PMID 16766409. doi:10.1080/14622200500494856.
- ↑ McNeill A (2001). "Smoking and mental health – a review of the literature" (PDF). SmokeFree London Programme. Retrieved 2008-10-05.
- ↑ Meltzer H, Gill B, Petticrew M, Hinds K (1995). OPCS Surveys of Psychiatric Morbidity Report 3: Economic Activity and Social Functioning of Adults With Psychiatric Disorders. London, Her Majesty’s Stationery Office.
- ↑ Kelly C, McCreadie RG (Nov 1999). "Smoking habits, current symptoms, and premorbid characteristics of schizophrenic patients in Nithsdale, Scotland". The American Journal of Psychiatry. 156 (11): 1751–7. PMID 10553739.
- ↑ Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA (Aug 1986). "Prevalence of smoking among psychiatric outpatients". The American Journal of Psychiatry. 143 (8): 993–7. PMID 3487983.
- ↑ Schroeder SA (Sep 2007). "Shattuck Lecture. We can do better--improving the health of the American people". The New England Journal of Medicine. 357 (12): 1221–1228. PMID 17881753. doi:10.1056/NEJMsa073350.
- ↑ George T (2002-07-22). "Schizophrenia and Smoking". Health Report. ABC Radio National (Australian Broadcasting Corporation). Retrieved 2012-05-06.
- ↑ Sacco KA, Bannon KL, George TP (Dec 2004). "Nicotinic receptor mechanisms and cognition in normal states and neuropsychiatric disorders". Journal of Psychopharmacology. 18 (4): 457–74. PMC 1201375
 . PMID 15582913. doi:10.1177/0269881104047273.
. PMID 15582913. doi:10.1177/0269881104047273. - ↑ Kumari V, Postma P (2005). "Nicotine use in schizophrenia: the self medication hypotheses". Neuroscience and Biobehavioral Reviews. 29 (6): 1021–34. PMID 15964073. doi:10.1016/j.neubiorev.2005.02.006.
- ↑ Gurillo, Pedro; Jauhar, Sameer; Murray, Robin M; MacCabe, James H (July 2015). "Does tobacco use cause psychosis? Systematic review and meta-analysis". The Lancet Psychiatry. 2: 718–725. doi:10.1016/S2215-0366(15)00152-2.
- ↑ Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL (Sep 1990). "Depression and the dynamics of smoking. A national perspective". JAMA. 264 (12): 1541–5. PMID 2395193. doi:10.1001/jama.1990.03450120053028.
- ↑ Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, Johnson J (Sep 1990). "Smoking, smoking cessation, and major depression". JAMA. 264 (12): 1546–9. PMID 2395194. doi:10.1001/jama.1990.03450120058029.
- ↑ Covey LS, Glassman AH, Stetner F (1998). "Cigarette smoking and major depression". Journal of Addictive Diseases. 17 (1): 35–46. PMID 9549601. doi:10.1300/J069v17n01_04.
- ↑ Hall SM, Muñoz RF, Reus VI, Sees KL (Oct 1993). "Nicotine, negative affect, and depression". Journal of Consulting and Clinical Psychology. 61 (5): 761–767. PMID 7902368. doi:10.1037/0022-006X.61.5.761.
- ↑ Wang, M; Wang, ZP; Gong, R; Zhao, ZT (January 2014). "Maternal smoking during pregnancy and neural tube defects in offspring: a meta-analysis.". Child's Nervous System. 30 (1): 83–9. PMID 23760473. doi:10.1007/s00381-013-2194-5.
- ↑ Ward C, Lewis S, Coleman T (2007). "Prevalence of maternal smoking and environmental tobacco smoke exposure during pregnancy and impact on birth weight: retrospective study using Millennium Cohort". BMC Public Health. 7: 81. PMC 1884144
 . PMID 17506887. doi:10.1186/1471-2458-7-81.
. PMID 17506887. doi:10.1186/1471-2458-7-81. - ↑ Maytin EV, Levin EN, Anderson RR (May 1991). "A laser densitometer for selective spot analysis on dot blots and two-dimensional gel autoradiograms". Analytical Biochemistry. 194 (2): 284–94. PMID 1862932. doi:10.1016/0003-2697(91)90231-H.
