Flutamide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Eulexin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697045 |
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Nonsteroidal antiandrogen |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | >90% |
| Protein binding | 94 to 96% |
| Biological half-life | 8 hours (for 2-hydroxyflutamide)[1] |
| Excretion | >90% via urine |
| Identifiers | |
| |
| Synonyms | Niftolide; SCH-13521; 4'-nitro-3'-trifluoromethylisobutyranilide |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.033.024 |
| Chemical and physical data | |
| Formula | C11H11F3N2O3 |
| Molar mass | 276.212 g/mol |
| 3D model (JSmol) | |
| Melting point | 111.5 to 112.5 °C (232.7 to 234.5 °F) |
| |
| |
| (verify) | |
Flutamide, sold under the brand name Eulexin among others, is a nonsteroidal antiandrogen (NSAA) used primarily to treat prostate cancer.[2][3] It acts as a selective antagonist of the androgen receptor (AR), competing with androgens such as testosterone and its powerful active metabolite dihydrotestosterone (DHT) for binding to ARs in the prostate gland. By doing so, it prevents them from stimulating the prostate cancer cells to grow. In addition to its use in prostate cancer, flutamide has been used to treat hyperandrogenism (excess androgen levels) in women, such as in those with polycystic ovary syndrome (PCOS), and hirsutism.[4] Flutamide has been largely replaced by newer NSAAs, namely bicalutamide and enzalutamide, due particularly to better safety, tolerability, and pharmacokinetic profiles.[5][6]
Medical uses
Prostate cancer
GnRH is released by the hypothalamus in a pulsatile fashion; this causes the anterior pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH stimulates the testes to produce testosterone, which is metabolized to DHT by the enzyme 5α-reductase.
DHT, and to a significantly smaller extent, testosterone, stimulate prostate cancer cells to grow. Therefore, blocking these androgens can provide powerful treatment for prostate cancer, especially metastatic disease. Normally administered are GnRH analogues, such as leuprorelin or cetrorelix. Although GnRH agonists stimulate the same receptors that GnRH does, since they are present continuously and not in a pulsatile manner, they serve to inhibit the pituitary gland and therefore block the whole chain. However, they initially cause a surge in activity; this is not solely a theoretical risk but may cause the cancer to flare. Flutamide was initially used at the beginning of GnRH agonist therapy to block this surge, and it and other NSAAs continue in this use. In contrast to GnRH agonists, GnRH antagonists don't cause an initial androgen surge, and are gradually replacing GnRH agonists in clinical use.
There have been studies to investigate the benefit of adding an antiandrogen to surgical orchiectomy or its continued use with a GnRH analogue (combined androgen blockade (CAB)). Adding antiandrogens to orchiectomy showed no benefit, while a small benefit was shown with adding antiandrogens to GnRH analogues.
Unfortunately, therapies which lower testosterone levels, such as orchiectomy or GnRH analogue administration, also have significant side effects. Compared to these therapies, treatment with antiandrogens exhibits "fewer hot flashes, less of an effect on libido, less muscle wasting, fewer personality changes, and less bone loss." However, antiandrogen therapy alone is less effective than surgery. Nevertheless, given the advanced age of many with prostate cancer, as well as other features, many men may choose antiandrogen therapy alone for a better quality of life.[7]
Hyperandrogenism
Flutamide has been researched and used extensively in the treatment of hyperandrogenism (e.g., in polycystic ovary syndrome) in women and is highly effective in controlling symptoms including acne, seborrhea, hirsutism, and androgenetic alopecia. The dosages employed are lower than those used in the treatment of prostate cancer. Although flutamide continues to be used for this indication, its use in recent years has been limited due to the risk of potentially fatal hepatotoxicity, and it is not recommended as a first-line therapy.[8][9][10] The related NSAA bicalutamide has also been found to be highly effective in the treatment of hirsutism in women[11][12] and has a far lower and only small risk of hepatotoxicity in comparison.[13][14][15]
Transgender hormone therapy
Flutamide is used as a component of hormone replacement therapy for trans women.[16] However, its use for this purpose is discouraged due to reports, albeit rare, of hepatotoxicity in prostate cancer patients at comparable doses.[15][17]
Side effects
The side effects of flutamide are sex-dependent. In men, a variety of side effects related to androgen deprivation may occur, the most common being gynecomastia and breast tenderness[18] The vast majority (>90%) of cases of gynecomastia with NSAAs including flutamide are mild to moderate.[19][20][21] and others including hot flashes, decreased muscle mass, decreased bone mass and an associated increased risk of fractures, depression,[22] and sexual dysfunction including reduced libido and erectile dysfunction.[23] In women, flutamide is, generally, relatively well-tolerated, and does not interfere with ovulation.[24] The only common side effect reported with flutamide in women is dry skin (75%), which is attributable to diminished androgen-mediated sebum production.[25] General side effects that may occur in either sex include dizziness, anorexia, gastrointestinal side effects such as nausea, vomiting, and diarrhea, a greenish-bluish discoloration of the urine,[25] and hepatic changes.[22][23][26] Because flutamide is a pure antiandrogen, unlike steroidal antiandrogens like cyproterone acetate and megestrol acetate (which additionally possess progestogenic activity), it does not appear to have a risk of cardiovascular side effects (e.g., thromboembolism) or fluid retention.[21][22][27]
Tamoxifen, a selective estrogen receptor modulator (SERM) with predominantly antiestrogenic actions, can counteract flutamide-induced gynecomastia and breast pain in men.
