Influenza research
| Influenza (Flu) |
|---|
 |
| Types |
| Vaccines |
| Treatment |
| Pandemics |
| Outbreaks |
| See also |
Influenza research involves investigating molecular virology, pathogenesis, host immune responses, genomics, and epidemiology regarding influenza. The main goal of research is to develop influenza countermeasures such as vaccines, therapies and diagnostic tools.
At least 12 companies and 17 governments are developing pre-pandemic influenza vaccines in 28 different clinical trials that, if successful, could turn a deadly pandemic infection into a nondeadly pandemic infection. A vaccine that could prevent any illness at all from the not-yet-existing pandemic influenza strain will take at least three months from the virus's emergence until full-scale vaccine production could begin; with vaccine production hoped to increase until one billion doses are produced by one year after the virus is first identified.[1]
Improved influenza countermeasures require basic research on how viruses enter cells, replicate, mutate, evolve into new strains and induce an immune response. Solutions to limitations in current vaccine methods are being researched.
The Influenza Genome Sequencing Project was initiated in 2004 to create a library of influenza sequences to understand what makes one strain more lethal than another, what genetic determinants most affect immunogenicity, and how the virus evolves over time.
Areas of current flu research
Avian flu
Before 2004, all previous highly pathogenic avian flu (HPAI) virus strains circulated only among domesticated poultry and by culling all of them in the area, the strains were made extinct. Previous HPAI strains only existed in domesticated birds. A wild bird's LPAI would mutate in a domestic flock into an HPAI strain, all domestic birds in the area would be killed, and the HPAI strain would no longer have any hosts and thus would no longer exist. This current HPAI H5N1 strain has turned out to be different. In October 2004 researchers discovered H5N1 is far more dangerous than previously believed because waterfowl, especially ducks, were directly spreading the highly pathogenic strain of H5N1. From this point on, avian flu experts increasingly referred to containment as a strategy that can delay but not prevent a future avian flu pandemic. Nonetheless, there is still hope it will mutate into some low pathogenic strain over time and no longer exist in its current high pathogenic set of strains. But as time has gone on, the hope has come to look less and less likely. The result is that billions of dollars every year are going to be needed in expenditures that would not be required if it did go away. Poultry farming is especially hard hit. How to best spend pandemic mitigation funds and poultry farming protection funds is a question that to be answered requires billions in flu research and new flu vaccine manufacturing factories.
Since avian flu is not going away as was hoped, more data is needed to figure out how best to cope. Governments are funding a variety of studies from cell culture of flu viruses to H5N1 vaccination effectiveness to adjuvants to wild bird migration patterns to wild bird avian flu subtype distribution to poultry flu vaccination etc. The information being gathered is increasing the world's ability to keep H5N1 contained, limiting its speed and extent of mutation, and buying time for new flu vaccine manufacturing methods and factories to come on line so that when the next flu pandemic happens the death toll can be minimized.
