Epidermis
| Epidermis | |
|---|---|
|
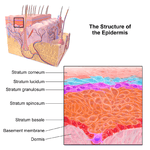
Histologic image of epidermis, delimited by white bar. | |
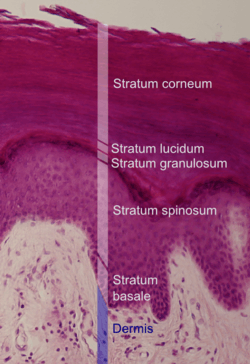 Histologic image detailing epidermal layers. Stratum corneum appears more compact in this image than above because of different sample preparation. | |
| Details | |
| Identifiers | |
| Latin | Epidermis |
| Code | TH H3.12.00.1.01001 |
| TA | A16.0.00.009 |
| FMA | 70596 |
The epidermis is the outer (ἐπί epi in Greek meaning "over" or "upon") of the two layers that make up the skin (or cutis; Greek δέρμα derma), the inner layer being the dermis.[1] This skin layer provides a barrier to infection from environmental pathogens[2] and regulates the amount of water released from the body into the atmosphere through transepidermal water loss (TEWL).[3]
The outermost part of the epidermis is composed of stratified layers of flattened cells,[4] that overlies a basal layer (stratum basale) composed of columnar cells arranged perpendicularly.
The rows of cells develop from the stem cells in the basal layer. ENaCs are found to be expressed in all layers of the epidermis.[5]
Structure
Cellular components
The epidermis has no blood supply and is nourished almost exclusively by diffused oxygen from the surrounding air.[6] It is 95% keratinocytes[4] (proliferating basal and differentiated suprabasal) but also contains melanocytes, Langerhans cells, Merkel cells,[1] and inflammatory cells. Rete ridges (or rete pegs) are epidermal thickenings that extend downward between dermal papillae.[7] Blood capillaries are found beneath the epidermis, and are linked to an arteriole and a venule.
Cell junctions
In the epidermis, the cells are tightly interconnected to serve as a tight barrier. The junctions between the epidermal cells is adherens junction type. These junctions are formed by transmembrane proteins called cadherins. Inside the cell, the cadherins are linked to actin filaments. In immunofluorescence microscopy, the actin filament network appears as a thick border surrounding the cells[5]. Yet, as noted, the actin filaments are located inside the cell and run parallel to the cell membrane. Because of the proximity of the neighboring cells and tightness of the junctions, the actin immunofluorescence appears as a border between cells.[5]
Layers

The epidermis is composed of 4 or 5 layers depending on the region of skin being considered.[8] Those layers in descending order are:[2]

- Composed of 10 to 30 layers of polyhedral, anucleated corneocytes (final step of keratinocyte differentiation), with the palms and soles having the most layers. Corneocytes are surrounded by a protein envelope (cornified envelope proteins), filled with water-retaining keratin proteins, attached together through corneodesmosomes and surrounded in the extracellular space by stacked layers of lipids.[9] Most of the barrier functions of the epidermis localize to this layer.[10]
- clear/translucent layer (stratum lucidum, only in palms and soles)
- The skin found in the palms and soles is known as "thick skin" because it has 5 epidermal layers instead of 4.
- granular layer (stratum granulosum)

- Keratinocytes lose their nuclei and their cytoplasm appears granular. Lipids, contained into those keratinocytes within lamellar bodies, are released into the extracellular space through exocytosis to form a lipid barrier. Those polar lipids are then converted into non-polar lipids and arranged parallel to the cell surface. For example glycosphingolipids become ceramides and phospholipids become free fatty acids.[9]
- spinous layer (stratum spinosum)

- Keratinocytes become connected through desmosomes and start produce lamellar bodies, from within the Golgi, enriched in polar lipids, glycosphingolipids, free sterols, phospholipids and catabolic enzymes.[3] Langerhans cells, immunologically active cells, are located in the middle of this layer.[9]
- basal/germinal layer (stratum basale/germinativum).

