Electrocardiography
| Electrocardiography | |
|---|---|
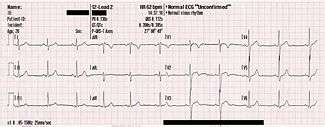
 ECG of a heart in normal sinus rhythm. | |
| ICD-9-CM | 89.52 |
| MeSH | D004562 |
| MedlinePlus | 003868 |
Electrocardiography (ECG or EKG[lower-alpha 1]) is the process of recording the electrical activity of the heart over a period of time using electrodes placed on the skin. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle's electrophysiologic pattern of depolarizing and repolarizing during each heartbeat. It is a very commonly performed cardiology test.
In a conventional 12-lead ECG, 10 electrodes are placed on the patient's limbs and on the surface of the chest. The overall magnitude of the heart's electrical potential is then measured from 12 different angles ("leads") and is recorded over a period of time (usually 10 seconds). In this way, the overall magnitude and direction of the heart's electrical depolarization is captured at each moment throughout the cardiac cycle.[4] The graph of voltage versus time produced by this noninvasive medical procedure is referred to as an electrocardiogram.
During each heartbeat, a healthy heart has an orderly progression of depolarization that starts with pacemaker cells in the sinoatrial node, spreads out through the atrium, passes through the atrioventricular node down into the bundle of His and into the Purkinje fibers, spreading down and to the left throughout the ventricles. This orderly pattern of depolarization gives rise to the characteristic ECG tracing. To the trained clinician, an ECG conveys a large amount of information about the structure of the heart and the function of its electrical conduction system.[5] Among other things, an ECG can be used to measure the rate and rhythm of heartbeats, the size and position of the heart chambers, the presence of any damage to the heart's muscle cells or conduction system, the effects of cardiac drugs, and the function of implanted pacemakers.[6]
History
The etymology of the word is derived from the Greek electro, because it is related to electrical activity, kardio, Greek for heart, and graph, a Greek root meaning "to write".
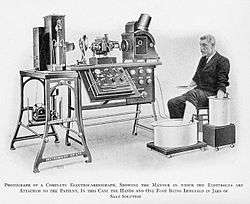
Alexander Muirhead is reported to have attached wires to a feverish patient's wrist to obtain a record of the patient's heartbeat in 1872 at St Bartholomew's Hospital.[7] Another early pioneer was Augustus Waller, of St Mary's Hospital in London.[8] His electrocardiograph machine consisted of a Lippmann capillary electrometer fixed to a projector. The trace from the heartbeat was projected onto a photographic plate that was itself fixed to a toy train. This allowed a heartbeat to be recorded in real time.
An initial breakthrough came when Willem Einthoven, working in Leiden, the Netherlands, used the string galvanometer (the first practical electrocardiograph) he invented in 1901.[9] This device was much more sensitive than both the capillary electrometer Waller used and the string galvanometer that had been invented separately in 1897 by the French engineer Clément Ader.[10] Einthoven had previously, in 1895, assigned the letters P, Q, R, S, and T to the deflections in the theoretical waveform he created using equations which corrected the actual waveform obtained by the capillary electrometer to compensate for the imprecision of that instrument. Using letters different from A, B, C, and D (the letters used for the capillary electrometer's waveform) facilitated comparison when the uncorrected and corrected lines were drawn on the same graph.[11] Einthoven probably chose the initial letter P to follow the example set by Descartes in geometry.[11] When a more precise waveform was obtained using the string galvanometer, which matched the corrected capillary electrometer waveform, he continued to use the letters P, Q, R, S, and T,[11] and these letters are still in use today. Einthoven also described the electrocardiographic features of a number of cardiovascular disorders. In 1924, he was awarded the Nobel Prize in Medicine for his discovery.[12]
In 1937, Taro Takemi invented the first portable electrocardiograph machine.[13]
Though the basic principles of that era are still in use today, many advances in electrocardiography have been made over the years. Instrumentation has evolved from a cumbersome laboratory apparatus to compact electronic systems that often include computerized interpretation of the electrocardiogram.[14]
Medical uses
The overall goal of performing electrocardiography is to obtain information about the structure and function of the heart. Medical uses for this information are varied and generally relate to having a need for knowledge of the structure and/or function. Some indications for performing electrocardiography include:
- Suspected myocardial infarction (heart attack) or new chest pain
- Suspected pulmonary embolism or new shortness of breath
- A third heart sound, fourth heart sound, a cardiac murmur[15] or other findings to suggest structural heart disease
- Perceived cardiac dysrhythmias[15] either by pulse or palpitations
- Monitoring of known cardiac dysrhythmias
- Fainting or collapse[15]
- Seizures[15]
- Monitoring the effects of a heart medication (e.g. drug-induced QT prolongation)
- Assessing severity of electrolyte abnormalities, such as hyperkalemia
- Hypertrophic cardiomyopathy screening in adolescents as part of a sports physical out of concern for sudden cardiac death (varies by country)
- Perioperative monitoring in which any form of anesthesia is involved (e.g. monitored anesthesia care, general anesthesia); typically both intraoperative and postoperative
- As a part of a pre-operative assessment some time before a surgical procedure (especially for those with known cardiovascular disease or who are undergoing invasive or cardiac, vascular or pulmonary procedures, or who will receive general anesthesia)
- Cardiac stress testing
- Computed tomography angiography (CTA) and Magnetic resonance angiography (MRA) of the heart (ECG is used to "gate" the scanning so that the anatomical position of the heart is steady)
- Biotelemetry of patients for any of the above reasons and such monitoring can include internal and external defibrillators and pacemakers
The United States Preventive Services Task Force does not recommend electrocardiography for routine screening procedure in patients without symptoms and those at low risk for coronary heart disease.[16][17] This is because an ECG may falsely indicate the existence of a problem, leading to misdiagnosis, the recommendation of invasive procedures, or overtreatment. However, persons employed in certain critical occupations, such as aircraft pilots,[18] may be required to have an ECG as part of their routine health evaluations.
