Ewing's sarcoma
| Ewing sarcoma | |
|---|---|
 | |
| Micrograph of metastatic Ewing sarcoma (right of image) in normal lung (left of image). PAS stain. | |
| Classification and external resources | |
| Specialty | Oncology |
| ICD-10 | C41.9 |
| ICD-9-CM | 170.9 |
| ICD-O | M9260/3 |
| OMIM | 612219 |
| DiseasesDB | 4604 |
| MedlinePlus | 001302 |
| eMedicine | ped/2589 |
| MeSH | D012512 |
Ewing's sarcoma or Ewing sarcoma (/ˈjuːɪŋ/) is a malignant small, round, blue cell tumor. It is a rare disease in which cancer cells are found in the bone or in soft tissue. The most common areas in which it occurs are the pelvis, the femur, the humerus, the ribs and clavicle (collar bone).
Since a common genetic locus is responsible for a large percentage of Ewing's sarcoma and primitive neuroectodermal tumors, these are sometimes grouped together in a category known as the Ewing family of tumors.[1]
Ewing's sarcoma occurs most frequently in teenagers and young adults, with a male/female ratio of 1.6:1.[2]
Although usually classified as a bone tumor, Ewing's sarcoma can have characteristics of both mesodermal and ectodermal origin, making it difficult to classify.[3]
James Ewing (1866–1943) first described the tumour, establishing that the disease was separate from lymphoma and other types of cancer known at that time.[4][5]
Presentation
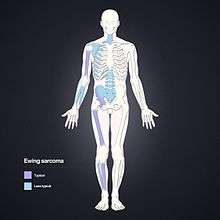
Ewing's sarcoma is more common in males (1.6 male:1 female) and usually presents in childhood or early adulthood, with a peak between 10 and 20 years of age. It can occur anywhere in the body, but most commonly in the pelvis and proximal long tubular bones, especially around the growth plates. The diaphyses of the femur are the most common sites, followed by the tibia and the humerus. Thirty percent are overtly metastatic at presentation. Patients usually experience extreme bone pain.
Signs and symptoms include: intermittent fevers, anemia, leukocytosis, increased sedimentation rate, and other symptoms of inflammatory systemic illness.[6] Also, depending on the type, progression, and location of the tumor - great pain may occur.
According to the Bone Cancer Research Trust (BCRT), the most common symptoms are: localized pain, swelling, and sporadic bone pain with variable intensity. The swelling is most likely to be visible if the sarcoma is located on a bone near the surface of the body, but when it occurs in other places deeper in the body, like on the pelvis, it may not be visible.[7]
Causes
Genetic exchange between chromosomes can cause cells to become cancerous. Most cases of Ewing's sarcoma (85%) are the result of a translocation between chromosomes 11 and 22, which fuses the EWS gene of chromosome 22 to the FLI1 gene of chromosome 11.[6]
EWS/FLI functions as the master regulator.[8]Other translocations are at t(21;22)[9] and t(7;22).[10]Ewing's sarcoma cells are positive for CD99 and MIC2,[6] and negative for CD45.[11]
Diagnosis
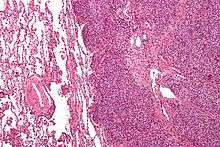
The definitive diagnosis is based on histomorphologic findings, immunohistochemistry and molecular pathology.
Ewing's sarcoma is a small-blue-round-cell tumor that typically has a clear cytoplasm on H&E staining, due to glycogen. The presence of the glycogen can be demonstrated with positive PAS staining and negative PAS diastase staining. The characteristic immunostain is CD99, which diffusely marks the cell membrane. Morphologic and immunohistochemical findings are corroborated with an associated chromosomal translocation, of which several occur. The most common translocation, present in about 90% of Ewing sarcoma cases, is t(11;22)(q24;q12),[12][13] which generates an aberrant transcription factor through fusion of the EWSR1 gene with the FLI1 gene.[14]
The pathologic differential diagnosis is the grouping of small-blue-round-cell tumors, which includes lymphoma, alveolar rhabdomyosarcoma, and desmoplastic small round cell tumor, among others.