Universal flu vaccines
See Prospects for universal flu vaccines
Current major flu research contracts
The US government on May 4, 2006 awarded five-year contracts for "more than $1 billion to five drug manufacturers developing technology for speedier mass production of vaccines in the event of a pandemic" from the $3.8 billion pandemic preparedness bill passed in 2005. "The federal government says its goal is to be able to distribute a vaccine to every American within six months of a pandemic. Currently, flu vaccines are produced in specialized chicken eggs, but that technique does not allow for speedy mass vaccinations." The companies receiving the contracts were:
- GlaxoSmithKline $274.8 million
- MedImmune Inc $169.5 million
- Novartis Vaccines and Diagnostics $220.5 million
- DynPort Vaccine Company,LLC $41 million
- Solvay Pharmaceuticals $298.6 million[2]
The US government purchased from Sanofi Pasteur and Chiron Corporation several million doses of vaccine meant to be used in case of an influenza pandemic due to H5N1 and is conducting clinical trials on them.[3] ABC News reported on April 1, 2006 that "Beginning in late 1997, the human trials have tested 30 different vaccines, all pegged to the H5N1 virus."[4]
"To address the H9N2 threat, NIAID contracted with Chiron Corporation to produce investigational batches of an inactivated vaccine, which will be evaluated clinically by NIAID early next year. For H5N1, Aventis-Pasteur and Chiron are both producing investigational lots of inactivated H5N1 vaccine preparations; additionally, DHHS has contracted with Aventis to produce up to 2 million doses to be stockpiled for emergency use, if needed, to vaccinate health workers, researchers, and, if indicated, the public in affected areas. Development and evaluation of a combination antiviral regimen against these potential pandemic influenza strains are also now under way."[5]
Vaccines
A vaccine probably would not be available in the initial stages of population infection.[6] Once a potential virus is identified, it normally takes at least several months before a vaccine becomes widely available, as it must be developed, tested and authorized. The capability to produce vaccines varies widely from country to country; in fact, only 15 countries are listed as "Influenza vaccine manufacturers" according to the World Health Organization.[7] It is estimated that, in a best scenario situation, 750 million doses could be produced each year, whereas it is likely that each individual would need two doses of the vaccine in order to become immuno-competent. Distribution to and inside countries would probably be problematic.[8] Several countries, however, have well-developed plans for producing large quantities of vaccine. For example, Canadian health authorities say that they are developing the capacity to produce 32 million doses within four months, enough vaccine to inoculate every person in the country.[9]
There are two serious technical problems associated with the development of a vaccine against H5N1. The first problem is this: seasonal influenza vaccines require a single injection of 15 μg haemagglutinin in order to give protection; H5 seems to evoke only a weak immune response and a large multicentre trial found that two injections of 90 µg H5 given 28 days apart provided protection in only 54% of people (Treanor 2006). Even if it is considered that 54% is an acceptable level of protection, the world is currently capable of producing only 900 million doses at a strength of 15 μg (assuming that all production were immediately converted to manufacturing H5 vaccine); if two injections of 90 μg are needed then this capacity drops to only 70 million (Poland 2006). Trials using adjuvants such as alum or MF59 to try and lower the dose of vaccine are urgently needed. The second problem is this: there are two circulating clades of virus, clade 1 is the virus originally isolated in Vietnam, clade 2 is the virus isolated in Indonesia. Current vaccine research is focussed on clade 1 viruses, but the clade 2 virus is antigenically distinct and a clade 1 vaccine will probably not protect against a pandemic caused by clade 2 virus.
One tactic which can be used to accelerate vaccine validation is to review in a controlled manner the elicitation of immune responses to vaccine challenge. One approach to applying this tactic was reported in 2013 where a hemagglutinin protein microarray was used to examine the response to an influenza vaccine.[10]
Live attenuated influenza vaccine
In June 2007, the National Institutes of Health (NIH) began enrolling participants in a Phase 1 H5N1 study of an intranasal influenza vaccine candidate based on Flumist, MedImmune's live, attenuated vaccine technology.[11][12]
Reverse genetics
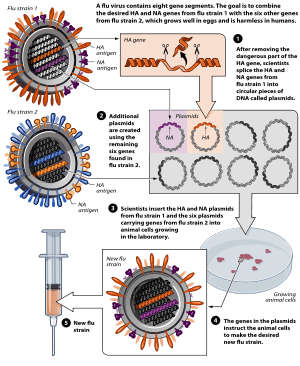
A technique called reverse genetics allows scientists to manipulate the genomes of influenza viruses and to transfer genes between viral strains. The technique allows the rapid generation of seed viruses for vaccine candidates that exactly match the anticipated epidemic strain. By removing or modifying certain virulence genes, reverse genetics also can be used to convert highly pathogenic influenza viruses into vaccine candidates that are safer for vaccine manufacturers to handle.