Diarrhea
Diarrhea is more common and sometimes more severe with flutamide than with other NSAAs.[28] In a comparative trial of combined androgen blockade for prostate cancer, the rate of diarrhea was 26% for flutamide and 12% for bicalutamide.[28] Moreover, 6% of flutamide-treated patients discontinued the drug due to diarrhea, whereas only 0.5% of bicalutamide-treated patients did so.[28] In the case of antiandrogen monotherapy for prostate cancer, the rates of diarrhea are 5–20% for flutamide, 2–5% for bicalutamide, and 2–4% for nilutamide.[28] In contrast to diarrhea, the rates of nausea and vomiting are similar among the three drugs.[28]
Rare reactions
Hepatotoxicity
Although rare, flutamide has been associated with severe hepatotoxicity and death.[29][30][31] By 1996, 46 cases of severe cholestatic hepatitis had been reported, with 20 fatalities.[29] There have been continued case reports since, including liver transplants and death.[32][33] Based on the number of prescriptions written, the rate of serious hepatotoxicity associated with flutamide treatment is estimated to be 3 per 10,000.[29] However, other researchers have suggested that the incidence of significant hepatotoxicity may be as high as 6–9%.[32] Another source reported a rate of 0.36%.[34] Flutamide is also associated with liver enzyme elevations in 42–62% of patients.[35] The risk of hepatotoxicity with flutamide treatment is far higher than with nilutamide or bicalutamide.[13][14][15] Lower dosages of the drug appear to have a reduced but still significant risk.[32][36] Liver function should be monitored regularly with liver function tests during flutamide treatment.[37] In addition, due to the high risk of serious hepatotoxicity, flutamide should not be used in the absence of a serious indication.[34]
The mechanism of action of flutamide-induced hepatotoxicity is thought to be due to mitochondrial toxicity.[38][39][40] Specifically, flutamide and particularly its major metabolite 2-hydroxyflutamide inhibit enzymes in the mitochondrial electron transport chain in hepatocytes, including respiratory complexes I (NADH ubiquinone oxidoreductase), II (succinate dehydrogenase), and V (ATP synthase), and thereby reduce cellular respiration via ATP depletion and hence decrease cell survival.[38][39][40] Inhibition of taurocholate (a bile acid) efflux has also been implicated in flutamide-induced hepatotoxicity.[38][41] In contrast to flutamide and 2-hydroxyflutamide, which severely compromise hepatocyte cellular respiration in vitro, bicalutamide does not significantly do so at the same concentrations and is regarded as non-mitotoxic.[38][40] It is thought that the nitroaromatic group of flutamide and 2-hydroxyflutamide enhance their mitochondrial toxicity; bicalutamide, in contrast, possesses a cyano group in place of the nitro moiety, greatly reducing the potential for such toxicity.[39][42]
The combination of paracetamol (acetaminophen) and flutamide may result in additive to synergistic hepatotoxicity, indicating a potential drug interaction.[41]
Pulmonary toxicity
Flutamide has also been associated with interstitial pneumonitis (which can progress to pulmonary fibrosis).[30] The incidence of interstitial pneumonitis with flutamide was found to be 0.04% in a large clinical cohort of 41,700 prostate cancer patients.[43]
Photosensitivity
A variety of case reports have associated flutamide with photosensitivity.[30]
Comparison with other antiandrogens
Flutamide has been found to be similarly effective in the treatment of prostate cancer to bicalutamide, although indications of superior efficacy, including greater compensatory increases in testosterone levels and greater reductions in PSA levels, were observed with bicalutamide.[44][45] Flutamide, at a dosage of 750 mg/day (250 mg three times daily), has also been found to be equivalent in effectiveness to 250 mg/day oral cyproterone acetate as a monotherapy in the treatment of prostate cancer in a large-scale clinical trial of 310 patients, though its side effect and toxicity profile (including gynecomastia, diarrhea, nausea, loss of appetite, and liver disturbances) was regarded as considerably worse than that of cyproterone acetate.