Differential diagnosis
Other entities with similar clinical presentations include osteomyelitis, osteosarcoma (especially telangiectatic osteosarcoma), and eosinophilic granuloma. Soft-tissue neoplasms such as pleomorphic undifferentiated sarcoma (malignant fibrous histiocytoma) that erode into adjacent bone may also have a similar appearance.
Imaging findings


On conventional radiographs, the most common osseous presentation is a permeative lytic lesion with periosteal reaction. The classic description of lamellated or "onion-skin" type periosteal reaction is often associated with this lesion. Plain films add valuable information in the initial evaluation or screening. The wide zone of transition (e.g. permeative) is the most useful plain film characteristic in differentiation of benign versus aggressive or malignant lytic lesions.
Magnetic resonance imaging (MRI) should be routinely used in the work-up of malignant tumors. It will show the full bony and soft tissue extent and relate the tumor to other nearby anatomic structures (e.g. vessels). Gadolinium contrast is not necessary as it does not give additional information over noncontrast studies, though some current researchers argue that dynamic, contrast-enhanced MRI may help determine the amount of necrosis within the tumor, thus help in determining response to treatment prior to surgery.
Computed axial tomography(CT) can also be used to define the extraosseous extent of the tumor, especially in the skull, spine, ribs, and pelvis. Both CT and MRI can be used to follow response to radiation and/or chemotherapy. Bone scintigraphy can also be used to follow tumor response to therapy.
In the group of malignant small round cell tumors which include Ewing's sarcoma, bone lymphoma, and small cell osteosarcoma, the cortex may appear almost normal radiographically, while permeative growth occurs throughout the Haversian channels. These tumours may be accompanied by a large soft-tissue mass while almost no bone destruction is visible. The radiographs frequently do not shown any signs of cortical destruction.
Radiographically, Ewing's sarcoma presents as "moth-eaten" destructive radiolucencies of the medulla and erosion of the cortex with expansion.
Treatment
Almost all patients require multidrug chemotherapy (often including ifosfamide and etoposide),[15] as well as local disease control with surgery and/or radiation.[16] An aggressive approach is necessary because almost all patients with apparently localized disease at the time of diagnosis actually have asymptomatic metastatic disease.
Treatment often consists of neoadjuvant chemotherapy, which may include vincristine, doxorubicin, and cyclophosphamide with ifosfamide and etoposide.[6] After about three months of chemotherapy, the remaining tumor is surgically resected, irradiated, or both.[6] The surgical resection may involve limb salvage or amputation. Complete excision at the time of biopsy may be performed if malignancy is confirmed at the time it is examined.
Treatment lengths vary depending on location and stage of the disease at diagnosis. Radical chemotherapy may be as short as six treatments at 3-week cycles, but most patients undergo chemotherapy for 6–12 months and radiation therapy for 5–8 weeks. Radiotherapy has been used for localized disease. The tumor has a unique property of being highly sensitive to radiation, sometimes acknowledged by the phrase "melting like snow", but the main drawback is that it recurs dramatically after some time. Antisense oligodeoxynucleotides have been proposed as possible treatment by down-regulating the expression of the oncogenic fusion protein associated with the development of Ewing's sarcoma resulting from the EWS-ETS gene translocation.[17][18] In addition, the synthetic retinoid derivative fenretinide (4-hydroxy(phenyl)retinamide) has been reported to induce high levels of cell death in Ewing's sarcoma cell lines in vitro and to delay growth of xenografts in in vivo mouse models.[19][20]
Fertility preservation
In women, chemotherapy may damage the ovaries and cause infertility. To avail future pregnancies, the woman may preserve oocytes or ovarian tissue by oocyte cryopreservation or ovarian tissue cryopreservation prior to starting chemotherapy. However, the latter may reseed the cancer upon reinsertion of the ovarian tissue.[21] If it is performed, the ovarian tissue should be examined for traces of malignancy at both the pathological and molecular levels prior to the grafting of the cryopreserved tissue.[21]
Prognosis
Staging attempts to distinguish patients with localized from those with metastatic disease.[22] Most commonly, metastases occur in the chest, bone and/or bone marrow. Less common sites include the central nervous system and lymph nodes.