Continuous ECG monitoring is used to monitor critically ill patients, patients undergoing general anesthesia,[15] and patients who have an infrequently occurring cardiac dysrhythmia that would be unlikely to be seen on a conventional ten second ECG.
Performing a 12-lead ECG in the United States is commonly performed by specialized technicians that may be certified electrocardiogram technicians. ECG interpretation is a component of many healthcare fields (nurses and physicians and cardiac surgeons being the most obvious) but anyone trained to interpret an ECG is free to do so. However, "official" interpretation is performed by a cardiologist. Certain fields such as anesthesia utilize continuous ECG monitoring and knowledge of interpreting ECGs is crucial to their jobs.
One additional form of electrocardiography is used in clinical cardiac electrophysiology in which a catheter is used to measure the electrical activity. The catheter is inserted through the femoral vein and can have several electrodes along its length to record the direction of electrical activity from within the heart..
Electrocardiographs
.jpg)
An electrocardiograph is a machine that is used to perform electrocardiography, and produces the electrocardiogram. The first electrocardiographs are discussed above and are electrically primitive compared to today's machines.
The fundamental component to electrocardiograph is the Instrumentation amplifier, which is responsible for taking the voltage difference between leads (see below) and amplifying the signal. ECG voltages measured across the body are on the order of hundreds of microvolts up to 1 millivolt (the small square on a standard ECG is 100 microvolts). This low voltage necessitates a low noise circuit and instrumentation amplifiers are key.
Early electrocardiographs were constructed with analog electronics and the signal could drive a motor to print the signal on paper. Today, electrocardiographs use analog-to-digital converters to convert to a digital signal that can then be manipulated with digital electronics. This permits digital recording of ECGs and use on computers.
There are other components to the electrocardiograph:[19]
- Safety features that include voltage protection for the patient and operator. Since the machines are powered by mains power, it is conceivable that either person could be subjected to voltage capable of causing death. Additionally, the heart is sensitive to the AC frequencies typically used for mains power (50 or 60 Hz).
- Defibrillation protection. Any ECG used in healthcare may be attached to a person who requires defibrillation and the electrocardiograph needs to protect itself from this source of energy.
- Electrostatic discharge is similar to defibrillation discharge and requires voltage protection up to 18,000 volts.
- Additionally circuitry called the right leg driver can be used to reduce common-mode interference (typically the 50/60 Hz mains power).
Typical design for a portable electrocardiograph is a combined unit that includes a screen, keyboard, and printer on a small wheeled cart. The unit connects to a long cable that branches to each lead which attaches to a conductive pad on the patient.
Lastly, the electrocardiograph may include a rhythm analysis algorithm that produces a computerized interpretation of the electrocardiogram. The results from these algorithms are considered "preliminary" until verified and/or modified by someone trained in interpreting electrocardiograms. Included in this analysis is computation of common parameters that include PR interval, QT duration, corrected QT (QTc) duration, PR axis, QRS axis, and more. Earlier designs recorded each lead sequentially but current designs employ circuits that can record all leads simultaneously. The former introduces problems in interpretation since there may be beat-to-beat changes in the rhythm that makes it unwise to compare across beats.
Electrodes and leads
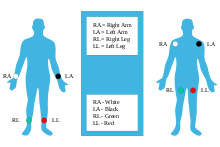
A "lead" is not the same as an "electrode". Whereas an electrode is a conductive pad in contact with the body that makes an electrical circuit with the electrocardiograph, a lead is a connector to an electrode. Since leads can share the same electrode, a standard 12-lead EKG happens to need only 10 electrodes (as listed in the table below).
A lead is slightly more abstract and is the source of measurement of a vector. For the limb leads, they are "bipolar" and are the comparison between two electrodes. For the precordial leads, they are "unipolar" and compared to a common lead (commonly the Wilson's central terminal), as described below.[21]
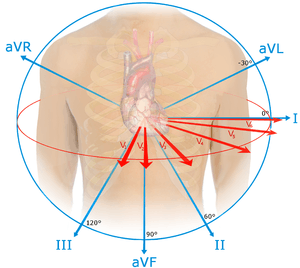
Leads are broken down into three sets: limb; augmented limb; and precordial. The 12-lead EKG has a total of three limb leads and three augmented limb leads arranged like spokes of a wheel in the coronal plane (vertical) and six precordial leads that lie on the perpendicular transverse plane (horizontal).
In medical settings, the term leads is also sometimes used to refer to the electrodes themselves, although this is not technically a correct usage of the term, which complicates the understanding of difference between the two.