[22] In contrast to the case of men, flutamide has been found to be significantly more effective than cyproterone acetate (as well as another steroidal antiandrogen, spironolactone) in the treatment of androgen-dependent conditions such as acne and hirsutism in women.[10][25] This sex difference in effectiveness may be related to the fact that flutamide significantly increases androgen levels in men,[10] which counteracts its antiandrogen efficacy,[21] but does not increase androgen levels in women.[37] (In contrast to flutamide, cyproterone acetate, due to its progestogenic and antigonadotropic activity, does not increase and rather suppresses androgen levels in both sexes.)[10]
Pharmacology
Antiandrogen
Flutamide acts as a selective, competitive, silent antagonist of the androgen receptor (AR).[1] Its active metabolite, 2-hydroxyflutamide, has between 10- to 25-fold higher affinity for the AR than does flutamide, and hence is a more powerful antiandrogen in comparison.[1][21][46][47] However, at high concentrations, unlike flutamide, 2-hydroxyflutamide is able to weakly activate the AR.[1][48] Flutamide has far lower affinity for the AR than do steroidal antiandrogens like spironolactone and cyproterone acetate, and it is a relatively weak antiandrogen in terms of potency by weight, but the large dosages at which flutamide is used appear to compensate for this.[49] In accordance with its selectivity for the AR, flutamide possesses no progestogenic, (direct) estrogenic, glucocorticoid, or antigonadotropic activity.[25][50] Similarly to nilutamide, bicalutamide, and enzalutamide, flutamide crosses the blood-brain-barrier and exerts central antiandrogen actions.[51]
CYP17A1 inhibitor
Flutamide and 2-hydroxyflutamide have been found in vitro to inhibit CYP17A1 (17α-hydroxylase/17,20-lyase), an enzyme which is required for the biosynthesis of androgens.[52] In accordance, flutamide has been found to slightly but significantly lower androgen levels in GnRH analogue-treated male prostate cancer patients[53] and women with polycystic ovary syndrome.[25] As such, flutamide is a weak inhibitor of androgen biosynthesis.[49] However, the clinical significance of this action may be limited when flutamide is given without a GnRH analogue to non-castrated men, as the drug markedly elevates testosterone levels into the high normal male range via prevention of AR activation-mediated negative feedback on the hypothalamic-pituitary-gonadal axis in this context.[10]
Other actions
In addition to its antiandrogen activity, flutamide has been identified as a putative ligand of the aryl hydrocarbon receptor.[54]
Pharmacokinetics
Flutamide is metabolized by CYP1A2 (via α-hydroxylation) in the liver during first-pass metabolism[23] to its main active form, 2-hydroxyflutamide (which accounts for 23% of an oral dose of flutamide one hour post-ingestion),[25] and to at least five other minor metabolites.[55] Levels of 2-hydroxyflutamide are 50-fold higher than those of flutamide at steady-state.[56] Flutamide is excreted in various forms in the urine, the primary form being 2-amino-5-nitro-4-(trifluoromethyl)phenol.[57]
Flutamide has a fairly short half-life of 5–6 hours.[5][55] However, the half-life of its active form, 2-hydroxyflutamide, is somewhat longer at about 8–9 hours.[1][27][55] In any case, the half-lives of flutamide and 2-hydroxyflutamide are regarded as too short to allow for once-daily dosing, and the drug is instead administered three times daily at 8-hour intervals.[58] In contrast, the newer NSAAs nilutamide, bicalutamide, and enzalutamide all have much longer half-lives,[27] and this allows for once-daily administration in their cases.[59]
Steady-state levels of 2-hydroxyflutamide are achieved after 2–4 days of flutamide administration.[25]
Although 2-hydroxyflutamide has a half-life of 8–9 hours in elderly men, it has been reported to possess a shorter half-life in younger men.[27]
Chemistry
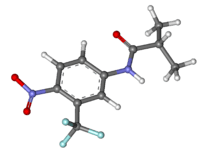
Unlike the hormones with which it competes, flutamide is not a steroid; rather, it is a substituted anilide. Hence, it is described as nonsteroidal in order to distinguish it from older steroidal antiandrogens such as cyproterone acetate and megestrol acetate.
