Blasio Vincent Ndale Esau Oriedo
| Dr. Blasio Vincent Oriedo | |
|---|---|
|
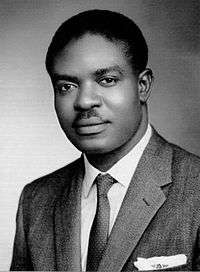
Blasio Vincent Oriedo circa 1962 | |
| Born |
15 September 1931 Ebwali Village, Bunyore, Kenya Colony |
| Died |
26 January 1966 (aged 34) Aga Khan University Hospital, Nairobi, Kenya |
| Cause of death | Inexplicable |
| Nationality | Kenyan |
| Citizenship | Kenyan |
| Education | Doctor of Medical Science in Public Health (DrPH) |
| Occupation | Epidemiologist, parasitologist, physician, author, hygienist, medical research scientist |
| Years active | 1948 –1966 |
| Known for |
Contribution to tropical medicine and public health; saved tens of thousands of aboriginal African lives by stemming a myriad of disease epidemics in colonial and postcolonial Kenya, the east and central African region, and the Sudan; and for medical research in the epidemiology of east African leishmaniasis. |
| Relatives |
Esau Khamati Oriedo (father), Dr. J. Vincent B. Oriedo (son) |
| Medical career | |
| Profession | Epidemiologist, parasitologist, physician, author, hygienist, medical research scientist |
| Field | Tropical medicine, public health, vector-borne epidemiological medical science |
| Institutions |
Ministry of Health and Housing, Kenya Medical Research Division of Insect-Borne Diseases, Kenya Colony Colonial Medical Services Medical Department of Kenya Colony East African High Commission’s Bureau of Research in Medicine and Hygiene |
| Specialism | Leishmaniasis (kala-azar) |
| Research | Tropical diseases |
| Notable works |
Tropical diseases: 1952 Kala-azar (black fever) or visceral leishmaniasis epidemic; 1954 enteric/typhoid fever epidemic; 1960 Kwashiorkor epidemic; and 1950s/1960s plasmodium falciparum malaria epidemics |
| Notable prizes | Tripartite laureate fellow; NIH Extramural (Medical) Researcher; Special Achievement and Contribution to Public Health—The East African Bureau of Research in Medicine and Hygiene;The Dutch Royal Institute fellow; Bukusu “Omukasa” |
Dr. Blasio Vincent Oriedo, in full Dr. Blasio Vincent Ndale Esau Oriedo (born September 15, 1931, Ebwali Village in Bunyore, Kenya Colony—died January 26, 1966, Aga Khan University Hospital, Nairobi, Kenya) was a distinguished pioneering African epidemiologist and a parasitological scientist known for his contributions to tropical medicine and stemming a myriad of disease epidemics in the colonial era and embryonic postcolonial Kenya, and in the countries of the East and Central African region, and the Sudan.[1][2][3][4][5][6][7] He is especially credited for singlehandedly saving tens of thousands of native African lives from decimation due to an array of infectious diseases. His death in the springtime of life at age 34 was precipitously inexplicable, and has remained so to this day. Dr. Oriedo was a tripartite laureate; and a recipient of the coveted Extramural Medical Research Grant presented by the National Institute of Health (NIH), United States of America (U.S.A.). What is more, he was an academician, author, a linguist, and an East African statesman of his day. He was a close confidante of Thomas Joseph Odhiambo Mboya (d. 1969); and served as a member of Tom Mboya’s interdisciplinary economic development advisory team from 1965 till his death in January 1966.[8][9][10][11] As a patron of the academics and intellectual infrastructures in East Africa, he is one of the unheralded silent forces behind the concept and impetus of the late 1950s - 1960s American academic scholarships for East African students; popularly dubbed the Mboya-Kennedy “Airlift to America” program.[12][13] Moreover, he was renowned for his innate acumen to engender abidingly comprehensive polygonal interpersonal relationships with such international luminaries as Sir Philip Edmund Clinton Manson-Bahr (d. 1966) with whom he was close friends; and Dr. Apollo Milton Obote (d. 2005) twice president (1966–71, 1980–85) of Uganda.