The 10 electrodes in a 12-lead EKG are listed below.[22]
| Electrode name | Electrode placement |
|---|---|
| RA | On the right arm, avoiding thick muscle. |
| LA | In the same location where RA was placed, but on the left arm. |
| RL | On the right leg, lower end of medial aspect of calf muscle. (Avoid bony prominences) |
| LL | In the same location where RL was placed, but on the left leg. |
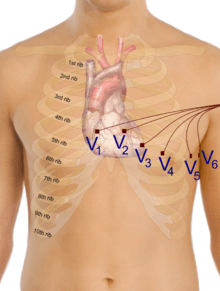
| V1 | In the fourth intercostal space (between ribs 4 and 5) just to the right of the sternum (breastbone). |
| V2 | In the fourth intercostal space (between ribs 4 and 5) just to the left of the sternum. |
| V3 | Between leads V2 and V4. |
| V4 | In the fifth intercostal space (between ribs 5 and 6) in the mid-clavicular line. |
| V5 | Horizontally even with V4, in the left anterior axillary line. |
| V6 | Horizontally even with V4 and V5 in the midaxillary line. |
Two common electrodes used are a flat paper-thin sticker and a self-adhesive circular pad. The former are typically used in a single ECG recording while the latter are for continuous recordings as they stick longer. Each electrode consists of an electrically conductive electrolyte gel and a silver/silver chloride conductor.[23] The gel typically contains potassium chloride — sometimes silver chloride as well — to permit electron conduction from the skin to the wire and to the electrocardiogram.
The common lead, Wilson's central terminal VW, is produced by averaging the measurements from the electrodes RA, LA, and LL to give an average potential across the body:
In a 12-lead ECG, all leads except the limb leads are unipolar (aVR, aVL, aVF, V1, V2, V3, V4, V5, and V6). The measurement of a voltage requires two contacts and so, electrically, the unipolar leads are measured from the common lead (negative) and the unipolar lead (positive). This averaging for the common lead and the abstract unipolar lead concept makes for a more challenging understanding and is complicated by sloppy usage of "lead" and "electrode".
Limb leads

Leads I, II and III are called the limb leads. The electrodes that form these signals are located on the limbs—one on each arm and one on the left leg.[24][25][26] The limb leads form the points of what is known as Einthoven's triangle.[27]
- Lead I is the voltage between the (positive) left arm (LA) electrode and right arm (RA) electrode:
- Lead II is the voltage between the (positive) left leg (LL) electrode and the right arm (RA) electrode:
- Lead III is the voltage between the (positive) left leg (LL) electrode and the left arm (LA) electrode:
Augmented limb leads
Leads aVR, aVL, and aVF are the augmented limb leads. They are derived from the same three electrodes as leads I, II, and III, but they use Goldberger's central terminal as their negative pole. Goldberger's central terminal is a combination of inputs from two limb electrodes, with a different combination for each augmented lead. It is referred to immediately below as "the negative pole".
- Lead augmented vector right (aVR)' has the positive electrode on the right arm. The negative pole is a combination of the left arm electrode and the left leg electrode:
- Lead augmented vector left (aVL) has the positive electrode on the left arm. The negative pole is a combination of the right arm electrode and the left leg electrode:
- Lead augmented vector foot (aVF) has the positive electrode on the left leg. The negative pole is a combination of the right arm electrode and the left arm electrode:
Together with leads I, II, and III, augmented limb leads aVR, aVL, and aVF form the basis of the hexaxial reference system, which is used to calculate the heart's electrical axis in the frontal plane.
Precordial leads
The precordial leads lie in the transverse (horizontal) plane, perpendicular to the other six leads. The six precordial electrodes act as the positive poles for the six corresponding precordial leads: (V1, V2, V3, V4, V5 and V6). Wilson's central terminal is used as the negative pole.
Specialized leads
Additional electrodes may rarely be placed to generate other leads for specific diagnostic purposes. Right-sided precordial leads may be used to better study pathology of the right ventricle or for dextrocardia (and are denoted with an R (e.g., V5R)). Posterior leads (V7 to V9) may be used to demonstrate the presence of a posterior myocardial infarction. A Lewis lead (requiring an electrode at the right sternal border in the second intercostal space) can be used to study pathological rhythms arising in the right atrium.
An esophogeal lead can be inserted to a part of the esophagus where the distance to the posterior wall of the left atrium is only approximately 5–6 mm (remaining constant in people of different age and weight).[28] An esophageal lead avails for a more accurate differentiation between certain cardiac arrhythmias, particularly atrial flutter, AV nodal reentrant tachycardia and orthodromic atrioventricular reentrant tachycardia.[29] It can also evaluate the risk in people with Wolff-Parkinson-White syndrome, as well as terminate supraventricular tachycardia caused by re-entry.[29]
An intracardiac electrogram (ICEG) is essentially an ECG with some added intracardiac leads (that is, inside the heart). The standard ECG leads (external leads) are I, II, III, aVL, V1, and V6. Two to four intracardiac leads are added via cardiac catheterization. The word "electrogram" (EGM) without further specification usually means an intracardiac electrogram.
Lead locations on an ECG report
A standard 12-lead ECG report (an electrocardiograph) shows a 2.5 second tracing of each of the twelve leads. The tracings are most commonly arranged in a grid of four columns and three rows. the first column is the limb leads (I,II, and III), the second column is the augmented limb leads (aVR, aVL, and aVF), and the last two columns are the precordial leads (V1-V6). Additionally, a rhythm strip may be included as a fourth or fifth row.