Five-year survival for localized disease is 70% to 80% when treated with chemotherapy.[23] Prior to the use of multi-drug chemotherapy, long-term survival was less than 10%. The development of multi-disciplinary therapy with chemotherapy, irradiation, and surgery has increased current long-term survival rates in most clinical centers to greater than 50%.[1] However, some sources state it is 25–30%.[24]
Retrospective research in patients led by Idriss M. Bennani-Baiti (Cancer Epigenetics Society) showed that two chemokine receptors, CXCR4 and CXCR7, can be used as molecular prognosis factors. Patients who express low levels of both chemokine receptors have the highest odds of long-term survival with >90% survival at 5 years post-diagnosis versus <30% survival at 5 years for patients with very high expression levels of both receptors.[25]
Epidemiology
Ewing's sarcomas represent 16% of primary bone sarcomas.[6] In the United States, they are most common in the second decade of life,[6] with a rate of 0.3 cases per million in children under 3 years of age, and as high as 4.6 cases per million in adolescents aged 15–19 years. Internationally, the annual incidence rate averages less than 2 cases per million children.[26] In the United Kingdom, an average of six children per year are diagnosed, mainly males in early stages of puberty. Due to the prevalence of diagnosis during teenage years, a link may exist between the onset of puberty and the early stages of this disease, although no research confirms this hypothesis.
The oldest known patient diagnosed was at age 76, from the Mercer County, New Jersey, area.
A grouping of three unrelated teenagers in Wake Forest, NC, have been diagnosed with Ewing's sarcoma. All three children were diagnosed in 2011 and all attended the same temporary classroom together while the school underwent renovation. A fourth teenager living nearby was diagnosed in 2009. The odds of this grouping are considered significant.[27]
Ewing's sarcoma shows striking differences in incidence across human populations and is about 10- to 20-fold more common in populations from European descent as compared to Africans.[28] Consistently, a genome-wide association study (GWAS) conducted in several hundreds European individuals with Ewing's sarcoma and genetically-matched healthy controls identified three susceptibility loci located on chromosomes 1, 10 and 15.[29] A continuative study discovered that the Ewing's sarcoma susceptibility gene EGR2, which is located within the chromosome 10 susceptibility locus, is regulated by the EWSR1-FLI1 fusion oncogene via a GGAA-microsatellite.[30][31]
Ewing sarcoma is the second most common bone cancer in children and adolescents, with poor prognosis and outcome in ~70% of initial diagnoses and 10–15% of relapses.[32]
Research, information and support
In the UK and Ireland, the Bone Cancer Research Trust funds research and provides information on Ewing's sarcoma and other bone cancers. This includes information for teenagers who have this condition.
Melatonin, a natural molecule without relevant side effects, has been previously shown to induce cytotoxicity in SK-N-MC cells, a Ewing sarcoma cell line.[33]
See also
References
- 1 2 Iwamoto Y (February 2007). "Diagnosis and treatment of Ewing's sarcoma". Jpn. J. Clin. Oncol. 37 (2): 79–89. PMID 17272319. doi:10.1093/jjco/hyl142.
- ↑ Burt M, Karpeh M, Ukoha O, et al. (January 1993). "Medical tumours of the chest wall. Solitary plasmacytoma and Ewing's sarcoma". J. Thorac. Cardiovasc. Surg. 105 (1): 89–96. PMID 8419714. Archived from the original on 2013-04-14.
- ↑ Longtin R (November 2003). "Ewing sarcoma: a miracle drug waiting to happen?". J. Natl. Cancer Inst. 95 (21): 1574–6. PMID 14600088. doi:10.1093/jnci/95.21.1574.
- ↑ synd/2367 at Who Named It?
- ↑ Ewing, J. (1921). "Diffuse endothelioma of bone". Proceedings of the New York Pathological Society. 21: 17–24.
- 1 2 3 4 5 6 7 medicine, s cecil. Goldman (24th ed.). Philadelphia: Elsevier Saunders. p. 1326. ISBN 978-1-4377-2788-3.
- ↑ "Symptoms of Ewing's Sarcoma - Bone Cancer Research Trust". Bcrt.org.uk. Archived from the original on 2013-01-30. Retrieved 2012-11-05.
- ↑ Owen LA, Kowalewski AA, Lessnick SL (2008). Wu, Xiaolin, ed. "EWS/FLI mediates transcriptional repression via NKX2.2 during oncogenic transformation in Ewing's sarcoma". PLoS ONE. 3 (4): e1965. PMC 2291578
 . PMID 18414662. doi:10.1371/journal.pone.0001965.