Synthesis

History
Flutamide was first synthesized in 1967 by Neri and colleagues at Schering Plough Corporation.[3][63][27][64] It was originally synthesized as a bacteriostatic agent, but was subsequently, and serendipitously found to possess antiandrogen activity.[25][64] The code name of flutamide during development was SCH-13521.[65] Clinical research of the drug began in 1971,[66] and it was first marketed in 1983.[67][68] Flutamide was not introduced in the United States until 1989; it was specifically approved by the U.S. Food and Drug Administration for the treatment of metastatic prostate cancer in combination with a gonadotropin-releasing hormone (GnRH) analogue.[69] Flutamide was the first NSAA to be introduced, and was followed by nilutamide in 1989 and then bicalutamide in 1995.[70]
Society and culture
Generic name
Flutamide is the INN, USAN, BAN, DCF, and JAN of the drug.[71][2][3] Its names in Latin, German, and Spanish are flutamidum, flutamid, and flutamida, respectively.[71][2]
Brand names
Brand names of flutamide include or have included Cebatrol, Cytomid, Drogenil, Etaconil, Eulexin, Flucinom, Flumid, Flutacan, Flutamid, Flutamida, Flutamin, Flutan, Flutaplex, Flutasin, Fugerel, Profamid, and Sebatrol, among others.[71][2][3]
Availability
Flutamide is marketed widely throughout the world, including in the United States, Canada, Europe, Australia, New Zealand, South Africa, Central and South America, East and Southeast Asia, India, and the Middle East.[71][2]
Research
Benign prostatic hyperplasia
Flutamide has been studied in the treatment of benign prostatic hyperplasia in men in several clinical studies.[72][73] It has been found to reduce prostate volume by about 25%, which is comparable to the reduction achieved with the 5α-reductase inhibitor finasteride.[74] Unfortunately, it has been associated with side effects in these studies including gynecomastia and breast tenderness (in about 50% of patients), gastrointestinal disturbances such as nausea, diarrhea, and flatulence, and hepatotoxicity, although sexual function including libido and erectile potency were maintained.[74]
References
- 1 2 3 4 5 Thomas L. Lemke; David A. Williams (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1373–. ISBN 978-1-60913-345-0.
- 1 2 3 4 5 Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 466–. ISBN 978-3-88763-075-1.
- 1 2 3 4 J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 573–. ISBN 978-1-4757-2085-3.
- ↑ "Polycystic Ovary Syndrome - Treatment - NHS Choices". Nhs.uk. 2011-10-17. Retrieved 2013-01-04.
- 1 2 James Leonard Gulley (2011). Prostate Cancer. Demos Medical Publishing. pp. 81–. ISBN 978-1-935281-91-7.
- ↑ Lutz Moser (1 January 2008). Controversies in the Treatment of Prostate Cancer. Karger Medical and Scientific Publishers. pp. 41–42. ISBN 978-3-8055-8524-8.
- ↑ Scher, Howard I. (2005). "Hyperplastic and Malignant Diseases of the Prostate". In Dennis L. Kasper, Anthony S. Fauci, Dan L. Longo, Eugene Braunwald, Stephen L. Hauser, & J. Larry Jameson (Eds.), Harrison's Principles of Internal Medicine (16th edition), pp. 548–9. New York: McGraw-Hill.
- ↑ Adam Ostrzenski (2002). Gynecology: Integrating Conventional, Complementary, and Natural Alternative Therapy. Lippincott Williams & Wilkins. pp. 86–. ISBN 978-0-7817-2761-7.
- ↑ Ulrike Blume-Peytavi; David A. Whiting; Ralph M. Trüeb (26 June 2008). Hair Growth and Disorders. Springer Science & Business Media. pp. 181–. ISBN 978-3-540-46911-7.
- 1 2 3 4 5 Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1196, 1208. ISBN 978-0-7817-1750-2.
- ↑ Erem C (2013). "Update on idiopathic hirsutism: diagnosis and treatment". Acta Clinica Belgica. 68 (4): 268–74. PMID 24455796. doi:10.2143/ACB.3267.
- ↑ Müderris II, Bayram F, Ozçelik B, Güven M (Feb 2002). "New alternative treatment in hirsutism: bicalutamide 25 mg/day". Gynecological Endocrinology. 16 (1): 63–6. PMID 11915584. doi:10.1080/713602986.
- 1 2 Jordan VC, Furr BJ (5 February 2010). Hormone Therapy in Breast and Prostate Cancer. Springer Science & Business Media. pp. 350–. ISBN 978-1-59259-152-7.
- 1 2 Dansette P, Snyder RR, Monks TJ, Jollow DJ, Sipes IG, Greim H, Gibson GG, Delaforge M (6 December 2012). Biological Reactive Intermediates Vi: Chemical and Biological Mechanisms in Susceptibility to and Prevention of Environmental Diseases. Springer Science & Business Media. pp. 37–. ISBN 978-1-4615-0667-6.
- 1 2 3 Ramon J, Denis L (5 June 2007). Prostate Cancer. Springer Science & Business Media. pp. 256–. ISBN 978-3-540-40901-4.