- Composed mainly of proliferating and non-proliferating keratinocytes, attached to the basement membrane by hemidesmosomes. Melanocytes are present, connected to numerous keratinocytes in this and other strata through dendrites. Merkel cells are also found in the stratum basale with large numbers in touch-sensitive sites such as the fingertips and lips. They are closely associated with cutaneous nerves and seem to be involved in light touch sensation.[9]
The Malpighian layer (stratum malpighi) is both the stratum basale and stratum spinosum.[4]
The epidermis is separated from the dermis, its underlying tissue, by a basement membrane.
Cellular kinetics
Cell division
The stratified squamous epithelium is maintained by cell division within the stratum basale. Differentiating cell delaminate from the basement membrane and are displaced outwards through the epidermal layers, undergoing multiple stages of differentiation until, in the stratum corneum, losing their nucleus and fusing to squamous sheets, which are eventually shed from the surface (desquamation). Differentiated keratinocytes secrete keratin proteins which contribute to the formation of an extracellular matrix and is an integral part of the skin barrier function. In normal skin, the rate of keratinocyte production equals the rate of loss,[4] taking about two weeks for a cell to journey from the stratum basale to the top of the stratum granulosum, and an additional four weeks to cross the stratum corneum.[2] The entire epidermis is replaced by new cell growth over a period of about 48 days.[11]
Calcium concentration
Keratinocyte differentiation throughout the epidermis is in part mediated by a calcium gradient, increasing from the stratum basale until the outer stratum granulosum, where it reaches its maximum, and decreasing in the stratum corneum. Calcium concentration in the stratum corneum is very low in part because those relatively dry cells are not able to dissolve the ions. This calcium gradient parallels keratinocyte differentiation and as such is considered a key regulator in the formation of the epidermal layers.[3]
Elevation of extracellular calcium concentrations induces an increase in intracellular free calcium concentrations.[12] Part of that intracellular increase comes from calcium released from intracellular stores[13] and another part comes from transmembrane calcium influx,[14] through both calcium-sensitive chloride channels[15] and voltage-independent cation channels permeable to calcium.[16] Moreover, it has been suggested that an extracellular calcium-sensing receptor (CaSR) also contributes to the rise in intracellular calcium concentration.[17]
Development
Epidermal organogenesis, the formation of the epidermis, begins in the cells covering the embryo after neurulation, the formation of the central nervous system. In most vertebrates, this original one-layered structure quickly transforms into a two-layered tissue; a temporary outer layer, the periderm, which is disposed once the inner basal layer or stratum germinativum has formed.[18]
This inner layer is a germinal epithelium that give rise to all epidermal cells. It divides to form the outer spinous layer (stratum spinosum). The cells of these two layers, together called the Malpighian layer(s) after Marcello Malpighi, divide to form the superficial granular layer (Stratum granulosum) of the epidermis.[18]
The cells in the stratum granulosum do not divide, but instead form skin cells called keratinocytes from the granules of keratin. These skin cells finally become the cornified layer (stratum corneum), the outermost epidermal layer, where the cells become flattened sacks with their nuclei located at one end of the cell. After birth these outermost cells are replaced by new cells from the stratum granulosum and throughout life they are shed at a rate of 0.001 - 0.003 ounces of skin flakes every hour, or 0.024-0.072 ounces per day.[19]
Epidermal development is a product of several growth factors, two of which are:[18]
- Transforming growth factor Alpha (TGFα) is an autocrine growth factor by which basal cells stimulate their own division.
- Keratinocyte growth factor (KGF or FGF7) is a paracrine growth factor produced by the underlying dermal fibroblasts in which the proliferation of basal cells is regulated.