- ↑ Hartmann T (1997). Attention Deficit Disorder : A Different Perception. Underwood Books. ISBN 1-887424-14-8.
- ↑ Kroon LA (2007). "Drug interactions with smoking". Am J Health Syst Pharm. 64 (18): 1917–1921. PMID 17823102. doi:10.2146/ajhp060414.
- ↑ Ande A, McArthur C, Ayuk L, et al. (2015). "Effect of mild-to-moderate smoking on viral load, cytokines, oxidative stress, and cytochrome P450 enzymes in HIV-infected individuals.". PLOS ONE. 10: e0122402. PMC 4399877
 . PMID 25879453. doi:10.1371/journal.pone.0122402.
. PMID 25879453. doi:10.1371/journal.pone.0122402. - ↑ Chen H, Vlahos R, Bozinovski S, Jones J, Anderson GP, Morris MJ (Apr 2005). "Effect of short-term cigarette smoke exposure on body weight, appetite and brain neuropeptide Y in mice". Neuropsychopharmacology. 30 (4): 713–9. PMID 15508020. doi:10.1038/sj.npp.1300597. Lay summary – News-Medical.Net.
- ↑ Vanni H, Kazeros A, Wang R, Harvey BG, Ferris B, De BP, Carolan BJ, Hübner RH, O'Connor TP, Crystal RG (May 2009). "Cigarette smoking induces overexpression of a fat-depleting gene AZGP1 in the human". Chest. 135 (5): 1197–1208. PMC 2679098
 . PMID 19188554. doi:10.1378/chest.08-1024.
. PMID 19188554. doi:10.1378/chest.08-1024. - ↑ Leistikow BN, Martin DC, Milano CE (Aug 2000). "Fire injuries, disasters, and costs from cigarettes and cigarette lights: a global overview". Preventive Medicine. 31 (2 Pt 1): 91–9. PMID 10938207. doi:10.1006/pmed.2000.0680.
- ↑ Leistikow BN, Martin DC, Samuels SJ (Dec 2000). "Injury death excesses in smokers: a 1990-95 United States national cohort study". Injury Prevention. 6 (4): 277–80. PMC 1730660
 . PMID 11144627. doi:10.1136/ip.6.4.277.
. PMID 11144627. doi:10.1136/ip.6.4.277. - ↑ Cosnes J, Carbonnel F, Carrat F, Beaugerie L, Cattan S, Gendre J (Nov 1999). "Effects of current and former cigarette smoking on the clinical course of Crohn's disease". Alimentary Pharmacology & Therapeutics. 13 (11): 1403–11. PMID 10571595. doi:10.1046/j.1365-2036.1999.00630.x.
- ↑ Calkins BM (Dec 1989). "A meta-analysis of the role of smoking in inflammatory bowel disease". Digestive Diseases and Sciences. 34 (12): 1841–54. PMID 2598752. doi:10.1007/BF01536701.
- ↑ Lakatos PL, Szamosi T, Lakatos L (Dec 2007). "Smoking in inflammatory bowel diseases: good, bad or ugly?". World Journal of Gastroenterology. 13 (46): 6134–9. PMC 4171221
 . PMID 18069751. doi:10.3748/wjg.13.6134.
. PMID 18069751. doi:10.3748/wjg.13.6134. - ↑ Mahid SS, Minor KS, Soto RE, Hornung CA, Galandiuk S (Nov 2006). "Smoking and inflammatory bowel disease: a meta-analysis". Mayo Clinic Proceedings. 81 (11): 1462–1471. PMID 17120402. doi:10.4065/81.11.1462.
- ↑ Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ (Oct 2004). "Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors". American Journal of Epidemiology. 160 (8): 784–796. PMID 15466501. doi:10.1093/aje/kwh275.
- ↑ Calhaz-Jorge C, Mol BW, Nunes J, Costa AP (Sep 2004). "Clinical predictive factors for endometriosis in a Portuguese infertile population". Human Reproduction. 19 (9): 2126–2131. PMID 15229202. doi:10.1093/humrep/deh374.
- ↑ Baron JA (Jan 1996). "Beneficial effects of nicotine and cigarette smoking: the real, the possible and the spurious". British Medical Bulletin. 52 (1): 58–73. PMID 8746297. doi:10.1093/oxfordjournals.bmb.a011533.