- ↑ Baudewijntje P.C. Kreukels; Thomas D. Steensma; Annelou L.C. de Vries (1 July 2013). Gender Dysphoria and Disorders of Sex Development: Progress in Care and Knowledge. Springer Science & Business Media. pp. 280–. ISBN 978-1-4614-7441-8.
- ↑ Dahl, M., Feldman, J., Goldberg, J.M., Jaberi, A., Bockting, W.O., and Knudson, G. (2006). Endocrine therapy for transgender adults in British Columbia: Suggested guidelines. Vancouver, BC: Vancouver Health Authority.
- ↑ Farida, Chentli; Faiza, Belhimer (2013). "Severe gynecomastia due to anti androgens intake: A case report and literature review". Indian Journal of Endocrinology and Metabolism. 17 (4): 730. ISSN 2230-8210. doi:10.4103/2230-8210.113770.
- ↑ Gillatt, David (2006). "Antiandrogen treatments in locally advanced prostate cancer: are they all the same?". Journal of Cancer Research and Clinical Oncology. 132 (S1): 17–26. ISSN 0171-5216. PMID 16845534. doi:10.1007/s00432-006-0133-5.
Unlike CPA, non-steroidal antiandrogens appear to be better tolerated than castration, allowing patients to maintain sexual activity, physical ability, and bone mineral density, but these agents have a higher incidence of gynecomastia and breast pain (mild to moderate in > 90% of cases).
- ↑ Goldspiel BR, Kohler DR (1990). "Flutamide: An Antiandrogen for Advanced Prostate Cancer". Ann Pharmacother. 24 (6): 616–623. PMID 2193461. doi:10.1177/106002809002400612.
[...] They [in patients treated with flutamide] observed mild gynecomastia in 30 patients (57 percent), moderate gynecomastia in 19 (36 percent), and massive gynecomastia in 4 patients (8 percent). Complaints of nipple and areolar tenderness were noted in 50/53 patients (94 per- cent)." Airhart et al. reported that 42 percent of patients receiving flutamide 750 mg/d or 1500 mg/d developed gynecomastia within 12 weeks of starting treatment with an apparent direct correlation between the dose of flutamide administered and the severity of gynecomastia.25 In another study, two of five evaluable patients developed moderate gynecomastia with mild tenderness at four and eight weeks after starting flutamide 750 mg/d. Patients with preexisting gynecomastia as a result of previous endocrine therapy with estrogens sustained no worsening of their gynecomastia and may have improved symptomatically." Keating et al."
- 1 2 3 4 William B. Pratt (1994). The Anticancer Drugs. Oxford University Press. pp. 219–220. ISBN 978-0-19-506739-2.
- 1 2 3 4 Jack H. Mydlo; Ciril J. Godec (29 September 2015). Prostate Cancer: Science and Clinical Practice. Elsevier Science. pp. 516–521, 534–540. ISBN 978-0-12-800592-7.
- 1 2 3 Richard A. Lehne (2013). Pharmacology for Nursing Care. Elsevier Health Sciences. pp. 1297–. ISBN 1-4377-3582-7.
- ↑ Ricardo Azziz (8 November 2007). Androgen Excess Disorders in Women. Springer Science & Business Media. pp. 384–. ISBN 978-1-59745-179-6.
- 1 2 3 4 5 6 7 8 Bentham Science Publishers (September 1999). Current Pharmaceutical Design. Bentham Science Publishers. pp. 712–716.
Latest studies suggest that [flutamide] also reduces adrenal and ovarian androgen synthesis [58,59]. [...] No alteration in the hormone levels has been observed in patients treated with flutamide for 6 or 12 months [61,62]. However in other studies flutamide decreased circulating concentrations of DHEAS as well as androstenedione, total testosterone and 3a-androstanediol glucuronide, in young women with PCOS [41,59]. These effects may be due to inhibition of adrenal 17-20 lyase [17,63]. Although there was no effect on gonadotropin response to GnRH, basal levels of FSH showed a rise associated with a small fall of LH [64].
- ↑ Jay Roberts; David L. Snyder; Eitan Friedman (14 August 1996). Handbook of Pharmacology on Aging. CRC Press. pp. 334–. ISBN 978-0-8493-8306-9.
- 1 2 3 4 5 Louis J Denis; Keith Griffiths; Amir V Kaisary; Gerald P Murphy (1 March 1999). Textbook of Prostate Cancer: Pathology, Diagnosis and Treatment: Pathology, Diagnosis and Treatment. CRC Press. pp. 279–280. ISBN 978-1-85317-422-3.
- 1 2 3 4 5 JORDAN V. CRAIG; B.J.A. Furr (5 February 2010). Hormone Therapy in Breast and Prostate Cancer. Springer Science & Business Media. pp. 356–. ISBN 978-1-59259-152-7.