Cell culture
Another technique is use of cell cultures to grow vaccine strains; such as genetically engineering baculovirus to express a gene that encodes an influenza coat protein such as hemagglutinin or neuraminidase. "A recent NIAID-supported Phase II clinical trial of a vaccine produced by Protein Sciences Corporation using this strategy showed that it is well tolerated and immunogenic; the company is conducting further clinical evaluation of this product. Other new pathways for producing influenza vaccines include DNA-based approaches and the development of broadly protective vaccines based on influenza virus proteins that are shared by multiple strains."[5]
AVI Bio Pharma Inc. has evidence of inhibition of multiple subtypes of influenza A virus in cell culture with Morpholino oligomers from the results of their labs and four independent research laboratories. "The key finding here is that our NEUGENE(R) therapeutics continue to show efficacy against all strains of influenza A, including H5N1."[13][14] Morpholinos conjugated with cell penetrating peptides have been shown effective in protecting mice from influenza A.[15][16]
"Several companies are focusing on new vehicles for growing antigens, which are the bits of a virus or bacterium needed to spur a person's immune system to fight an infection. VaxInnate, a New Jersey-based biotechnology company, has reported success using E. coli bacteria, which can cause a sometimes-fatal infection but also can be used to grow vaccine ingredients when the harmful part of the bacterium is removed. Dowpharma, a unit of Dow Chemical, has been using different bacteria found in soil and water, P. fluorescens, which may make a higher volume of antigens more quickly than E. coli."[17] Also, a vaccine called FluBlOk, which is made in insect cells was granted FDA approval in January 2013. This vaccine, which focuses on hemagglutinin, would cut the production process by one to two months, as well as avoiding other pitfalls of chicken eggs.[18]
"The Committee for Medicinal Products for Human Use (CHMP), which reviews applications for 27 EU countries, found that Novartis's Optaflu vaccine, given to more than 3,400 people during clinical studies, met the CHMP's immunogenicity criteria [...] Novartis has said that Optaflu is a subunit vaccine, meaning it contains individual viral proteins rather than whole virus particles. [...] Novartis said it anticipates applying for US licensing of its cell-based flu vaccine in 2008. The company conducted phase 1 and 2 clinical trials of the vaccine in the United States and in July 2006 announced it would build a $600 million plant in Holly Springs, North Carolina, to make cell-culture flu vaccines. In May 2006, the United States Department of Health and Human Services awarded Novartis a $220 million contract to develop cell-based flu vaccines, and Novartis has said the money would go toward the cost of the new facility. Depending on when its vaccine is approved by the U.S. Food and Drug Administration (FDA), the plant could begin production as early as 2011 and be ready for full production as early as 2012, with an annual output of 50 million doses of a trivalent vaccine, the company has said. In the event of a flu pandemic, the facility is designed to have the capacity to make up to 150 million monovalent (single strain) doses each year within 6 months of a pandemic declaration, Novartis said. Novartis' other cell-based vaccine production facility is in Marburg, Germany."[19]
Pandemic flu vaccine planning
According to the United States Department of Health and Human Services (HHS) Pandemic Influenza Plan Appendix F: Current HHS Activities last revised on November 8, 2005:[20]
- Currently, influenza vaccine for the annual, seasonal influenza program comes from four manufacturers. However, only a single manufacturer produces the annual vaccine entirely within the U.S. Thus, if a pandemic occurred and existing U.S.-based influenza vaccine manufacturing capacity was completely diverted to producing a pandemic vaccine, supply would be severely limited. Moreover, because the annual influenza manufacturing process takes place during most of the year, the time and capacity to produce vaccine against potential pandemic viruses for a stockpile, while continuing annual influenza vaccine production, is limited. Since supply will be limited, it is critical for HHS to be able to direct vaccine distribution in accordance with predefined groups (see Appendix D); HHS will ensure the building of capacity and will engage states in a discussion about the purchase and distribution of pandemic influenza vaccine.