- ↑ Schwartz SM, Marshall LM, Baird DD (Oct 2000). "Epidemiologic contributions to understanding the etiology of uterine leiomyomata". Environmental Health Perspectives. 108 Suppl 5: 821–7. JSTOR 3454313. PMID 11035989. doi:10.1289/ehp.00108s5821.
- ↑ Lubin JH, Steindorf K (Jan 1995). "Cigarette use and the estimation of lung cancer attributable to radon in the United States". Radiation Research. 141 (1): 79–85. PMID 7997518. doi:10.2307/3579093.
- ↑ Reid A, de Klerk NH, Ambrosini GL, Berry G, Musk AW (Aug 2006). "The risk of lung cancer with increasing time since ceasing exposure to asbestos and quitting smoking". Occupational and Environmental Medicine. 63 (8): 509–12. PMC 2078130
 . PMID 16849527. doi:10.1136/oem.2005.025379.
. PMID 16849527. doi:10.1136/oem.2005.025379. - ↑ Lederle FA, Larson JC, Margolis KL, Allison MA, Freiberg MS, Cochrane BB, Graettinger WF, Curb JD (2008). "Abdominal aortic aneurysm events in the women's health initiative: cohort study". BMJ. 337: a1724. PMC 2658825
 . PMID 18854591. doi:10.1136/bmj.a1724. Lay summary – Medical News Today.
. PMID 18854591. doi:10.1136/bmj.a1724. Lay summary – Medical News Today. - ↑ Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (Feb 2005). "Smoking and fracture risk: a meta-analysis". Osteoporosis International. 16 (2): 155–62. PMID 15175845. doi:10.1007/s00198-004-1640-3.
- ↑ Sørensen LT (Apr 2012). "Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis". Archives of Surgery. 147 (4): 373–83. PMID 22508785. doi:10.1001/archsurg.2012.5.
- ↑ Cohen DJ, Doucet M, Cutlip DE, Ho KK, Popma JJ, Kuntz RE (Aug 2001). "Impact of smoking on clinical and angiographic restenosis after percutaneous coronary intervention: another smoker's paradox?". Circulation. 104 (7): 773–8. PMID 11502701. doi:10.1161/hc3201.094225.
- ↑ Goldman SM (2014). "Environmental toxins and Parkinson's disease". Annu. Rev. Pharmacol. Toxicol. 54: 141–64. PMID 24050700. doi:10.1146/annurev-pharmtox-011613-135937.
- ↑ Pradhan P, Tirumala S, Liu X, Sayer JM, Jerina DM, Yeh HJ (May 2001). "Solution structure of a trans-opened (10S)-dA adduct of (+)-(7S,8R,9S,10R)-7,8-dihydroxy-9,10-epoxy-7,8,9,10-tetrahydrobenzo[a]pyrene in a fully complementary DNA duplex: evidence for a major syn conformation". Biochemistry. 40 (20): 5870–81. PMID 11352722. doi:10.1021/bi002896q.
- ↑ Bray F.; Tyczynski JE.; Parkin DM. (2004). "Going up or coming down? The changing phases of the lung cancer epidemic from 1967 to 1999 in the 15 European Union countries.". Eur. J. Cancer. 40: 96–125. PMID 14687795. doi:10.1016/j.ejca.2003.08.005.
- ↑ Jones M, Fosbery R, Taylor D (2000). "Answers to self-assessment questions". Biology 1. Cambridge Advanced Sciences. p. 250. ISBN 0-521-78719-X.
- 1 2 Feng Z, Hu W, Hu Y, Tang MS (Oct 2006). "Acrolein is a major cigarette-related lung cancer agent: Preferential binding at p53 mutational hotspots and inhibition of DNA repair". Proceedings of the National Academy of Sciences of the United States of America. 103 (42): 15404–15409. Bibcode:2006PNAS..10315404F. PMC 1592536
 . PMID 17030796. doi:10.1073/pnas.0607031103.
. PMID 17030796. doi:10.1073/pnas.0607031103. - ↑ Dr. C. Everett Koop. "Smoking and smokeless tobacco". Retrieved July 15, 2006.
- ↑ "Tobacco Smoke Carcinogens and Lung Cancer". Retrieved 8 September 2014.