- 1 2 3 Neil Kaplowitz (16 October 2002). Drug-Induced Liver Disease. CRC Press. pp. 618–619. ISBN 978-0-203-90912-6.
- 1 2 3 Jeffrey K. Aronson (19 April 2010). Meyler's Side Effects of Drugs in Cancer and Immunology. Elsevier. pp. 318–319. ISBN 978-0-08-093288-0.
- ↑ Thole, Zebron; Manso, Gloria; Salgueiro, Esther; Revuelta, Pilar; Hidalgo, Agustin (2004). "Hepatotoxicity Induced by Antiandrogens: A Review of the Literature". Urologia Internationalis. 73 (4): 289–295. ISSN 0042-1138. PMID 15604569. doi:10.1159/000081585.
- 1 2 3 Brahm J, Brahm M, Segovia R, Latorre R, Zapata R, Poniachik J, Buckel E, Contreras L (2011). "Acute and fulminant hepatitis induced by flutamide: case series report and review of the literature". Ann Hepatol. 10 (1): 93–8. PMID 21301018.
- ↑ García Cortés M, Andrade RJ, Lucena MI, Sánchez Martínez H, Fernández MC, Ferrer T, Martín-Vivaldi R, Peláez G, Suárez F, Romero-Gómez M, Montero JL, Fraga E, Camargo R, Alcántara R, Pizarro MA, García-Ruiz E, Rosemary-Gómez M (2001). "Flutamide-induced hepatotoxicity: report of a case series". Rev Esp Enferm Dig. 93 (7): 423–32. PMID 11685939.
- 1 2 Jeffrey K. Aronson (21 February 2009). Meyler's Side Effects of Endocrine and Metabolic Drugs. Elsevier. pp. 153–. ISBN 978-0-08-093292-7.
- ↑ Jafri, Syed-Mohammed R. (2014). "Bicalutamide-induced hepatotoxicity: A rare adverse effect". American Journal of Case Reports. 15: 266–270. ISSN 1941-5923. PMC 4068966
 . PMID 24967002. doi:10.12659/AJCR.890679.
. PMID 24967002. doi:10.12659/AJCR.890679. - ↑ Bruni, Vincenzina; Peruzzi, Elena; Dei, Metella; Nannini, Sara; Seravalli, Viola; Sisti, Giovanni; Fambrini, Massimiliano (2012). "Hepatotoxicity with low- and ultralow-dose flutamide: a surveillance study on 203 hyperandrogenic young females". Fertility and Sterility. 98 (4): 1047–1052. ISSN 0015-0282. PMID 22795685. doi:10.1016/j.fertnstert.2012.06.018.
- 1 2 Evanthia Diamanti-Kandarakis; John E. Nestler; Dimitrios Panidis; Renato Pasquali (21 December 2009). Insulin Resistance and Polycystic Ovarian Syndrome: Pathogenesis, Evaluation, and Treatment. Springer Science & Business Media. pp. 75–. ISBN 978-1-59745-310-3.
- 1 2 3 4 Ball, Amy L.; Kamalian, Laleh; Alfirevic, Ana; Lyon, Jonathan J.; Chadwick, Amy E. (2016). "Identification of the Additional Mitochondrial Liabilities of 2-Hydroxyflutamide When Compared With its Parent Compound, Flutamide in HepG2 Cells". Toxicological Sciences: kfw126. ISSN 1096-6080. PMID 27413113. doi:10.1093/toxsci/kfw126.
- 1 2 3 Coe, Kevin J.; Jia, Yankai; Ho, Han Kiat; Rademacher, Peter; Bammler, Theo K.; Beyer, Richard P.; Farin, Frederico M.; Woodke, Libby; Plymate, Stephen R.; Fausto, Nelson; Nelson, Sidney D. (2007). "Comparison of the Cytotoxicity of the Nitroaromatic Drug Flutamide to Its Cyano Analogue in the Hepatocyte Cell Line TAMH: Evidence for Complex I Inhibition and Mitochondrial Dysfunction Using Toxicogenomic Screening". Chemical Research in Toxicology. 20 (9): 1277–1290. ISSN 0893-228X. PMC 2802183
 . PMID 17702527. doi:10.1021/tx7001349.
. PMID 17702527. doi:10.1021/tx7001349. - 1 2 3 Marroquin, L. D.; Hynes, J.; Dykens, J. A.; Jamieson, J. D.; Will, Y. (2007). "Circumventing the Crabtree Effect: Replacing Media Glucose with Galactose Increases Susceptibility of HepG2 Cells to Mitochondrial Toxicants". Toxicological Sciences. 97 (2): 539–547. ISSN 1096-6080. PMID 17361016. doi:10.1093/toxsci/kfm052.