Function
Barrier
The epidermis serves as a barrier to protect the body against microbial pathogens, oxidant stress (UV light) and chemical compounds and provides mechanical resistance. Most of that function is played by the stratum corneum.[10]
Characteristics of the barrier
- Physical barrier through keratinocytes attached together via cell–cell junctions and associated to cytoskeletal proteins, which gives the epidermis its mechanical strength.[3]
- Chemical barrier through the presence of highly organized lipids, acids, hydrolytic enzymes and antimicrobial peptides.[3]
- Immunologically active barrier through humoral and cellular constituents of the immune system.[3]
- Water content of the stratum corneum drops towards the surface, creating hostile conditions for pathogenic microorganism growth.[10]
- An acidic pH (around 5.0) and low amounts of water make it hostile to many microorganic pathogens.[10]
- The presence of non-pathogenic microorganism on the epidermis surface help defend against pathogenic one by limiting food availability and through chemical secretions.[10]
Factors that alter the barrier
- Psychological stress, through an increase in glucocorticoids, compromises the stratum corneum and thus the barrier function.[20]
- Sudden and large shifts in humidity alter stratum corneum hydration in a way that could allow entry of pathogenic microorganisms.[21]
Skin hydration
The ability of the skin to hold water is primarily due to the stratum corneum and is critical for maintaining healthy skin.[22] Lipids arranged through a gradient and in an organized manner between the cells of the stratum corneum form a barrier to transepidermal water loss.[23][24]
Skin color
The amount and distribution of melanin pigment in the epidermis is the main reason for variation in skin color in Homo sapiens. Melanin is found in the small melanosomes, particles formed in melanocytes from where they are transferred to the surrounding keratinocytes. The size, number, and arrangement of the melanosomes varies between racial groups, but while the number of melanocytes can vary between different body regions, their numbers remain the same in individual body regions in all human beings. In white and Asian skin the melanosomes are packed in "aggregates", but in black skin they are larger and distributed more evenly. The number of melanosomes in the keratinocytes increases with UV radiation exposure, while their distribution remain largely unaffected.[25]
Clinical significance
Laboratory culture of keratinocytes to form a 3D structure (artificial skin) recapitulating most of the properties of the epidermis is routinely used as a tool for drug development and testing.
Additional images
|
See also
References
- 1 2 James, William; Berger, Timothy; Elston, Dirk (2005) Andrews' Diseases of the Skin: Clinical Dermatology (10th ed.). Saunders. pp. 2–3. ISBN 0-7216-2921-0.
- 1 2 3 Marks, James G; Miller, Jeffery (2006). Lookingbill and Marks' Principles of Dermatology (4th ed.). Elsevier. pp. 1–7. ISBN 1-4160-3185-5.
- 1 2 3 4 5 6 Proksch, E.; Brandner, J.; Jensen, J.M. (2008). "The skin: an indispensable barrier". Experimental Dermatology. 17 (12): 1063–1072. PMID 19043850. doi:10.1111/j.1600-0625.2008.00786.x.
- 1 2 3 4 McGrath, J.A.; Eady, R.A.; Pope, F.M. (2004). Rook's Textbook of Dermatology (7th ed.). Blackwell Publishing. pp. 3.1–3.6. ISBN 978-0-632-06429-8.
- 1 2 3 Hanukoglu I, Boggula VR, Vaknine H, Sharma S, Kleyman T, Hanukoglu A (January 2017). "Expression of epithelial sodium channel (ENaC) and CFTR in the human epidermis and epidermal appendages". Histochemistry and Cell Biology. 147 (6): 733–748. PMID 28130590. doi:10.1007/s00418-016-1535-3.
- ↑ Stücker, M; Struk, A; Altmeyer, P; Herde, M; Baumgärtl, H; Lübbers, DW (2002). "The cutaneous uptake of atmospheric oxygen contributes significantly to the oxygen supply of human dermis and epidermis". The Journal of Physiology. 538 (3): 985–994. PMC 2290093
 . PMID 11826181. doi:10.1113/jphysiol.2001.013067.
. PMID 11826181. doi:10.1113/jphysiol.2001.013067. - ↑ TheFreeDictionary > rete ridge Citing: The American Heritage Medical Dictionary Copyright 2007, 2004
- ↑ The Ageing Skin - Structure
- 1 2 3 4 http://www.radcliffe-oxford.com/books/samplechapter/7750/01_bensouillah-241a6c80rdz.pdf
- 1 2 3 4 5 Elias, P.M. (2007). "The skin barrier as an innate immune element". Seminars in Immunopathology. 29 (1): 3–14. PMID 17621950. doi:10.1007/s00281-007-0060-9.