- ↑ "DNA interaction with Benzopyrene". DNA. Archived from the original on December 23, 2004. Retrieved March 5, 2005.
- ↑ Kataoka H, Sumida A, Makita M (1997). "Determination of aliphatic and aromatic aldehydes in cigarette smoke by gas chromatography with flame photometric detection". Chromatographia. 44 (9–10): 491–6. doi:10.1007/BF02466742.
- ↑ Sumner PE, Moore JM, Boyette MD. "Retrofitting Tobacco Curing Barns" (PDF). Extension Engineering Publications. The University of Georgia College of Agricultural and Environmental Sciences. Retrieved 2012-05-06.
- ↑ NOVA. "Search for a Safer Cigarette".
- ↑ Godish T (2001). Indoor environmental quality. Chelsea, Michigan: Lewis Publishers. pp. 77–9. ISBN 1-56670-402-2.
- ↑ "Smoking, Health And Personality". REBEK. May 13, 2015.
- ↑ U.S. Army Center for Health Promotion and Preventive Medicine. "Radiological Sources of Potential Exposure and/or Contamination" (PDF). Archived from the original (PDF) on December 12, 2006.
- ↑ Martell EA (Mar 1983). "alpha-Radiation dose at bronchial bifurcations of smokers from indoor exposure to radon progeny". Proceedings of the National Academy of Sciences of the United States of America. 80 (5): 1285–9. Bibcode:1983PNAS...80.1285M. PMC 393580
 . PMID 6572389. doi:10.1073/pnas.80.5.1285.
. PMID 6572389. doi:10.1073/pnas.80.5.1285. - ↑ Muggli ME, Ebbert JO, Robertson C, Hurt RD (Sep 2008). "Waking a sleeping giant: the tobacco industry's response to the polonium-210 issue". American Journal of Public Health. 98 (9): 1643–50. PMC 2509609
 . PMID 18633078. doi:10.2105/AJPH.2007.130963.
. PMID 18633078. doi:10.2105/AJPH.2007.130963. - ↑ Rego B (Sep 2009). "The Polonium brief: a hidden history of cancer, radiation, and the tobacco industry" (PDF). Isis; An International Review Devoted to the History of Science and Its Cultural Influences. 100 (3): 453–484. PMID 19960838. doi:10.1086/644613.
- ↑ Office of Research Services, Division of Radiation Safety. "F. Typical Sources of Radiation Exposure". United States National Institutes of Health. Archived from the original on 2013-06-13. Retrieved 2012-05-06.
- ↑ "Radiation Risk for Xray and CT exams -". dosage chart. Associated Radiologists. Archived from the original on April 26, 2012. Retrieved 2012-05-06.
- ↑ "Radiation Risks and Realities" (PDF). United States Environmental Protection Agency.
- 1 2 "Everyday exposures to radiation". Front Line. Public Broadcasting System.
- ↑ "Radiation fears after Japan blast". BBC. 2011-07-21.
- ↑ Proctor RN (2006-12-01). "Puffing on Polonium". The New York Times.
- ↑ "Tobacco Smoke | Radiation Protection". United States Environmental Protection Agency. Retrieved 2012-05-06.
- ↑ Hecht SS (Jul 1999). "Tobacco smoke carcinogens and lung cancer". Journal of the National Cancer Institute. 91 (14): 1194–1210. PMID 10413421. doi:10.1093/jnci/91.14.1194.
- ↑ Hecht, S. S. (2011). "Tobacco smoke carcinogens and lung cancer". In Penning, T. M. Chemical Carcinogenesis. Totowa, NJ: Springer. p. 67. ISBN 9781617379949.
- ↑ Talhout R, Opperhuizen A, van Amsterdam JG (Oct 2007). "Role of acetaldehyde in tobacco smoke addiction". European Neuropsychopharmacology. 17 (10): 627–636. PMID 17382522. doi:10.1016/j.euroneuro.2007.02.013.
- ↑ Hilts PJ (1994-08-02). "Relative Addictiveness of Drugs". New York Times. Retrieved 2012-05-06.
- ↑ "The Henningfield-Benowitz substance comparison charts". Retrieved 2012-05-06.
- ↑ "AADAC|Truth About Tobacco – Addiction". Alberta Health Services.