The timing across the page is continuous and not tracings of the 12 leads for the same time period. In other words, if the output were traced by needles on paper, each row would switch which leads as the paper is pulled under the needle. For example, the top row would first trace lead I, then switch to lead aVR, then switch to V1, and then switch to V4 and so none of these four tracings of the leads are from the same time period as they are traced in sequence through time.
Contiguity of leads
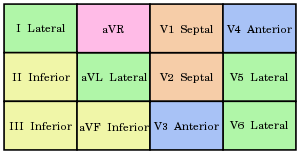
Each of the 12 ECG leads records the electrical activity of the heart from a different angle, and therefore align with different anatomical areas of the heart. Two leads that look at neighboring anatomical areas are said to be contiguous.
| Category | Leads | Activity |
|---|---|---|
| Inferior leads' | Leads II, III and aVF | Look at electrical activity from the vantage point of the inferior surface (diaphragmatic surface of heart) |
| Lateral leads | I, aVL, V5 and V6 | Look at the electrical activity from the vantage point of the lateral wall of left ventricle |
| Septal leads | V1 and V2 | Look at electrical activity from the vantage point of the septal surface of the heart (interventricular septum) |
| Anterior leads | V3 and V4 | Look at electrical activity from the vantage point of the anterior wall of the right and left ventricles (Sternocostal surface of heart) |
In addition, any two precordial leads next to one another are considered to be contiguous. For example, though V4 is an anterior lead and V5 is a lateral lead, they are contiguous because they are next to one another.
Electrophysiology
The formal study of the electrical conduction system of the heart is called cardiac electrophysiology (EP). An electrophysiology study involves a formal study of the conduction system and can be done for various reasons. During such a study, catheters are used to access the heart and some of these catheters include electrodes that can be placed anywhere in the heart to record the electrical activity from within the heart. Some catheters contain several electrodes and can record the propagation of electrical activity.
Interpretation
Interpretation of the ECG is fundamentally about understanding the electrical conduction system of the heart. Normal conduction starts and propagates in a predictable pattern, and deviation from this pattern can be a normal variation or be pathological. An ECG does not equate with mechanical pumping activity of the heart, for example, pulseless electrical activity produces an ECG that should pump blood but no pulses are felt (and constitutes a medical emergency and CPR should be performed). Ventricular fibrillation produces an ECG but is too dysfunctional to produce a life-sustaining cardiac output. Certain rhythms are known to have good cardiac output and some are known to have bad cardiac output. Ultimately, an echocardiogram or other anatomical imaging modality is useful in assessing the mechanical function of the heart.
Like all medical tests, what constitutes "normal" is based on population studies. The heart rate range of between 60 and 100 is considered normal since data shows this to be the usual resting heart rate.
Theory

Interpretation of the ECG is ultimately that of pattern recognition. In order to understand the patterns found, it is helpful to understand the theory of what ECGs represent. The theory is rooted in electromagnetics and boils down to the four following points:
- depolarization of the heart toward the positive electrode produces a positive deflection
- depolarization of the heart away from the positive electrode produces a negative deflection
- repolarization of the heart toward the positive electrode produces a negative deflection
- repolarization of the heart away from the positive electrode produces a positive deflection
Thus, the overall direction of depolarization and repolarization produces a vector that produces positive or negative deflection on the ECG depending on which lead it points to. For example, depolarizing from right to left would produce a positive deflection in lead I because the two vectors point in the same direction. In contrast, that same depolarization would produce minimal deflection in V1 and V2 because the vectors are perpendicular and this phenomenon is called isoelectric.
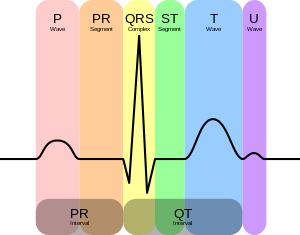
Normal rhythm produces four entities — a P wave, a QRS complex, a T wave, and a U wave — that each have a fairly unique pattern.
- The P wave represents atrial depolarization.
- The QRS complex represents ventricular depolarization.
- The T wave represents ventricular repolarization.
- The U wave represents papillary muscle repolarization.
However, the U wave is not typically seen and its absence is generally ignored. Changes in the structure of the heart and its surroundings (including blood composition) change the patterns of these four entities.
Electrocardiogram grid
ECG's are normally printed on a grid. The horizontal axis represents time and the vertical axis represents voltage. The standard values on this grid are shown in the adjacent image:
- A small box is 1 mm x 1 mm big and represents 0.1 mV x 0.04 seconds.
- A large box is 5 mm x 5mm big and represents 0.5 mV x 0.2 seconds wide.
The "large" box is represented by a heavier line weight than the small boxes.

Not all aspects of an ECG rely on precise recordings or having a known scaling of amplitude or time. For example, determining if the tracing is a sinus rhythm only requires feature recognition and matching, and not measurement of amplitudes or times (i.e., the scale of the grids are irrelevant). An example to the contrary, the voltage requirements of left ventricular hypertrophy require knowing the grid scale.