- Vaccine production capacity: The protective immune response generated by current influenza vaccines is largely based on viral hemagglutinin (HA) and neuraminidase (NA) antigens in the vaccine. As a consequence, the basis of influenza vaccine manufacturing is growing massive quantities of virus in order to have sufficient amounts of these protein antigens to stimulate immune responses. Influenza vaccines used in the United States and around world are manufactured by growing virus in fertilized hens’ eggs, a commercial process that has been in place for decades. To achieve current vaccine production targets millions of 11-day-old fertilized eggs must be available every day of production.
- In the near term, further expansion of these systems will provide additional capacity for the U.S.-based production of both seasonal and pandemic vaccines, however, the surge capacity that will be needed for a pandemic response cannot be met by egg-based vaccine production alone, as it is impractical to develop a system that depends on hundreds of millions of 11-day-old specialized eggs on a standby basis. In addition, because a pandemic could result from an avian influenza strain that is lethal to chickens, it is impossible to ensure that eggs will be available to produce vaccine when needed.
- In contrast, cell culture manufacturing technology can be applied to influenza vaccines as they are with most viral vaccines (e.g., polio vaccine, measles-mumps-rubella vaccine, chickenpox vaccine). In this system, viruses are grown in closed systems such as bioreactors containing large numbers of cells in growth media rather than eggs. The surge capacity afforded by cell-based technology is insensitive to seasons and can be adjusted to vaccine demand, as capacity can be increased or decreased by the number of bioreactors or the volume used within a bioreactor. In addition to supporting basic research on cell-based influenza vaccine development, HHS is currently supporting a number of vaccine manufacturers in the advanced development of cell-based influenza vaccines with the goal of developing U.S.-licensed cell-based influenza vaccines produced in the United States.
- Dose-sparing technologies. Current U.S.-licensed vaccines stimulate an immune response based on the quantity of HA (hemagglutinin) antigen included in the dose. Methods to stimulate a strong immune response using less HA antigen are being studied in H5N1 and H9N2 vaccine trials. These include changing the mode of delivery from intramuscular to intradermal and the addition of immune-enhancing adjuvant to the vaccine formulation. Additionally, HHS is soliciting contract proposals from manufacturers of vaccines, adjuvants, and medical devices for the development and licensure of influenza vaccines that will provide dose-sparing alternative strategies.
H5N1 vaccine research
 |

There are several H5N1 vaccines for several of the avian H5N1 varieties. H5N1 continually mutates rendering them, so far for humans, of little use. While there can be some cross-protection against related flu strains, the best protection would be from a vaccine specifically produced for any future pandemic flu virus strain. Dr. Daniel Lucey, co-director of the Biohazardous Threats and Emerging Diseases graduate program at Georgetown University has made this point, "There is no H5N1 pandemic so there can be no pandemic vaccine." However, "pre-pandemic vaccines" have been created; are being refined and tested; and do have some promise both in furthering research and preparedness for the next pandemic. Vaccine manufacturing companies are being encouraged to increase capacity so that if a pandemic vaccine is needed, facilities will be available for rapid production of large amounts of a vaccine specific to a new pandemic strain.