He was born to the venerable Esau Khamati Oriedo (d. 1 December 1992) and Evangeline Olukhanya Ohana Analo-Oriedo (d. 11 July 1982), both from the western Kenya’s Luhya ethnic group of the Bantu lineage. His father was a renowned Kenyan statesman (freedom fighter and colonial era political detainee, district representative and once chairman of the North Nyanza Local Native Council[14]), an entrepreneur, philanthropist, and a veteran of two world wars—WW I and II, and a Christian who doggedly challenged the early white Christian missionaries in East Africa to embrace the African cultures as congruent with the Christian credo.[15][16] His mother was a staunch advocate of women’s rights and literacy in Kenya. Albeit a closeness with his mother, the relationship with his father was estranged. Thus, his formative years were spent with a paternal uncle, Bernard Walter Amukhale Oriedo.
He received early education at government and mission schools, and sat, successfully with Distinction, for Cambridge School Certificate in 1946 at the former Government African School at Kakamega in North Nyanza (present day Kakamega High School at Kakamega in western Kenya).[17][18][19][Notes 1] He attended the prestigious Royal Institute of Medicine & Public Health at Nairobi; graduating in 1950. He was a Licentiate of the Royal College of Physicians and Surgeons of Great Britain. He attained DPH postgraduate education in epidemiological tropical medicine in Europe at the London School of Hygiene & Tropical Medicine a constituent college of the University of London; and was a fellow at the Dutch Royal Tropical Institute foundation in The Netherlands, and the Tulane University's Medical College's School of Tropical and Infectious Diseases at New Orleans in United States. He attended and contributed to a myriad of scientific conferences and proceedings, lectures, and speaking engagements in East and Central Africa, Sudan, North America, Australia, Oceania, India, Hong Kong, and South Africa.
He was the first and the youngest native East and Central African epidemiologist in the field of tropical medicine and infectious diseases—both as researcher and a clinical practitioner in the spread, control, and eradication of infectious agents. His pioneering parasitological epidemiology medical research and resultant modalities have received global acclaim and application.[20] He was a key champion of indigenous medical research and the dissemination of homegrown scientific medical information—such as, new clinical modalities, field studies and discoveries, etc.—via cooperation with indigenous and overseas scholarly reviewed publications, medical panels, and scientific proceedings. He foresaw this informational approach as an effective and dynamic forum for interchange of knowledge and viewpoints amongst various indigenous healthcare communities and their counterparts abroad; a mechanism for the documentation and dissemination of vital information on local diseases within the East and Central African region. His epidemiological medical research of the East African leishmaniasis or kala-azar (black fever) has bred critical knowledge for worldwide use in both private and public health sectors, and civil societies.[21][22][23][24][25][26][27][28] In 1964 he attended, as an invited expert panelist, the XII International Congress of Entomology at London, United Kingdom.[29]
He was a cogent cognizant of health care as a basic human right long before the 1978 Alma Ata Declaration proclamation.[30] This cognizance is evident in his intrepid and transformative role in East Africa’s healthcare, socioeconomic, sociocultural, and intellectual infrastructures. In 1960 he directed a healthcare and hygiene strategy of tactical, strategic, operational, and performance indexing; a short-term and long-term planning strategy based on the application of preventative modalities that helped shift the medical science paradigm—in East Africa—away from the undue emphasis on curative means, and more so towards a balanced approach. That which effectually integrated strategic epidemiological knowledge with tactical, operational, and situational curative approaches.[31][32][Notes 2] In the course of his tenure the region witnessed markedly sustained improvement in schoolchildren’s health and hygiene, public health (stemming of major disease epidemics and better sanitary conditions), and seamless integration of interdisciplinary and interagency resourcing. A tenure accredited with a maximization of key quality metrics and improvement in performance outcomes.
He promoted and nurtured coordinated approaches, amongst healthcare practitioners and related bodies, to facilitate the most effective seamlessly integrated dispensary and operations of public health and other civic and societal welfare services. As of 1950 until his abrupt and inexplicable death in 1966, he is credited with stemming the tide of numerous endemic and pandemic diseases in the East and Central African regions and the Sudan; and a forfending of entire indigenous populations from imminent extinction. The following are examples of those striking feats.[8][33]
In October 1952, the young BV Oriedo’s skills were put to the test when he was tasked to lead efforts to stem a major epidemic outbreak of a deadly parasitic Kala-azar (black fever) or visceral leishmaniasis disease in Kenya, and parts of Uganda. The epidemic had also manifested itself in the Sudan. Coming to the fore personally, he took a practical approach and relocated himself to the remote hinterland outpost District Hospital and Public Health Office at Kitui in South Eastern Kenya; the region hardest hit by the epidemic. He devised a savvy strategy to stem the tide of the epidemic, and saved thousands of indigenous lives. In 1954 the disease was arrested.