Rate and rhythm
In a normal heart, the heart rate is the rate in which the sinoatrial node depolarizes as it is the source of depolarization of the heart. Heart rate, like other vital signs like blood pressure and respiratory rate, change with age. In adults, a normal heart rate is between 60 and 100 beats per minute (normocardic) where in children it is higher. A heart rate less than normal is called bradycardia (<60 in adults) and higher than normal is tachycardia (>100 in adults). A complication of this is when the atria and ventricles are not in synchrony and the "heart rate" must be specified as atrial or ventricular (e.g., atrial rate in atrial fibrillation is 300–600 bpm, whereas ventricular rate can be normal (60–100) or faster (100–150)).
In normal resting hearts, the physiologic rhythm of the heart is normal sinus rhythm (NSR). Normal sinus rhythm produces the prototypical pattern of P wave, QRS complex, and T wave. Generally, deviation from normal sinus rhythm is considered a cardiac arrhythmia. Thus, the first question in interpreting an ECG is whether or not there is a sinus rhythm. A criterion for sinus rhythm is that P waves and QRS complexes appear 1-to-1, thus implying that the P wave causes the QRS complex.
Once sinus rhythm is established, or not, the second question is the rate. For a sinus rhythm this is either the rate of P waves or QRS complexes since they are 1-to-1. If the rate is too fast then it is sinus tachycardia and if it is too slow then it is sinus bradycardia.
If it is not a sinus rhythm, then determining the rhythm is necessary before proceeding with further interpretation. Some arrhythmias with characteristic findings:
- Absent P waves with "irregularly irregular" QRS complexes is the hallmark of atrial fibrillation
- A "saw tooth" pattern with QRS complexes is the hallmark of atrial flutter
- Sine wave pattern is the hallmark of ventricular flutter
- Absent P waves with wide QRS complexes with fast rate is ventricular tachycardia
Determination of rate and rhythm is necessary in order to make sense of further interpretation.
Axis
The heart has several axes, but the most common by far is the axis of the QRS complex (references to "the axis" implicitly means the QRS axis). Each axis can be computationally determined to result in a number representing degrees of deviation from zero, or it can be categorized into a few types.
The QRS axis is the general direction of the ventricular depolarization wavefront (or mean electrical vector) in the frontal plane. It is often sufficient to classify the axis as one of three types: normal, left deviated, or right deviated. Population data shows that normal QRS axis is from −30° to 105° with 0° being along lead I and positive being inferior and negative being superior (best understood graphically as the hexaxial reference system).[30] Beyond +105° is right axis deviation and beyond −30° is left axis deviation (the third quadrant of −90° to −180° is very rare and is an indeterminate axis). A shortcut for determining if the QRS axis is normal is if the QRS complex is mostly positive in lead I and lead II (or lead I and aVF if +90° is the upper limit of normal).
The normal QRS axis is generally down and to the left, following the anatomical orientation of the heart within the chest. An abnormal axis suggests a change in the physical shape and orientation of the heart, or a defect in its conduction system that causes the ventricles to depolarize in an abnormal way.
| Classification | Angle | Notes |
|---|---|---|
| Normal | −30° to 105° | Normal |
| Left axis deviation | −30° to −90° | May indicate left ventricular hypertrophy, left anterior fascicular block, or an old inferior q-wave myocardial infarction |
| Right axis deviation | +105° to +180° | May indicate right ventricular hypertrophy, left posterior fascicular block, or an old lateral q-wave myocardial infarction |
| Indeterminate axis | +180° to −90° | Rarely seen; considered an 'electrical no-man's land' |
The extent of normal axis can be +90° or 105° depending on the source.
Amplitudes and intervals

All of the waves on an EKG tracing and the intervals between them have a predictable time duration, a range of acceptable amplitudes (voltages), and a typical morphology. Any deviation from the normal tracing is potentially pathological and therefore of clinical significance.
For ease of measuring the amplitudes and intervals, an EKG is printed on graph paper at a standard scale: each 1 mm (one small box on the standard EKG paper) represents 40 milliseconds of time on the x-axis, and 0.1 millivolts on the y-axis.