- ↑ Iizuka, Hajime (1994). "Epidermal turnover time". Journal of Dermatological Science. 8 (3): 215–217. PMID 7865480. doi:10.1016/0923-1811(94)90057-4.
- ↑ Hennings, H; Kruszewski, FH; Yuspa, SH; Tucker, RW (1989). "Intracellular calcium alterations in response to increased external calcium in normal and neoplastic keratinocytes". Carcinogenesis. 10 (4): 777–80. PMID 2702726. doi:10.1093/carcin/10.4.777.
- ↑ Pillai, S; Bikle, DD (1991). "Role of intracellular-free calcium in the cornified envelope formation of keratinocytes: Differences in the mode of action of extracellular calcium and 1,25 dihydroxyvitamin D3". Journal of cellular physiology. 146 (1): 94–100. PMID 1990023. doi:10.1002/jcp.1041460113.
- ↑ Reiss, M; Lipsey, LR; Zhou, ZL (1991). "Extracellular calcium-dependent regulation of transmembrane calcium fluxes in murine keratinocytes". Journal of cellular physiology. 147 (2): 281–91. PMID 1645742. doi:10.1002/jcp.1041470213.
- ↑ Mauro, TM; Pappone, PA; Isseroff, RR (1990). "Extracellular calcium affects the membrane currents of cultured human keratinocytes". Journal of cellular physiology. 143 (1): 13–20. PMID 1690740. doi:10.1002/jcp.1041430103.
- ↑ Mauro, TM; Isseroff, RR; Lasarow, R; Pappone, PA (1993). "Ion channels are linked to differentiation in keratinocytes". The Journal of membrane biology. 132 (3): 201–9. PMID 7684087. doi:10.1007/BF00235738.
- ↑ Tu, CL; Oda, Y; Bikle, DD (1999). "Effects of a calcium receptor activator on the cellular response to calcium in human keratinocytes". The Journal of Investigative Dermatology. 113 (3): 340–5. PMID 10469331. doi:10.1046/j.1523-1747.1999.00698.x.
- 1 2 3 Gilbert, Scott F (2000). "The Epidermis and the Origin of Cutaneous Structures". Developmental Biology. Sinauer Associates. ISBN 0-87893-243-7.
- ↑ Weschler, Charles J. (April 8, 2011). "Squalene and Cholesterol in Dust from Danish Homes and Daycare Centers". Environ. Sci. Technol. 45: 3872–3879. PMID 21476540. doi:10.1021/es103894r. Retrieved 3 July 2014.
- ↑ Denda, M.; Tsuchiya, T.; Elias, P.M.; Feingold, K.R. (2000). "Stress alters cutaneous permeability barrier homeostasis". Am J Physiol Regul Integr Comp Physiol. 278 (2): R367–372. PMID 10666137.
- ↑ http://onlinelibrary.wiley.com/doi/10.1021/js950219p/abstract
- ↑ Blank, IH (1952). "Factors which influence the water content of the stratum corneum". The Journal of Investigative Dermatology. 18 (6): 433–40. PMID 14938659. doi:10.1038/jid.1952.52.
- ↑ Downing, DT; Stewart, ME; Wertz, PW; Colton, SW; Abraham, W; Strauss, JS (1987). "Skin lipids: An update". The Journal of Investigative Dermatology. 88 (3 Suppl): 2s–6s. PMID 2950180. doi:10.1111/1523-1747.ep12468850.
- ↑ Bonté, F; Saunois, A; Pinguet, P; Meybeck, A (1997). "Existence of a lipid gradient in the upper stratum corneum and its possible biological significance". Archives of dermatological research. 289 (2): 78–82. PMID 9049040. doi:10.1007/s004030050158.
- ↑ Montagna, William; Prota, Giuseppe; Kenney, John A. (1993). Black skin: structure and function. Gulf Professional Publishing. p. 69. ISBN 0-12-505260-X.