- ↑ Gervais A, O'Loughlin J, Meshefedjian G, Bancej C, Tremblay M (Aug 2006). "Milestones in the natural course of onset of cigarette use among adolescents". Cmaj. 175 (3): 255–61. PMC 1513423
 . PMID 16880445. doi:10.1503/cmaj.051235.
. PMID 16880445. doi:10.1503/cmaj.051235. - ↑ National Cancer Institute. "Harms of Smoking and Health Benefits of Quitting". Fact Sheet. United States National Institutes of Health. Retrieved 2012-05-06.
- ↑ Smith D (2000). "Smoking increases teen depression". Monitor on Psychology. American Psychological Association. Retrieved 2012-05-06.
- ↑ National Institute on Drug Abuse. "Mind Over Matter: Tobacco Addiction". United States National Institutes of Health. Retrieved 2012-05-06.
- ↑ Parkin C, Fairweather DB, Shamsi Z, Stanley N, Hindmarch I (Mar 1998). "The effects of cigarette smoking on overnight performance". Psychopharmacology. 136 (2): 172–8. PMID 9551774. doi:10.1007/s002130050553.
- ↑ Maneckjee R, Minna JD (Oct 1994). "Opioids induce while nicotine suppresses apoptosis in human lung cancer cells". Cell Growth & Differentiation. 5 (10): 1033–1040. PMID 7848904.
- ↑ Guillem K, Vouillac C, Azar MR, Parsons LH, Koob GF, Cador M, Stinus L (Sep 2005). "Monoamine oxidase inhibition dramatically increases the motivation to self-administer nicotine in rats". The Journal of Neuroscience. 25 (38): 8593–8600. PMID 16177026. doi:10.1523/JNEUROSCI.2139-05.2005.
- ↑ Villégier AS, Blanc G, Glowinski J, Tassin JP (Sep 2003). "Transient behavioral sensitization to nicotine becomes long-lasting with monoamine oxidases inhibitors". Pharmacology, Biochemistry, and Behavior. 76 (2): 267–274. PMID 14592678. doi:10.1016/S0091-3057(03)00223-5.
- 1 2 "Secondhand Smoke". American Lung Association. June 2007. Retrieved 2012-05-06.
- ↑ ""Tobacco-Free Florida", Centers for Disease Control & Prevention Fact Sheets". Retrieved 8 September 2014.
- 1 2 IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2007). "Smokeless tobacco and some tobacco-specific N-nitrosamines" (PDF). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans / World Health Organization, International Agency for Research on Cancer. 89: 1–592. PMC 4781254
 . PMID 18335640.
. PMID 18335640. - ↑ "What is cancer?". Detailed Guide. American Cancer Society. 2011-04-11.
- 1 2 Symm B, Morgan MV, Blackshear Y, Tinsley S (Jul 2005). "Cigar smoking: an ignored public health threat". The Journal of Primary Prevention. 26 (4): 363–75. PMID 15995804. doi:10.1007/s10935-005-5389-z.
- ↑ Dollar KM, Mix JM, Kozlowski LT (May 2008). "Little cigars, big cigars: omissions and commissions of harm and harm reduction information on the Internet". Nicotine & Tobacco Research. 10 (5): 819–26. PMID 18569755. doi:10.1080/14622200802027214.
- ↑ Shanks TG, Burns DM (February 1988). "Disease Consequences of Cigar Smoking" (PDF). In Shopland DR, Burns DM, Hoffmann D, Cummings KM, Amacher RH. Cigars: Health Effects and Trends. Smoking and Tobacco Control Monograph No. 9. National Cancer Institute. pp. 105–60.
- ↑ "Questions and answers about cigar smoking and cancer". National Cancer Institute. 2000-03-07. Retrieved 2008-10-21.
- ↑ Misner, Jared (November 18, 2009). "UF study finds more teens smoke hookah". The Independent Florida Alligator.
- ↑ Knishkowy B, Amitai Y (Jul 2005). "Water-pipe (narghile) smoking: an emerging health risk behavior". Pediatrics. 116 (1): e113–9. PMID 15995011. doi:10.1542/peds.2004-2173.
- ↑ Hurt RD (2010-02-20). "Hookah smoking: Is it safer than cigarettes?". Mayo Clinic.
- ↑ "EGYPT: Water pipe smoking a significant TB risk". IRIN. March 24, 2008.