- 1 2 Kostrubsky, Seva E.; Strom, Stephen C.; Ellis, Ewa; Nelson, Sidney D.; Mutlib, Abdul E. (2007). "Transport, Metabolism, and Hepatotoxicity of Flutamide, Drug–Drug Interaction with Acetaminophen Involving Phase I and Phase II Metabolites". Chemical Research in Toxicology. 20 (10): 1503–1512. ISSN 0893-228X. doi:10.1021/tx7001542.
- ↑ Boelsterli, Urs; Ho, Han; Zhou, Shufeng; Yeow Leow, Koon (2006). "Bioactivation and Hepatotoxicity of Nitroaromatic Drugs". Current Drug Metabolism. 7 (7): 715–727. ISSN 1389-2002. PMID 17073576. doi:10.2174/138920006778520606.
- ↑ Bennett CL, Raisch DW, Sartor O (2002). "Pneumonitis associated with nonsteroidal antiandrogens: presumptive evidence of a class effect". Ann. Intern. Med. 137 (7): 625. PMID 12353966. doi:10.7326/0003-4819-137-7-200210010-00029.
An estimated 0.77% of the 6,480 nilutamide-treated patients, 0.04% of the 41,700 flutamide-treated patients, and 0.01% of the 86,800 bicalutamide-treated patients developed pneumonitis during the study period.
- ↑ Helsen C, Van den Broeck T, Voet A, Prekovic S, Van Poppel H, Joniau S, Claessens F (Aug 2014). "Androgen receptor antagonists for prostate cancer therapy". Endocrine-Related Cancer. 21 (4): T105–18. PMID 24639562. doi:10.1530/ERC-13-0545.
- ↑ Nakai Y, Tanaka N, Anai S, Miyake M, Tatsumi Y, Fujimoto K (2015). "A Randomized Control Trial Comparing the Efficacy of Antiandrogen Monotherapy: Flutamide vs. Bicalutamide". Horm Cancer. 6 (4): 161–7. PMID 26024831. doi:10.1007/s12672-015-0226-1.
- ↑ William Figg; Cindy H. Chau; Eric J. Small (14 September 2010). Drug Management of Prostate Cancer. Springer Science & Business Media. pp. 71–. ISBN 978-1-60327-829-4.
- ↑ DICP: The Annals of Pharmacotherapy. Harvey Whitney Books Company. 1990. p. 617.
Additionally, 2-hydroxyflutamide has approximately a 25-fold greater affinity for androgen receptors than does flutamide.
- ↑ Masiello, D.; Cheng, S.; Bubley, G. J.; Lu, M. L.; Balk, S. P. (2002). "Bicalutamide Functions as an Androgen Receptor Antagonist by Assembly of a Transcriptionally Inactive Receptor". Journal of Biological Chemistry. 277 (29): 26321–26326. ISSN 0021-9258. PMID 12015321. doi:10.1074/jbc.M203310200.
- 1 2 Douglas T. Carrell; C. Matthew Peterson (23 March 2010). Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice. Springer Science & Business Media. pp. 163–. ISBN 978-1-4419-1436-1.
- ↑ J. Larry Jameson; Leslie J. De Groot (18 May 2010). Endocrinology: Adult and Pediatric. Elsevier Health Sciences. pp. 2401–. ISBN 1-4557-1126-8.
- ↑ Hormones - Antineoplastics: Advances in Research and Application: 2011 Edition: ScholarlyPaper. ScholarlyEditions. 9 January 2012. pp. 9–. ISBN 978-1-4649-4785-8.
- ↑ Ayub, M.; Levell, M.J. (1987). "Inhibition of rat testicular 17α-hydroxylase and 17,20-lyase activities by anti-androgens (flutamide, hydroxyflutamide, ru23908, cyproterone acetate) in vitro". Journal of Steroid Biochemistry. 28 (1): 43–47. ISSN 0022-4731. PMID 2956461. doi:10.1016/0022-4731(87)90122-1.
- ↑ Ayub, M.; Levell, M. J. (1990). "SUPPRESSION OF PLASMA ANDROGENS BY THE ANTIANDROGEN FLUTAMIDE IN PROSTATIC CANCER PATIENTS TREATED WITH ZOLADEX, A GnRH ANALOGUE". Clinical Endocrinology. 32 (3): 329–340. ISSN 0300-0664. doi:10.1111/j.1365-2265.1990.tb00874.x.