Problems with H5N1 vaccine production include:
- lack of overall production capacity
- lack of surge production capacity (it is impractical to develop a system that depends on hundreds of millions of 11-day-old specialized eggs on a standby basis)
- the pandemic H5N1 might be lethal to chickens
Cell culture (cell-based) manufacturing technology can be applied to influenza vaccines as they are with most viral vaccines and thereby solve the problems associated with creating flu vaccines using chicken eggs as is currently done. Researchers at the University of Pittsburgh have had success with a genetically engineered vaccine that took only a month to make and completely protected chickens from the highly pathogenic H5N1 virus.[21]
According to the United States Department of Health and Human Services:
- In addition to supporting basic research on cell-based influenza vaccine development, HHS is currently supporting a number of vaccine manufacturers in the advanced development of cell-based influenza vaccines with the goal of developing U.S.-licensed cell-based influenza vaccines produced in the United States. Dose-sparing technologies. Current U.S.-licensed vaccines stimulate an immune response based on the quantity of HA (hemagglutinin) antigen included in the dose. Methods to stimulate a strong immune response using less HA antigen are being studied in H5N1 and H9N2 vaccine trials. These include changing the mode of delivery from intramuscular to intradermal and the addition of immune-enhancing adjuvant to the vaccine formulation. Additionally, HHS is soliciting contract proposals from manufacturers of vaccines, adjuvants, and medical devices for the development and licensure of influenza vaccines that will provide dose-sparing alternative strategies.[22]
Chiron Corporation is now recertified and under contract with the National Institutes of Health to produce 8,000-10,000 investigational doses of Avian Flu (H5N1) vaccine. Aventis Pasteur is under similar contract. The United States government hopes to obtain enough vaccine in 2006 to treat 4 million people. However, it is unclear whether this vaccine would be effective against a hypothetical mutated strain that would be easily transmitted through human populations, and the shelflife of stockpiled doses has yet to be determined.[23]
The New England Journal of Medicine reported on March 30, 2006 on one of dozens of vaccine studies currently being conducted. The Treanor et al. study was on vaccine produced from the human isolate (A/Vietnam/1203/2004 H5N1) of a virulent clade 1 influenza A (H5N1) virus with the use of a plasmid rescue system, with only the hemagglutinin and neuraminidase genes expressed and administered without adjuvant. "The rest of the genes were derived from an avirulent egg-adapted influenza A/PR/8/34 strain. The hemagglutinin gene was further modified to replace six basic amino acids associated with high pathogenicity in birds at the cleavage site between hemagglutinin 1 and hemagglutinin 2. Immunogenicity was assessed by microneutralization and hemagglutination-inhibition assays with the use of the vaccine virus, although a subgroup of samples were tested with the use of the wild-type influenza A/Vietnam/1203/2004 (H5N1) virus." The results of this study combined with others scheduled to be completed by Spring 2007 is hoped will provide a highly immunogenic vaccine that is cross-protective against heterologous influenza strains.[24]
H5N1 vaccine approval and stockpiling
On April 17, 2007, the first US approval for H5N1 influenza vaccine for humans was given. This vaccine made by Sanofi-Aventis at a plant in Swiftwater, Pennsylvania is not to be sold commercially; instead the US is stockpiling it as an interim measure while better vaccines are being researched. Two injections given 28 days apart gave evidence of providing protection for 45 percent of the people who got the vaccine in a study. "The U.S. Department of Health and Human Services said it had already purchased 13 million doses of the Sanofi vaccine, enough to inoculate 6.5 million people. The vaccine was approved for people age 18 to 64. Studies in other age groups are ongoing. The most common side effects reported were pain at the injection site, headache, general ill feeling and muscle pain, the FDA said."[25]
This April 17, 2007 "approval by the Food and Drug Administration means the vaccine is no longer considered experimental and therefore could be dispensed during a pandemic without requiring each recipient to sign a form giving informed consent. [...] The two injections combined contain 180 micrograms of antigen, the piece of the H5N1 virus designed to spur immunity. By contrast, a conventional flu shot contains 45 micrograms of antigen: 15 micrograms for each of the three strains it protects against."[26]
The vaccine approved on April 17, 2007 "is based on an H5N1 virus isolated from a Vietnamese patient in 2004. Today's approval by the FDA follows a February 27 recommendation by an FDA advisory panel, which found that the vaccine was safe and effective. However, some of the panel members had reservations about the immunogenicity of the vaccine, which in data submitted to the panel was somewhat lower than previously reported in a 2006 article in the New England Journal of Medicine. In a clinical trial, two 90-microgram (mcg) doses of the vaccine, administered to 103 healthy adults 28 days apart, generated a protective immune response in 45% of recipients, the FDA noted. (The researchers used a neutralizing antibody titer of 1:40, a fourfold or more increase in antibody titer, to define adequate immune response.) [...] The national stockpile currently contains 13 million doses of the H5N1 vaccine, enough to vaccinate 6.5 million people [...] HHS has said it is moving forward with the development of a "clade 2" H5N1 vaccine, based on viruses that circulated in birds in China and Indonesia in 2003-04 and spread to the Middle East, Europe, and Africa in 2005 and 2006."[27]
Anti-viral drugs
Many nations, as well as the World Health Organization, are working to stockpile anti-viral drugs in preparation for a possible pandemic. Oseltamivir (trade name Tamiflu) is the most commonly sought drug, since it is available in pill form. Zanamivir (trade name Relenza) is also considered for use, but it must be inhaled. Other anti-viral drugs are less likely to be effective against pandemic influenza.