- ↑ Reuters (March 17, 2007). "Egyptians warned on pipe smoking". The Australian.
- 1 2 Shihadeh A, Azar S, Antonios C, Haddad A (Sep 2004). "Towards a topographical model of narghile water-pipe café smoking: a pilot study in a high socioeconomic status neighborhood of Beirut, Lebanon". Pharmacology, Biochemistry, and Behavior. 79 (1): 75–82. PMID 15388286. doi:10.1016/j.pbb.2004.06.005.
- ↑ Djordjevic MV, Stellman SD, Zang E (Jan 2000). "Doses of nicotine and lung carcinogens delivered to cigarette smokers". Journal of the National Cancer Institute. 92 (2): 106–11. PMID 10639511. doi:10.1093/jnci/92.2.106.
- ↑ Associated Press (May 29, 2007). "WHO warns the hookah may pose same risk as cigarettes". USA Today.
- ↑ Natto, SB (2005). "Tobacco smoking and periodontal health in a Saudi Arabian population.". Swedish dental journal. Supplement (176). PMID 16223098.
- ↑ Koch W (2005-12-28). "Hookah trend is puffing along". USA Today. Retrieved 2010-05-04.
- ↑ Sajid KM, Chaouachi K, Mahmood R (2008). "Hookah smoking and cancer: carcinoembryonic antigen (CEA) levels in exclusive/ever hookah smokers". Harm Reduction Journal. 5: 19. PMC 2438352
 . PMID 18501010. doi:10.1186/1477-7517-5-19.
. PMID 18501010. doi:10.1186/1477-7517-5-19. - ↑ Koul PA, Hajni MR, Sheikh MA, Khan UH, Shah A, Khan Y, Ahangar AG, Tasleem RA (2011). "Hookah smoking and lung cancer in the Kashmir valley of the Indian subcontinent". Asian Pacific Journal of Cancer Prevention. 12 (2): 519–24. PMID 21545223.
- ↑ Boffetta P, Hecht S, Gray N, Gupta P, Straif K (Jul 2008). "Smokeless tobacco and cancer". The Lancet. Oncology. 9 (7): 667–75. PMID 18598931. doi:10.1016/S1470-2045(08)70173-6.
- ↑ "Summaries for patients. Primary care interventions to prevent tobacco use in children and adolescents: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 159 (8): I–36. Oct 2013. PMID 23974179. doi:10.7326/0003-4819-159-8-201310150-00699.
- ↑ Guindon GE, Boisclair D (2003). Past, current and future trends in tobacco use (PDF). Washington DC: The International Bank for Reconstruction and Development / The World Bank. pp. 13–16. ISBN 1-932126-66-X. Retrieved 2009-03-22.
- 1 2 "WHO/WPRO-Smoking Statistics". World Health Organization Regional Office for the Western Pacific. 2002-05-28. Retrieved 2009-01-01.
- ↑ Centers for Disease Control and Prevention (CDC) (Nov 2007). "Cigarette smoking among adults--United States, 2006". MMWR. Morbidity and Mortality Weekly Report. 56 (44): 1157–61. PMID 17989644.
- 1 2 "The Global Burden of Disease 2004 Update" (PDF). World Health Organization. 2008. Retrieved 2008-01-01.
- 1 2 "WHO/WPRO-Tobacco Fact sheet". World Health Organization Regional Office for the Western Pacific. 2007-05-29. Retrieved 2009-01-01.
- ↑ Elementary and Secondary Education | Environmental Tobacco Smoke | Pro-Children Act of 2001 | Non-Smoking Policy for Children’s Services | Section 4303
- ↑ Colgrove J, Bayer R, Bachynski KE (Jun 2011). "Nowhere left to hide? The banishment of smoking from public spaces". The New England Journal of Medicine. 364 (25): 2375–7. PMID 21612464. doi:10.1056/NEJMp1104637.
- ↑ Lincecum, Gideon. "Nicotiana tabacum". Giden Lincecum Herbarium. University of Texas. Retrieved 9 December 2012.
- ↑ Adler IA (1980). "Classics in oncology. Primary malignant growths of the lung. Isaac A. Adler, A.M., M.D". CA: A Cancer Journal for Clinicians. 30 (5): 295–301. PMID 6773624. doi:10.3322/canjclin.30.5.295.