In 1954 he spearheaded a successful government campaign to stem typhoid epidemic in present-day Kenya and Uganda. The North Kavirondo region of Mt. Elgon in Kenya—the Bungoma realm (presently Bungoma County in the former Western Province of Kenya) was one of hardest hit areas. The disease was wreaking havoc amidst the ethnic Bukusu population; threatening to decimate the ethnic group. He employed his charisma (to build effective stakeholder partnership and respective rapports with local native elders and traditional entities), vigilant statesmanship, and technical acumen to effectually stem the epidemic and save the local population from imminent decimation.
In 1960 the colonial authorities tasked him with formulating a roadmap to guide and coordinate an interterritorial, interdisciplinary and interagency crisis-management team to deal with kwashiorkor crisis—a disease with high mortality-rates among infants and children. He successfully focused on the Kikuyu ethnic group, one of the localities where the disease was endemic. The lessons learnt from the Kikuyu campaign gave impetus to an effective regional strategy.
In 1959 he spearheaded an intensified malaria eradication campaign in the East African highlands that helped to reduce malaria epidemics in the region.
In 1964 he was a recipient of a coveted medical research grant furnished by the United States National Institutes of Health (NIH), Extramural Research Program. He was a laureate and a tripartite fellow at the London School of Hygiene & Tropical Medicine, the Dutch Royal Institute, and Tulane University's Medical College's School of Public Health and Tropical Medicine.
A confidante of Tom Mboya, he allied with Mboya to successfully champion American education opportunities for East African Students. In the late 1950s (and thereafter) he was a silent force behind the fostering of indispensable rapports with likeminded contemporaries abroad that led to the inception of higher education opportunities in North America for talented East African students.[12]
He was an ardent patron of academics, healthcare, and socioeconomic development in East Africa. While fighting disease epidemics across the region he’d witnessed the abysmal conditions of the civil and other key infrastructures in large the segments of the country, which had led him to explicate that excessive emphasis was being placed on the political fulcrum at the detriment of critical socioeconomic, healthcare, and intellectual infrastructure rudiments.[34] This experience caused him to direct his skills and influence, ardently, crusading for the latter, while engaging peripherally in the former. As a matter of fact, he was but a handful of native Africans to approach the pursuit of “political” independence with an infallible apprehensive optimism. He favored blending the liberation movement with a creation of a robust and dynamic intellectual infrastructure capable of bringing into being an adequate cadre of erudite native professionals needed to sustain a practicably independent Kenyan state. Consequently, he declined a career in politics, despite being incessantly lobbied by his associates to do so, among them Tom Mboya; who were all in all au courant with his intuitively charismatic oratory, articulacy, and situational leadership skills, coupled with his acumen for local and international affairs and geopolitics which were congruent with the needs of the liberation movement in Kenya, and the wider East Africa.[Notes 3][35][36] Afterwards, he served, at Tom Mboya’s behest, as a member of Mboya’s multidisciplinary economic development team from 1965 till his death in January 1966.[37]
He was a staunch adversary of maladroitness and the abuse of public trust; utterly stubborn—an uncompromising scrupulous—and demonstrative disdain for and impatient towards ineptitude. He was an outspoken critic of vice by those in power; thus, his policies became anathema to the vestiges of colonial Kenya, and most postcolonial bureaucrats and political elites of the embryonic independent Kenya. Proof positive, in 1965, upon his return from a conference in the Netherlands and other official engagement in Europe, he summarily terminated employment of several expatriates and native personnel for graft, ineptitude, and absconding from duty.[38] His actions albeit justifiably de jure met with ad hominem assails from a cadre of bureaucrats and political elites; nevertheless, he stood his ground and refused to be intimidated into rescinding the edicts. In his point of view these individuals’ embrace of public service was solely a means to an end; such that theirs was a dichotomous embodiment of a pernicious approach to public interest.[34]
He was a fluent speaker and writer of English, Dutch, Kiswahili, Luganda, Luhya, Dholuo, Kamba, and Kikuyu languages.