- ↑ Koch DC, Jang HS, O'Donnell EF, Punj S, Kopparapu PR, Bisson WH, Kerkvliet NI, Kolluri SK (2015). "Anti-androgen flutamide suppresses hepatocellular carcinoma cell proliferation via the aryl hydrocarbon receptor mediated induction of transforming growth factor-β1". Oncogene. 34 (50): 6092–104. PMID 25867062. doi:10.1038/onc.2015.55.
- 1 2 3 Bruce A. Chabner; Dan L. Longo (8 November 2010). Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. pp. 679–. ISBN 978-1-60547-431-1.
- ↑ Vincent DeVita; Theodore S. Lawrence; Steven A. Rosenberg (29 September 2015). Lymphomas and Leukemias: Cancer: Principles & Practice of Oncology. Wolters Kluwer Health. pp. 1029–. ISBN 978-1-4963-3828-0.
- ↑ Analytical Profiles of Drug Substances and Excipients. Academic Press. 19 March 2001. pp. 155–. ISBN 978-0-08-086122-7.
- ↑ W. Renée Acosta (1 October 2009). LWW's Foundations in Pharmacology for Pharmacy Technicians. Lippincott Williams & Wilkins. pp. 300–. ISBN 978-0-7817-6624-1.
- ↑ Alan J. Wein; Louis R. Kavoussi; Andrew C. Novick; Alan W. Partin; Craig A. Peters (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2939–. ISBN 978-1-4160-6911-9.
- ↑ Stabile, R. G.; Dicks, A. P. (2003). "Microscale Synthesis and Spectroscopic Analysis of Flutamide, an Antiandrogen Prostate Cancer Drug". Journal of Chemical Education. 80 (12): 1439. doi:10.1021/ed080p1439.
- ↑ Baker, J. W.; Bachman, G. L.; Schumacher, I.; Roman, D. P.; Tharp, A. L. (1967). "Synthesis and Bacteriostatic Activity of Some Nitrotrifluoro methylanilides". Journal of Medicinal Chemistry. 10 (1): 93–5. PMID 6031711. doi:10.1021/jm00313a020.
- ↑ Bandgar, B. P.; Sawant, S. S. (2006). "Novel and Gram‐Scale Green Synthesis of Flutamide". Synthetic Communications. 36 (7): 859–864. doi:10.1080/00397910500464848.
- ↑ H. John Smith; Hywel Williams (10 October 2005). Smith and Williams' Introduction to the Principles of Drug Design and Action, Fourth Edition. CRC Press. pp. 489–. ISBN 978-0-203-30415-0.
- 1 2 Baker JW, Bachman GL, Schumacher I, Roman DP, Tharp AL (1967). "Synthesis and bacteriostatic activity of some nitrotrifluoromethylanilides". J. Med. Chem. 10 (1): 93–5. PMID 6031711. doi:10.1021/jm00313a020.
- ↑ Barry Boettcher (12 May 2014). Immunological Influence on Human Fertility: Proceedings of the Workshop on Fertility in Human Reproduction, University of Newcastle, Australia, July 11-13, 1977. Elsevier Science. pp. 167–. ISBN 978-1-4832-6895-8.
- ↑ The Irish Reports: Containing Reports of Cases Argued and Determined in the Court of Appeal, the High Court of Justice, the Court of Bankruptcy, in Ireland, and the Irish Land Commission. Incorporated Council of Law Reporting for Ireland. 1990. p. 501.
- ↑ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 1695–. ISBN 978-0-8155-1856-3.
- ↑ The Irish Reports: Containing Reports of Cases Argued and Determined in the Court of Appeal, the High Court of Justice, the Court of Bankruptcy, in Ireland, and the Irish Land Commission. Incorporated Council of Law Reporting for Ireland. 1990. pp. 501–502.
- ↑ Vera Regitz-Zagrosek (2 October 2012). Sex and Gender Differences in Pharmacology. Springer Science & Business Media. pp. 575–. ISBN 978-3-642-30725-6.
- ↑ Jean-Pierre Bégué; Daniele Bonnet-Delpon (2 June 2008). Bioorganic and Medicinal Chemistry of Fluorine. John Wiley & Sons. pp. 327–. ISBN 978-0-470-28187-1.
- 1 2 3 4 https://www.drugs.com/international/flutamide.html
- ↑ Oesterling JE (1994). "Endocrine therapies for symptomatic benign prostatic hyperplasia". Urology. 43 (2 Suppl): 7–16. PMID 7509536.
- ↑ Stone NN (1989). "Flutamide in treatment of benign prostatic hypertrophy". Urology. 34 (4 Suppl): 64–8; discussion 87–96. PMID 2477936.
- 1 2 Lee M, Sharifi R (1997). "Benign prostatic hyperplasia: diagnosis and treatment guideline". Ann Pharmacother. 31 (4): 481–6. PMID 9101011.