- ↑ Irving Fisher (1924). "Does tobacco injure the human body?". Readers Digest.
- 1 2 Proctor RN (Feb 2001). "Commentary: Schairer and Schöniger's forgotten tobacco epidemiology and the Nazi quest for racial purity". International Journal of Epidemiology. 30 (1): 31–4. PMID 11171846. doi:10.1093/ije/30.1.31.
- ↑ Adler I (1912). Primary malignant growths of the lungs and bronchi: a pathological and clinical study. New York: Longmans, Green. OCLC 14783544., cited in Spiro SG, Silvestri GA (Sep 2005). "One hundred years of lung cancer". American Journal of Respiratory and Critical Care Medicine. 172 (5): 523–9. PMID 15961694. doi:10.1164/rccm.200504-531OE.
- 1 2 3 Oreskes N Conway EM (2010). Merchants of Doubt: How a Handful of Scientists Obscured the Truth on Issues from Tobacco Smoke to Global Warming. San Francisco, CA: Bloomsbury Press. p. 15. ISBN 1-59691-610-9.
- 1 2 Michaels, David (2008). Doubt is their product: how industry's assault on science threatens your health. Oxford [Oxfordshire]: Oxford University Press. pp. 4–5. ISBN 0-19-530067-X.
- 1 2 Brandt AM (2007). The cigarette century: the rise, fall and deadly persistence of the product that defined America. New York: Basic Books, a member of the Perseus Books Group. ISBN 0-465-07047-7.
- 1 2 Bjerregaard BK, Raaschou-Nielsen O, Sørensen M, Frederiksen K, Tjønneland A, Rohrmann S, Linseisen J, Bergman MM, Boeing H, Sieri S, Palli D, Tumino R, Sacerdote C, Bueno-de-Mesquita HB, Büchner FL, Gram IT, Braaten T, Lund E, Hallmans G, Agren A, Riboli E (Dec 2006). "The effect of occasional smoking on smoking-related cancers: in the European Prospective Investigation into Cancer and Nutrition (EPIC)". Cancer Causes & Control. 17 (10): 1305–9. PMID 17111263. doi:10.1007/s10552-006-0068-9.
- ↑ Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, McConnachie A, Pringle S, Murdoch D, Dunn F, Oldroyd K, Macintyre P, O'Rourke B, Borland W (Jul 2008). "Smoke-free legislation and hospitalizations for acute coronary syndrome". The New England Journal of Medicine. 359 (5): 482–491. PMID 18669427. doi:10.1056/NEJMsa0706740.
- ↑ Winickoff JP, Friebely J, Tanski SE, Sherrod C, Matt GE, Hovell MF, McMillen RC (Jan 2009). "Beliefs about the health effects of "thirdhand" smoke and home smoking bans". Pediatrics. 123 (1): e74–e79. PMC 3784302
 . PMID 19117850. doi:10.1542/peds.2008-2184.
. PMID 19117850. doi:10.1542/peds.2008-2184.
Bibliography
- "WHO REPORT on the global TOBACCO epidemic" (PDF). World Health Organization. 2008. Retrieved 2008-01-01.
- "The Global Burden of Disease 2004 Update" (PDF). World Health Organization. 2008. Retrieved 2008-01-01.
- "Chapter 1: Introduction and Approach to Causal Inference" (PDF). 2004 Surgeon General's Report—The Health Consequences of Smoking (PDF). Washington DC: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2004. Retrieved 2009-05-24.
- "The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General" (PDF). Atlanta, U.S.: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2006. Retrieved 2009-02-15.
- "Cancer Facts and Figures 2004: Basic Cancer Facts". American Cancer Society. Retrieved 2009-01-21.
- Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, Pukkala E, Skytthe A, Hemminki K (Jul 2000). "Environmental and heritable factors in the causation of cancer--analyses of cohorts of twins from Sweden, Denmark, and Finland". The New England Journal of Medicine. 343 (2): 78–85. PMID 10891514. doi:10.1056/NEJM200007133430201.
- Montesano R, Hall J (Oct 2001). "Environmental causes of human cancers". European Journal of Cancer. 37 Suppl 8: S67–87. PMID 11602374. doi:10.1016/S0959-8049(01)00266-0.