Consonant with his fêted cerebral abilities, he was a trendsetter and socialite who boasted a charismatic persona, splendid nobility; a prescient interlocutor with a quick wit to boot. A cadre of multidisciplinary and racially diverse (Africans, Indo-Asiatics, Caucasians, Arabs, etc.) contemporaries from across East Africa flocked to his residence to indulge in social intercourse—interchange of ideals and ideas, entertainment, debate local and international affairs and geopolitics du jour. He was known to his contemporaries as “Jaraha”—a hybrid Kiswahili-Dhuluo idiom for “en vogue socialite” or the “cosmopolitan”! His pals encompassed such international luminaries as Tom Mboya (d. 1969)—with whom they were confidantes; Sir Philip Edmund Clinton Manson-Bahr (d. 1966)—the son-in-law of Sir Patrick Mason, the doyen founder of the field of tropical medicine; Dr. Apollo Milton Obote—led Uganda to independence from Britain in 1962, becoming Prime Minister and the President twice; Prof. Hillary Ojiambo; Masinde Muliro; Charles Njonjo; Kitili Maluki Mwendwa; Elijah Wasike Mwangale; Paul Ngei; Fred Kubai; Achieng Oneko; Joseph Otiende; Dr Julius Gikonyo Kiano; Argwings Kodhek; Dr. B. A. Southgate[39]—British Colonial Medical office, London; Dr. R. Bowen;[39] and Dr. R. B. Heisch;[39] to name but a few. Dr. BV Oriedo was a sprightly romantic and charming figure with an Achilles' heel for comely studious women. His chivalrous gregariousness and joviality persona enamored women and is replete with tales of broken hearts; a trait that was an absolute bête noire to his mother, an ardent crusader of women rights in Kenya.
Biography
Early life
Dr. BV Oriedo was born to Esau Khamati Oriedo (d. 01 December 1992) and Evangeline Olukhanya Ohana Analo-Oriedo (d. 11 July 1982), both from the western Kenya’s Luhya tribe of Africa’s Bantu lineage. His mother was a homemaker, a domestic economics educator, and an ardent advocate of women rights. Whereas, his father was a consummate Kenyan statesman, politician (1910s – 1960s), and an anti-colonialism activist and freedom fighter who had been detained, 1952-1956, alongside Paramount Chief Koinange and Jomo Kenyatta (the first President of the Republic of Kenya), and a cadre of other anti-colonialists during the campaign for Kenya’s independence from the British rule. Esau Oriedo was also an entrepreneur and trade unionist, a staunch crusader of Christianity’s embrace of indigenous African cultures,[15] philanthropist, and a veteran of World War I and World War II as a soldier in the King's African Rifles (KAR) regiment of the British Army. Albeit enjoying a close relationship with his mother, the relationship with his father was estranged. He ran away from home as a child. His formative years were spent with his paternal uncle, Bernard Walter Amukhale Oriedo, who helped raise him. It has been argued that his uncle played an influencing role in Dr. BV Oriedo’s decision to actualize a healthcare vocation even though his father had wanted him to pursue a business and political careers.