Both Tamiflu and Relenza are in short supply, and production capabilities are limited in the medium term. Some doctors say that co-administration of Tamiflu with probenecid could double supplies.[28]
There also is the potential of viruses to evolve drug resistance. Some H5N1-infected persons treated with oseltamivir have developed resistant strains of that virus.
Peramivir is a pharmaceutical drug used to treat viral infections. Like zanamivir and oseltamivir, peramivir is a neuraminidase inhibitor, acting as a transition-state analogue inhibitor of influenza neuraminidase and thereby preventing new viruses from emerging from infected cells. Experimental data indicate that peramivir may have useful activity against many viruses of interest, including H5N1 (avian bird flu), hepatitis B, polio, measles and smallpox. HHS Secretary Mike Leavitt announced on January 4, 2007 that the Department has awarded a $102.6 million, four-year contract to BioCryst Pharmaceuticals for advanced development of their influenza antiviral drug, peramivir.[29]
Several types of mushrooms have been discovered to have in vitro antiviral properties against influenza virus, including influenza virus type A.[30]
Spanish flu research
One hypothesis is that the virus strain originated at Fort Riley, Kansas, by two genetic mechanisms — genetic drift and antigenic shift — in viruses in poultry and swine which the fort bred for local consumption. But evidence from a recent reconstruction of the virus suggests that it jumped directly from birds to humans, without traveling through swine.[31] On October 5, 2005, researchers announced that the genetic sequence of the 1918 flu strain, a subtype of avian strain H1N1, had been reconstructed using historic tissue samples.[32][33][34] On 18 January 2007, Kobasa et al. reported that infected monkeys (Macaca fascicularis) exhibited classic symptoms of the 1918 pandemic and died from a cytokine storm.[35]
Distributed computing
One can share computer time for distributed research projects doing influenza research.
Folding@Home, a distributed computing program from Stanford University, is researching how viruses pass through the cell membrane (whereas most treatments focus on preventing viral replication) and what role proteins have. They are currently focussing their research on influenza.
Rosetta@Home is working on a Spanish flu inhibitor to block the flu infection.
See also
- Global Alliance for Vaccines and Immunization
- IFPMA International Federation of Pharmaceutical Manufacturers Associations
- Reporting disease cases
- Original antigenic sin
- Center for Biologics Evaluation and Research
- ICEID
- Influenza Genome Sequencing Project
- Cytokine storm
- International Partnership on Avian and Pandemic Influenza
- National Influenza Centers
- Pandemic Preparedness and Response Act
References
- ↑ Pandemic flu: fighting an enemy that is yet to exist Archived October 12, 2007, at the Wayback Machine. Catherine Brahic, Science and Development Network, May 4, 2006.
- ↑ Yahoo News AP article Bird Flu Vaccine Funding Awarded published May 4, 2006 .
- ↑ New York Times article ""Doubt Cast on Stockpile of a Vaccine for Bird Flu"" Archived January 15, 2016, at the Wayback Machine.
- ↑ ABC News Archived August 12, 2016, at the Wayback Machine.