. PMID 18414662. doi:10.1371/journal.pone.0001965. - ↑ Sorensen PH, Lessnick SL, Lopez-Terrada D, Liu XF, Triche TJ, Denny CT (February 1994). "A second Ewing's sarcoma translocation, t(21;22), fuses the EWS gene to another ETS-family transcription factor, ERG". Nat. Genet. 6 (2): 146–51. PMID 8162068. doi:10.1038/ng0294-146.
- ↑ Jeon IS, Davis JN, Braun BS, et al. (March 1995). "A variant Ewing's sarcoma translocation (7;22) fuses the EWS gene to the ETS gene ETV1". Oncogene. 10 (6): 1229–34. PMID 7700648.
- ↑ Bernstein M, Kovar H, Paulussen M, et al. (May 2006). "Ewing sarcoma family of tumours: current management". Oncologist. 11 (5): 503–19. PMID 16720851. doi:10.1634/theoncologist.11-5-503.
- ↑ "Soft tissue tumors: Ewing's tumors/Primitive neurectodermal tumors (PNET)". Atlas of Genetics and Cytogenetics in Oncology and Haematology. Archived from the original on 29 October 2012. Retrieved 5 November 2012.
- ↑ Turc-Carel C, Aurias A, Mugneret F, et al. (June 1988). "Chromosomes in Ewing's sarcoma. I. An evaluation of 85 cases of remarkable consistency of t(11;22)(q24;q12)". Cancer Genet. Cytogenet. 32 (2): 229–38. PMID 3163261. doi:10.1016/0165-4608(88)90285-3.
- ↑ Delattre, Olivier; Zucman, Jessica; Plougastel, Béatrice; Desmaze, Chantal; Melot, Thomas; Peter, Martine; Kovar, Heinrich; Joubert, Isabelle; de Jong, Pieter (1992-09-10). "Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours". Nature. 359 (6391): 162–165. PMID 1522903. doi:10.1038/359162a0.
- ↑ Lahl M, Fisher VL, Laschinger K (February 2008). "Ewing sarcoma family of tumours: an overview from diagnosis to survivorship". Clin J Oncol Nurs. 12 (1): 89–97. PMID 18258578. doi:10.1188/08.CJON.89-97. Archived from the original on 2013-01-28.
- ↑ Randall, RL (2005). "Ewing's Sarcoma Family of Tumours (ESFT)". ESUN. Retrieved 2009-04-15.
- ↑ Asami S, Chin M, Shichino H, et al. (March 2008). "Treatment of Ewing sarcoma using an antisense oligodeoxynucleotide to regulate the cell cycle". Biol. Pharm. Bull. 31 (3): 391–4. PMID 18310898. doi:10.1248/bpb.31.391. Archived from the original (– Scholar search) on 2012-12-19.
- ↑ Mateo-Lozano S, Gokhale PC, Soldatenkov VA, Dritschilo A, Tirado OM, Notario V (November 2006). "Combined transcriptional and translational targeting of EWS/FLI-1 in Ewing sarcoma". Clin. Cancer Res. 12 (22): 6781–90. PMID 17121899. doi:10.1158/1078-0432.CCR-06-0609.
- ↑ Myatt SS, Redfern CP, Burchill SA (April 2005). "p38MAPK-Dependent sensitivity of Ewing's sarcoma family of tumors to fenretinide-induced cell death". Clin. Cancer Res. 11 (8): 3136–48. PMID 15837770. doi:10.1158/1078-0432.CCR-04-2050.
- ↑ Myatt SS, Burchill SA (February 2008). "The sensitivity of the Ewing's sarcoma family of tumours to fenretinide-induced cell death is increased by EWS-Fli1-dependent modulation of p38(MAPK) activity". Oncogene. 27 (7): 985–96. PMID 17700534. doi:10.1038/sj.onc.1210705.
- 1 2 Abir R, Feinmesser M, Yaniv I, et al. (May 2010). "Occasional involvement of the ovary in Ewing sarcoma". Hum Reprod. 25 (7): 1708–12. PMID 20472912. doi:10.1093/humrep/deq121.