| Feature | Description | Pathology | Duration |
|---|---|---|---|
| P wave | The p-wave represents depolarization of the atria. Atrial depolarization spreads from the SA node towards the AV node, and from the right atrium to the left atrium. | The p-wave is typically upright in most leads except for aVR; an unusual p-wave axis (inverted in other leads) can indicate an ectopic atrial pacemaker. If the p wave is of unusually long duration, it may represent atrial enlargement. Typically a large right atrium gives a tall, peaked p-wave while a large left atrium gives a two-humped bifid p-wave. | <80 ms |
| PR interval | The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex. This interval reflects the time the electrical impulse takes to travel from the sinus node through the AV node. | A PR interval shorter than 120 ms suggests that the electrical impulse is bypassing the AV node, as in Wolf-Parkinson-White syndrome. A PR interval consistently longer than 200 ms diagnoses first degree atrioventricular block. The PR segment (the portion of the tracing after the p-wave and before the QRS complex) is typically completely flat, but may be depressed in pericarditis. | 120 to 200 ms |
| QRS complex | The QRS complex represents the rapid depolarization of the right and left ventricles. The ventricles have a large muscle mass compared to the atria, so the QRS complex usually has a much larger amplitude than the P-wave. | If the QRS complex is wide (longer than 120 ms) it suggests disruption of the heart's conduction system, such as in LBBB, RBBB, or ventricular rhythms such as ventricular tachycardia. Metabolic issues such as severe hyperkalemia, or TCA overdose can also widen the QRS complex. An unusually tall QRS complex may represent left ventricular hypertrophy while a very low-amplitude QRS complex may represent a pericardial effusion or infiltrative myocardial disease. | 80 to 100 ms |
| J-point | The J-point is the point at which the QRS complex finishes and the ST segment begins. | The J point may be elevated as a normal variant. The appearance of a separate J wave or Osborn wave at the J point is pathognomonic of hypothermia or hypercalcemia.[31] | |
| ST segment | The ST segment connects the QRS complex and the T wave; it represents the period when the ventricles are depolarized. | It is usually isoelectric, but may be depressed or elevated with myocardial infarction or ischemia. ST depression can also be caused by LVH or digoxin. ST elevation can also be caused by pericarditis, Brugada syndrome, or can be a normal variant (J-point elevation). | |
| T wave | The T wave represents the repolarization of the ventricles. It is generally upright in all leads except aVR and lead V1. | Inverted T waves can be a sign of myocardial ischemia, LVH, high intracranial pressure, or metabolic abnormalities. Peaked T waves can be a sign of hyperkalemia or very early myocardial infarction. | 160 ms |
| Corrected QT interval (QTc) | The QT interval is measured from the beginning of the QRS complex to the end of the T wave. Acceptable ranges vary with heart rate, so it must be corrected to the QTc by dividing by the square root of the RR interval. | A prolonged QTc interval is a risk factor for ventricular tachyarrhythmias and sudden death. Long QT can arise as a genetic syndrome, or as a side effect of certain medications. An unusually short QTc can be seen in severe hypercalcemia. | <440 ms |
| U wave | The U wave is hypothesized to be caused by the repolarization of the interventricular septum. It normally has a low amplitude, and even more often is completely absent. | If the U wave is very prominent, suspect hypokalemia, hypercalcemia or hyperthyroidism.[32] | |
Ischemia and infarction
Ischemia or non-ST elevation myocardial infarctions may manifest as ST depression or inversion of T waves. It may also affect the high frequency band of the QRS.
ST elevation myocardial infarctions have different characteristic ECG findings based on the amount of time elapsed since the MI first occurred. The earliest sign is hyperacute T waves, peaked T-waves due to local hyperkalemia in ischemic myocardium. This then progresses over a period of minutes to elevations of the ST segment by at least 1 mm. Over a period of hours, a pathologic Q wave may appear and the T wave will invert. Over a period of days the ST elevation will resolve. Pathologic q waves generally will remain permanently.[33]
The coronary artery that has been occluded can be identified in an ST-elevation myocardial infarction based on the location of ST elevation. The LAD supplies the anterior wall of the heart, and therefore causes ST elevations in anterior leads (V1 and V2). The LCx supplies the lateral aspect of the heart and therefore causes ST elevations in lateral leads (I, aVL and V6). The RCA usually supplies the inferior aspect of the heart, and therefore causes ST elevations in inferior leads (II, III and aVF).
Artifacts
An EKG tracing is affected by patient motion. Some rhythmic motions (such as shivering or tremors) can create the illusion of cardiac dysrhythmia.[34] Artifacts are distorted signals caused by a secondary internal or external sources, such as muscle movement or interference from an electrical device.[35][36]
Distortion poses significant challenges to healthcare providers,[35] who employ various techniques[37] and strategies to safely recognize[38] these false signals. Accurately separating the ECG artifact from the true ECG signal can have a significant impact on patient outcomes and legal liabilities.[39]
Improper lead placement (for example, reversing two of the limb leads) has been estimated to occur in 0.4% to 4% of all EKG recordings,[40] and has resulted in improper diagnosis and treatment including unnecessary use of thrombolytic therapy.[41][42]
Diagnosis
Numerous diagnosis and findings can be made based upon electrocardiography and many are discussed above. The following is an organized list of these and more.
Rhythm disturbances/ Arrhythmias:
- Atrial fibrillation & atrial flutter without rapid ventricular response
- Premature atrial contraction (PACs) & Premature ventricular contraction (PVCs)
- Sinus arrhythmia
- Sinus bradycardia & sinus tachycardia
- Sinus pause & sinoatrial arrest
- Sick sinus syndrome: bradycardia-tachycardia syndrome
- Supraventricular tachycardia
- Atrial fibrillation (afib) with rapid ventricular response
- Atrial flutter with rapid ventricular response
- AV nodal reentrant tachycardia
- Atrioventricular reentrant tachycardia
- Junctional ectopic tachycardia
- Atrial tachycardia
- Sinoatrial nodal reentrant tachycardia
- Torsades de pointes (polymorphic ventricular tachycardia)
- Wide complex tachycardia
- Ventricular flutter
- Ventricular fibrillation
- Ventricular tachycardia (monomorphic ventricular tachycardia)
- Pre-excitation syndrome
Heart block and conduction problems:
- Aberration
- Brugada syndrome
- First-degree AV block, Second-degree AV block (Mobitz I & II), Third-degree AV block
- Left anterior & left posterior fascicular block; bifasciular block and trifasciular blocks
- Incomplete and complete right bundle branch block (RBBB)
- Incomplete and complete Left bundle branch block (LBBB)
- Long QT syndrome
- Right and left atrial abnormality
Electrolytes disturbances & intoxication:
- Digitalis intoxication
- Calcium: hypocalcemia and hypercalcemia
- Potassium: hypokalemia and hyperkalemia
Ischemia and infarction:
- ST elevation and ST depression
- High Frequency QRS changes
- Myocardial infarction (heart attack)
Structural:
See also
- Electrical conduction system of the heart
- Electrogastrogram
- Electropalatography
- Electroretinography
- Heart rate monitor
- Emergency medicine
Notes
- ↑ The version with -K-, which is rarer in British English than in American English, is an early-20th-century loanword from the German acronym EKG for Elektrokardiogramm (electrocardiogram),[1] which reflects that German physicians were pioneers in the field at the time. Today AMA style and, under its stylistic influence, most American medical publications use ECG instead of EKG.[2] The German term Elektrokardiogramm as well as the English equivalent electrocardiogram consist of the New Latin/international scientific vocabulary elements elektro- (cognate electro-) and kardi- (cognate cardi-), the latter from Greek kardia (heart).[3] The -K- version is more often retained under circumstances where there may be verbal confusion between ECG and EEG (electroencephalography) due to similar pronunciation.