- 1 2 The NIH Biomedical Research Response to Influenza Archived November 4, 2016, at the Wayback Machine.
- ↑ CDC Archived October 14, 2015, at the Wayback Machine.
- ↑ WHO Archived August 22, 2006, at the Wayback Machine.
- ↑ phacilitate.co.uk Archived July 17, 2006, at the Wayback Machine.
- ↑ Canada TV News Archived March 27, 2007, at the Wayback Machine.
- ↑ Desbian, Anthony L.; Van Hoeven, Neal; Reed, Steven J.; Casey, Allen C.; Laurance, John D.; Baldwin, Susan L.; Duthie, Malcolm S.; Reed, Steven G.; Carter, Darrick (2013). "Development of a high density hemagglutinin protein microarray to determine the breadth of influenza antibody responses". BioTechniques (papaer). 54 (6): 345–348. PMID 23750544. doi:10.2144/000114041.
- ↑ MedImmune Press release MedImmune and National Institutes of Health Begin Clinical Testing of a Live, Attenuated Intranasal Vaccine Against an H5N1 Avian Influenza Virus published June 15, 2006
- ↑ MedImmune And National Institutes Of Health Begin Clinical Testing Of A Live, Attenuated Intranasal Vaccine Against An H5N1 Avian Influenza Virus Article Date: 16 Jun 2006 "Archived copy". Archived from the original on 2011-05-16. Retrieved 2007-11-05.
- ↑ AVI BioPharma Reports Successful Inhibition of Multiple Subtypes of Influenza A Using NEUGENE Antisense Therapeutic
- ↑ Ge, Q; Pastey, M; Kobasa, D; Puthavathana, P; Lupfer, C; Bestwick, RK; Iversen, PL; Chen, J; Stein, DA (2006). "Inhibition of Multiple Subtypes of Influenza A Virus in Cell Cultures with Morpholino Oligomers". Antimicrob Agents Chemother. 50 (11): 3724–33. PMC 1635187
 . PMID 16966399. doi:10.1128/AAC.00644-06.
. PMID 16966399. doi:10.1128/AAC.00644-06. - ↑ Gabriel, G; Nordmann A; Stein DA; Iversen PL; Klenk HD (2008). "Morpholino oligomers targeting the PB1 and NP genes enhance the survival of mice infected with highly pathogenic influenza A H7N7 virus.". J Gen Virol. 89 (Pt 4): 939–48. PMID 18343835. doi:10.1099/vir.0.83449-0.
- ↑ Lupfer, C; Stein DA; Mourich DV; Tepper SE; Iversen PL; Pastey M (2008). "Inhibition of influenza A H3N8 virus infections in mice by morpholino oligomers.". Arch Virol. 153 (5): 929–37. PMID 18369525. doi:10.1007/s00705-008-0067-0.
- ↑ ABC News Archived May 2, 2009, at the Wayback Machine. article Scientists mull faster vaccine production published on April 12, 2006
- ↑ Bypassing eggs, flu vaccine grown in insect cells shows promise Archived January 15, 2016, at the Wayback Machine.
- ↑ CIDRAP Archived May 6, 2013, at the Wayback Machine. article Panel supports EU approval of cell-based flu vaccine published April 27, 2007
- ↑ "HHS Pandemic Influenza Plan. Appendix F: Current HHS Activities". United States Department of Health and Human Services. November 8, 2005. Archived from the original on 2007-02-14.
- ↑ Gao W, Soloff AC, Lu X, et al. (February 2006). "Protection of mice and poultry from lethal H5N1 avian influenza virus through adenovirus-based immunization". J. Virol. 80 (4): 1959–64. PMC 1367171
 . PMID 16439551. doi:10.1128/JVI.80.4.1959-1964.2006. [Quickie Bird Flu Vaccine Created Lay summary] Check
. PMID 16439551. doi:10.1128/JVI.80.4.1959-1964.2006. [Quickie Bird Flu Vaccine Created Lay summary] Check |laysummary=value (help). - ↑ Department of Health & Human Services Archived February 14, 2007, at the Wayback Machine.