Early and Higher Education
He received early education at government and mission schools, and sat, successfully with distinction, for Cambridge School Certificate in 1946 at the former Government African School at Kakamega in North Nyanza (present day Kakamega High School at Kakamega in western Kenya).[18][Notes 1] He attended the prestigious Royal Institute of Medicine & Public Health (RIMPH), an elite conjoined Government College at Kabete in suburban Nairobi, Kenya which catered to cerebrally gifted scholars in East and Central Africa; where he pursued an interdisciplinary degree in medicine—with focus on public health, hygiene, and disease prevention medicine program. During his tenure of study at the Royal Institute of Medicine & Public Health, he secured an internship as a staff researcher assistant with the Division of Insect-Borne Diseases at Medical Research Laboratory, Nairobi. In 1950 he completed his college education at the RIMPH, graduating with high honours. In the same year of his college graduation he successfully completed the board certification exams, administered from London in Great Britain; he became a Licentiate of the Royal College of Physicians of London. The certification and licensure qualified him for a job classification of a senior public health officer — a rank exclusively earmarked for Briton or Caucasian medical expatriates possessing Great Britain medical degrees or analogous European qualifications. Moreover, his qualifications exceeded the requirements for employment by the Colonial Medical Service — the organization responsible for dispensation of healthcare services and policy initiatives in the British Overseas Territories.[40][41][42] Instead, he was appointed to an inferior position as an African assistant medical officer (AAMO).[43] He remonstratively rebuffed the appointment; in 1951 he was actualized as a senior public health officer with de jure commission which permitted him to serve across the East and Central African region. He also qualified for assignments under the auspices of the Colonial Medical Service.[40][44][ In 1954 he received academic fellowship to study tropical medicine & parasitological epidemiology[44] in the United Kingdom at the London School of Hygiene & Tropical Medicine. His research thesis was on the vector-borne tropical diseases; it focused on the epidemiology of East African leishmaniasis (kala-azar), and attained a DPH. In 1957 he was a recipient of an associate research scientist fellowship from Tulane University's Medical College's School of Public Health and Tropical Medicine at New Orleans in United States—he continued, fruitfully, to collaborate his work in East Africa with Tulane University until his precipitously inexplicable death in January 1966.[45] He was also a recipient of a research stipend awarded by the Dutch Royal Institute in the Netherlands; the institute actively promoted his research on the “vector-borne tropical diseases: epidemiology of East African leishmaniasis (kala-azar)” in the Netherlands and other European countries. He worked feverishly, with diligent acumen, effectively combining vocational duties and scholarship research with travel abroad to various international scholarly medical conferences and special proceedings to promote awareness of the tropical diseases in Africa; and to help stimulate funding for research and drug discovery to stem epidemics and other preventable diseases on the continent. An epic accomplishment for an under 30-year old native African at the apogee of European colonialism in East Africa! In 1959 he gained full membership to The Royal Society of Tropical Medicine and Hygiene—a London-based organization promoting the study, control and prevention of tropical disease, and facilitation of discussion and exchange of information among those interested in tropical diseases and international health, and the overall promotion of the work of those interested in these objectives. In 1962, through his collaborative research with Tulane University’s Medical College’s School of Tropical and Infectious Diseases, he was endowed with a prestigious extramural medical research grant from the NIH—an agency of the United States Department of Health and Human Services.[44][46]
Professional Life
Throughout his career he was tenured at the Ministry of Health and Housing, Nairobi, Kenya, and the Nairobi based Division of Insect-Borne Diseases at Medical Research Laboratory under the auspices of the British Colonial Medical Services.[31][40] The inception of his epidemiological vocation dates to 1950 after he attained a diploma in public health and preventive medicine (DPH)from the Royal Institute of Medicine & Public Health. At that same period, at the age nineteen, he became the youngest native person in the East and Central African region to autonomously engage in active interdisciplinary medical research in epidemiology and parasitology.[46] After an efficacious completion of a London (Britain) administered board certification exams and licensure, he was actualized in 1951 to the rank of a senior (principal) public health officer under the auspices of the Ministry of Health and Housing, Nairobi, Kenya. Thus, becoming the first and the only native person, du jour, to hold such commission across the British East Africa Colony and Protectorate.[32] He was later to become the first native East African epidemiologist in the field of tropical medicine and infectious diseases. He served as an epidemiologist in dual capacity under the aegis of the Colonial Medical Services[8][40][47] and the Ministry of Health and Housing in the colonial and post-colonial Kenya. His consummate and pioneering parasitological epidemiology and medical research, and epidemiological mapping of pestilences and preventive modalities in the field of tropical medicine and insect-borne infectious diseases in East and Central African have received global acclaim and application. Antecedently, his interdisciplinary medical acumen; dedication to public service; selflessness; and ability to connect with local African villagers helped stem disease-epidemic outbreaks and save thousands of native lives; and to improve the quality of living across the East and Central African region and the Sudan. Mournfully, historiography focuses on either the European doctors or the non-white subordinates of the various African Colonial Medical Services, whereas non-white personnel, such as Dr. BV Oriedo who worked contemporaneously in higher status positions, have received very little attention or no acknowledgement.[48][Notes 4]
In 1950 he was selected to led a handful of medical students from Kenya to attend the Conference of the World Health Organization on Malaria at Kampala, Uganda.