References
- ↑ EKG. Oxford Online Dictionaries
- ↑ American Medical Association, "15.3.1 Electrocardiographic Terms", AMA Manual of Style
- ↑ Merriam-Webster. "Merriam-Webster's Collegiate Dictionary". Merriam-Webster.
- ↑ "ECG- simplified. Aswini Kumar M.D.". LifeHugger. Retrieved 11 February 2010.
- ↑ Walraven, G. (2011). Basic arrhythmias (7th ed.), pp. 1–11
- ↑ Braunwald E. (ed) (1997), Heart Disease: A Textbook of Cardiovascular Medicine, Fifth Edition, p. 108, Philadelphia, W.B. Saunders Co.. ISBN 0-7216-5666-8.
- ↑ Ronald M. Birse,rev. Patricia E. Knowlden Oxford Dictionary of National Biography 2004 (Subscription required) – (original source is his biography written by his wife – Elizabeth Muirhead. Alexandernn Muirhead 1848–1920. Oxford, Blackwell: privately printed 1926.)
- ↑ Waller AD (1887). "A demonstration on man of electromotive changes accompanying the heart's beat". J Physiol (Lond). 8 (5): 229–34. PMC 1485094
 . PMID 16991463.
. PMID 16991463. - ↑ Rivera-Ruiz M, Cajavilca C, Varon J (29 September 1927). "Einthoven's String Galvanometer: The First Electrocardiograph". Texas Heart Institute journal / from the Texas Heart Institute of St. Luke's Episcopal Hospital, Texas Children's Hospital. 35 (2): 174–8. PMC 2435435
 . PMID 18612490.
. PMID 18612490. - ↑ Interwoven W (1901). "Un nouveau galvanometre". Arch Neerl Sc Ex Nat. 6: 625.
- 1 2 3 Hurst JW (3 November 1998). "Naming of the Waves in the ECG, With a Brief Account of Their Genesis". Circulation. 98 (18): 1937–42. PMID 9799216. doi:10.1161/01.CIR.98.18.1937.
- ↑ Cooper JK (1986). "Electrocardiography 100 years ago. Origins, pioneers, and contributors". N Engl J Med. 315 (7): 461–4. PMID 3526152. doi:10.1056/NEJM198608143150721.
- ↑ "Dr. Taro Takemi". 27 August 2012.
- ↑ Mark, Jonathan B. (1998). Atlas of cardiovascular monitoring. New York: Churchill Livingstone. ISBN 0-443-08891-8.
- 1 2 3 4 5 Masters, Jo; Bowden, Carole; Martin, Carole (2003). Textbook of veterinary medical nursing. Oxford: Butterworth-Heinemann. p. 244. ISBN 0-7506-5171-7.
- ↑ Moyer VA (2 October 2012). "Screening for coronary heart disease with electrocardiography: U.S. Preventive Services Task Force recommendation statement.". Annals of Internal Medicine. 157 (7): 512–8. PMID 22847227. doi:10.7326/0003-4819-157-7-201210020-00514.
- ↑ Consumer Reports; American Academy of Family Physicians; ABIM Foundation (April 2012), "EKGs and exercise stress tests: When you need them for heart disease — and when you don't" (PDF), Choosing Wisely, Consumer Reports, retrieved 14 August 2012
- ↑ "Summary of Medical Standards" (PDF). U.S. Federal Aviation Administration. 2006. Retrieved 27 December 2013.
- ↑ "Mitigation Strategies for ECG Design Challenges" (PDF). Analog Devices. Retrieved 24 April 2016.
- ↑ RESTING 12-LEAD ECG ELECTRODE PLACEMENT AND ASSOCIATED PROBLEMS.DrTanzil
- ↑ "Electrocardiogram Leads". CV Physiology. 26 March 2007. Retrieved 2009-08-15.
- ↑ "12-Lead ECG Placement Guide with Illustrations". Cables and Sensors. Retrieved 11 July 2017.
- ↑ Kavuru, Madhav S.; Vesselle, Hubert; Thomas, Cecil W. (1987). "Advances in Body Surface Potential Mapping (BSPM) Instrumentation". Pediatric and Fundamental Electrocardiography. Developments in Cardiovascular Medicine. 56: 315–327. ISBN 978-1-4612-9428-3. ISSN 0166-9842. doi:10.1007/978-1-4613-2323-5_15.