- ↑ McTiernan AM, Cassoni AM, Driver D, Michelagnoli MP, Kilby AM, Whelan JS (2006). "Improving Outcomes After Relapse in Ewing Sarcoma: Analysis of 114 Patients From a Single Institution". Sarcoma. 2006: 83548. PMC 1698143
 . PMID 17496997. doi:10.1155/SRCM/2006/83548.
. PMID 17496997. doi:10.1155/SRCM/2006/83548. - ↑ "ACS :: How Is the Ewing Family of Tumors Staged?". Archived from the original on 2008-04-22.
- ↑ Thacker, MM; Temple, HT; Scully, SP (2005). "Current treatment for Ewing's sarcoma". Expert review of anticancer therapy. 5 (2): 319–31. PMID 15877528. doi:10.1586/14737140.5.2.319.
- ↑ Bennani-Baiti IM; et al. (2010). "Intercohort gene expression co-analysis reveals chemokine receptors as prognostic indicators in Ewing's sarcoma". Clinical Cancer Research. 16 (14): 3769–3778. PMC 2905506
 . PMID 20525755. doi:10.1158/1078-0432.CCR-10-0558.
. PMID 20525755. doi:10.1158/1078-0432.CCR-10-0558. - ↑ Ewing Sarcoma Imaging at eMedicine
- ↑ WRAL (29 April 2013). "Three Wake students battle rare cancer: Cluster or coincidence? :: WRAL.com".
- ↑ Worch, Jennifer; Cyrus, Jobin; Goldsby, Robert; Matthay, Katherine K.; Neuhaus, John; DuBois, Steven G. (2011-03-01). "Racial Differences in the Incidence of Mesenchymal Tumors Associated with EWSR1 Translocation". Cancer Epidemiology Biomarkers & Prevention. 20 (3): 449–453. ISSN 1055-9965. PMC 3051020
 . PMID 21212061. doi:10.1158/1055-9965.EPI-10-1170.
. PMID 21212061. doi:10.1158/1055-9965.EPI-10-1170. - ↑ Postel-Vinay, Sophie; Véron, Amélie S; Tirode, Franck; Pierron, Gaelle; Reynaud, Stéphanie; Kovar, Heinrich; Oberlin, Odile; Lapouble, Eve; Ballet, Stelly. "Common variants near TARDBP and EGR2 are associated with susceptibility to Ewing sarcoma". Nature Genetics. 44 (3): 323–327. PMID 22327514. doi:10.1038/ng.1085.
- ↑ Grünewald, Thomas G P; Bernard, Virginie; Gilardi-Hebenstreit, Pascale; Raynal, Virginie; Surdez, Didier; Aynaud, Marie-Ming; Mirabeau, Olivier; Cidre-Aranaz, Florencia; Tirode, Franck. "Chimeric EWSR1-FLI1 regulates the Ewing sarcoma susceptibility gene EGR2 via a GGAA microsatellite". Nature Genetics. 47 (9): 1073–1078. PMC 4591073
 . PMID 26214589. doi:10.1038/ng.3363.
. PMID 26214589. doi:10.1038/ng.3363. - ↑ Gomez, Nicholas C; Davis, Ian J. "Linking germline and somatic variation in Ewing sarcoma". Nature Genetics. 47 (9): 964–965. PMID 26313223. doi:10.1038/ng.3387.
- ↑ Twardziok Monika; et al. (2016). "Multiple Active Compounds From Viscum Album L. Synergistically Converge To Promote Apoptosis In Ewing Sarcoma". PLOS ONE. 11 (9): 1–18. doi:10.1371/journal.pone.0159749.
- ↑ Casado-Zapico, Sara, et al. "Synergistic Antitumor Effect Of Melatonin With Several Chemotherapeutic Drugs On Human Ewing Sarcoma Cancer Cells: Potentiation Of The Extrinsic Apoptotic Pathway." Journal Of Pineal Research 48.1 (2010): 72-80. Academic Search Premier. Web. 5 Nov. 2016.
- Bone Tumors - Differential diagnosis. Henk Jan van der Woude and Robin Smithuis.Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital,Leiderdorp,the Netherlands.
External links
- Cancer.Net: Ewing Family of Tumors, Childhood
- Ewing family of tumors entry in the public domain NCI Dictionary of Cancer Terms
- OrthoTumours a case-based educational resource