- ↑ NPR Archived March 3, 2016, at the Wayback Machine.
- ↑ Poland GA (March 2006). "Vaccines against avian influenza—a race against time". N. Engl. J. Med. 354 (13): 1411–3. PMID 16571885. doi:10.1056/NEJMe068047.
- ↑ Scientific American article U.S. approves first bird flu vaccine for people published April 17, 2007
- ↑ The New York Times Archived May 20, 2013, at the Wayback Machine. article First Vaccine Against Avian Flu Is Approved as Interim Measure published April 18, 2007
- ↑ CIDRAP Archived May 3, 2013, at the Wayback Machine. article FDA approves first H5N1 vaccine published April 17, 2007
- ↑ Butler D (November 2005). "Wartime tactic doubles power of scarce bird-flu drug". Nature. 438 (7064): 6. Bibcode:2005Natur.438....6B. PMID 16267514. doi:10.1038/438006a.
- ↑ "Archived copy". Archived from the original on 2007-01-07. Retrieved 2007-01-06.
- ↑ Lindequist U, Niedermeyer TH, Jülich WD; Niedermeyer; Jülich (September 2005). "The pharmacological potential of mushrooms". Evid Based Complement Alternat Med. 2 (3): 285–99. PMC 1193547
 . PMID 16136207. doi:10.1093/ecam/neh107.
. PMID 16136207. doi:10.1093/ecam/neh107. - ↑ Sometimes a virus contains both avian adapted genes and human adapted genes. Both the H2N2 and H3N2 pandemic strains contained avian flu virus RNA segments. "While the pandemic human influenza viruses of 1957 (H2N2) and 1968 (H3N2) clearly arose through reassortment between human and avian viruses, the influenza virus causing the 'Spanish flu' in 1918 appears to be entirely derived from an avian source (Belshe 2005)." (from Chapter Two : Avian Influenza by Timm C. Harder and Ortrud Werner Archived May 10, 2016, at the Wayback Machine., an excellent free on-line Book called Influenza Report 2006 which is a medical textbook that provides a comprehensive overview of epidemic and pandemic influenza.)
- ↑ "The 1918 flu virus is resurrected". Nature. 437 (7060): 794–5. October 2005. Bibcode:2005Natur.437..794.. PMID 16208326. doi:10.1038/437794a.
- ↑ Taubenberger, Jeffery K.; Ann H. Reid, Raina M. Lourens, Ruixue Wang, Guozhong Jin and Thomas G. Fanning; Lourens, Raina M.; Wang, Ruixue; Jin, Guozhong; Fanning, Thomas G. (2005). "Characterization of the 1918 influenza virus polymerase genes". Nature. 437 (7060): 889–893. Bibcode:2005Natur.437..889T. PMID 16208372. doi:10.1038/nature04230.
- ↑ Tumpey, Terrence M.; Peter Palese; Aguilar, Patricia V.; Zeng, Hui; Solórzano, Alicia; Swayne, David E.; Cox, Nancy J.; Katz, Jacqueline M.; Taubenberger, Jeffery K.; Palese, Peter; García-Sastre, Adolfo (2005). "Characterization of the Reconstructed 1918 Spanish Influenza Pandemic Virus". Science. 310 (5745): 77–80. Bibcode:2005Sci...310...77T. PMID 16210530. doi:10.1126/science.1119392.
- ↑ Kobasa D, Jones SM, Shinya K; et al. (January 2007). "Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus". Nature. 445 (7125): 319–23. Bibcode:2007Natur.445..319K. PMID 17230189. doi:10.1038/nature05495.
External links
- Influenza Research Database – Database of influenza genomic sequences and related information.
- Health-EU portal EU response to influenza
Further reading
- WHO's assessment of FLU RESEARCH as of November 2006
- OIE Scientific and Technical Review — Animal vaccination