- ↑ "Lead Placement". Univ. of Maryland School of Medicine Emergency Medicine Interest Group. Archived from the original on 20 July 2011. Retrieved 15 August 2009.
- ↑ "Limb Leads – ECG Lead Placement – Normal Function of the Heart – Cardiology Teaching Package – Practice Learning – Division of Nursing – The University of Nottingham". Nottingham.ac.uk. Retrieved 15 August 2009.
- ↑ "Lesson 1: The Standard 12 Lead ECG". Library.med.utah.edu. Archived from the original on 22 March 2009. Retrieved 15 August 2009.
- ↑ "Electrocardiogram explanation image". Retrieved 28 February 2014.
- ↑ Meigas, K; Kaik, J; Anier, A (2008). "Device and methods for performing transesophageal stimulation at reduced pacing current threshold". Estonian Journal of Engineering. 57 (2): 154. doi:10.3176/eng.2008.2.05.
- 1 2 Pehrson, Steen M.; Blomströ-LUNDQVIST, Carina; Ljungströ, Erik; Blomströ, Per (1994). "Clinical value of transesophageal atrial stimulation and recording in patients with arrhythmia-related symptoms or documented supraventricular tachycardia-correlation to clinical history and invasive studies". Clinical Cardiology. 17 (10): 528–534. PMID 8001299. doi:10.1002/clc.4960171004.
- ↑ Surawicz, Borys; Knillans, Timothy (2008). Chou's electrocardiography in clinical practice : adult and pediatric (6th ed.). Philadelphia, PA: Saunders/Elsevier. p. 12. ISBN 1416037748.
- ↑ Otero J, Lenihan DJ. "The "normothermic" Osborn wave induced by severe hypercalcemia". Tex Heart Inst J. 27: 316–7. PMC 101092
 . PMID 11093425.
. PMID 11093425. - ↑ Houghton, Andrew R; Gray,D avid (2012). Making Sense of the ECG, Third Edition. Hodder Education. p. 214. ISBN 978-1-4441-6654-5.
- ↑ Alpert JS, Thygesen K, Antman E, Bassand JP (2000). "Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction". J Am Coll Cardiol. 36 (3): 959–69. PMID 10987628. doi:10.1016/S0735-1097(00)00804-4.
- ↑ Segura-Sampedro, Juan José; Parra-López, Loreto; Sampedro-Abascal, Consuelo; Muñoz-Rodríguez, Juan Carlos (2015). "Atrial flutter EKG can be useless without the proper electrophysiological basis". International Journal of Cardiology. 179: 68–9. PMID 25464416. doi:10.1016/j.ijcard.2014.10.076.
- 1 2 Takla, George; Petre, John H.; Doyle, D John; Horibe, Mayumi; Gopakumaran, Bala (2006). "The Problem of Artifacts in Patient Monitor Data During Surgery: A Clinical and Methodological Review". Anesthesia & Analgesia. 103 (5): 1196–1204. doi:10.1213/01.ane.0000247964.47706.5d.
- ↑ Kligfield, Paul; Gettes, Leonard S.; Bailey, James J.; Childers, Rory; Deal, Barbara J.; Hancock, E. William; van Herpen, Gerard; Kors, Jan A.; Macfarlane, Peter (2007-03-13). "Recommendations for the standardization and interpretation of the electrocardiogram: part I: The electrocardiogram and its technology: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology". Circulation. 115 (10): 1306–1324. PMID 17322457. doi:10.1161/CIRCULATIONAHA.106.180200.
- ↑ "northstarcpr.com".
- ↑ Jafary, Fahim H (2007). "The "incidental" episode of ventricular fibrillation: A case report". Journal of Medical Case Reports. 1: 72. PMC 2000884
 . PMID 17760955. doi:10.1186/1752-1947-1-72.
. PMID 17760955. doi:10.1186/1752-1947-1-72. - ↑ Mangalmurti, Sandeep; Seabury, Seth A.; Chandra, Amitabh; Lakdawalla, Darius; Oetgen, William J.; Jena, Anupam B. (2014). "Medical professional liability risk among US cardiologists". American Heart Journal. 167 (5): 690–6. PMC 4153384
 . PMID 24766979. doi:10.1016/j.ahj.2014.02.007.
. PMID 24766979. doi:10.1016/j.ahj.2014.02.007.
- ↑ Incorrect electrode cable connection during electrocardiographic recording (2007) Velislav N. Batchvarov, Marek Malik, A. John Camm, Europace, Oct 2007
- ↑ Chanarin, N., Caplin, J., & Peacock, A. (1990). "Pseudo reinfarction": a consequence of electrocardiogram lead transposition following myocardial infarction. Clinical cardiology, 13(9), 668–669.
- ↑ Guijarro-Morales A., Gil-Extremera B., Maldonado-Martín A. (1991). "ECG diagnostic errors due to improper connection of the right arm and leg cables". International Journal of Cardiology. 30 (2): 233–235. doi:10.1016/0167-5273(91)90103-v.
External links
| Wikimedia Commons has media related to ECG. |
- The whole ECG course on 1 A4 paper from ECGpedia, a wiki encyclopedia for a course on interpretation of ECG
- Wave Maven – a large database of practice ECG questions provided by Beth Israel Deaconess Medical Center
- PysioBank – a free scientific database with physiologic signals (here ecg)
- EKG Academy – free EKG lectures, drills and quizzes