Albeit tenured both at the Nairobi based Division of Insect-Borne Diseases at Medical Research Laboratory[Notes 6], and the Ministry of Health and Housing during and post-colonial British rule, he shunned the city comforts du jour in the interest of serving the aboriginal populations of the African Great Lakes region, going to the fore personally. He spent most of his time in disease ravaged remote villages, meticulously implementing curative and preventative measures; recording observations and mapping out diseases, authoring and disseminating reports.[Notes 5]
His cerebral abilities and immense potential in the field of tropical medicine and infectious vector-borne diseases was, beforehand, recognized by Sir Philip Edmund Clinton Manson-Bahr, MD, (d. November 1966) of the British Colonial Medical Services and renowned for his contributions to tropical medicine; and the son-in-law of Sir Patrick Mason, the doyen founder of the field of tropical medicine. Sir Manson-Bahr enlisted the young researcher to assist in his work on tropical medicine and infectious diseases in East African[21]; and later, elsewhere within the British Empire, largely under the auspices of the Colonial Medical Service—the personnel section of the Colonial Service, employing the healthcare professionals who tended to the health of both the colonial staff and the local populations of the British Empire.
In 1951 Sir Manson-Bahr invited him to attend the “Conference of Specialists on infectious tropical diseases: Filariasis in the South Pacific”, held at Papeete, Tahiti, August - September, 1951; which Sir Manson-Bahr was a principle organizer and interlocutor. Filariasis[Notes 6] was increasingly of concern in the colonial East Africa du jour.
The two men would subsequently foster a close friendship and collaboration in the field of infectious diseases and tropical medicine. Moreover, Sir Manson-Bahr in conjunction with the British Colonial Medical Services and the East African Bureau of Research in Medicine and Hygiene (East Africa High Commission) featured markedly in the meritorious efforts that earnt him a 1954 research fellowship to study tropical medicine & parasitological epidemiology in the United Kingdom at the London School of Hygiene & Tropical Medicine.
In 1964 he was an invited panel of specialist at the XII International Congress of Entomology at London, United Kingdom.[29]
Campaign Against Infectious Disease Epidemics
He promoted and nurtured coordinated approaches, amongst healthcare practitioners and related bodies, to facilitate the most effective seamlessly integrated dispensary and operations of healthcare, socioeconomic, and other social welfare services. He was presciently cognizant of the adverse socioeconomic, sociocultural, and socioecological consequences of disease or injury on individuals, communities and civil infrastructures, or organizations. He effectively synergized with all key stakeholders, in a robust and dynamic interdisciplinary bilateral or multilateral partnership, via a wholesome stakeholder-engagement whose desired key outcome were to formulate and implement disease prevention initiatives that were evidence-based, and both practicable and transformative, tailored towards the target-population, and outcome-driven. These initiatives were performance indexed— vis-à-vis, delivering measurable performance.
As of 1950 until his abrupt and inexplicable death in 1966, he is credited with stemming the tide of numerous endemic and pandemic diseases in the East and Central African regions and the Sudan; and a forfending of thousands of human lives. In 1959 he spearheaded an intensified malaria eradication campaign in the East African highlands that helped to reduce malaria epidemics in the region.[49][50][51][52][53][54]
Kala-azar (black fever) or visceral leishmaniasis epidemic
In October 1952 the young BV Oriedo’s skills were put to the test when he was tasked to lead efforts to stem a major epidemic outbreak of black fever disease in Kenya, and parts of Uganda.[32][33] The epidemic had also manifested itself in the Sudan. Kala-azar (black fever) or visceral leishmaniasis is a deadly parasitic disease endemic to the tropics, subtropics, and southern Europe. He took a hands-on approach relocated himself to the remote hinterland outpost District Hospital and Public Health Office at Kitui in Kenya; the region hard-hit by the epidemic. He devised a savvy strategy to stem the tide of the epidemic, and saved thousands of lives. In 1954 the disease was arrested.[21][Notes 7]
Enteric or Typhoid fever epidemic
In 1954 he spearheaded a successful government campaign to stem typhoid epidemic in present-day Kenya and Uganda.[55] Once more his expertise was needed by the colonial administration in Kenya and the British Colonial Medical Services in London, to spearhead efforts to stem a major epidemic outbreak of another disease, typhoid or enteric fever—a fatal multisystemic disease. The North Kavirondo region of Mt. Elgon in Kenya—the Bungoma realm (presently Bungoma County in the former Western Province of Kenya) was one of hardest hit areas. The disease was wreaking havoc amidst the ethnic Bukusu population; threatening to decimate the ethnic group. Yet again, he employed his charisma, vigilant statesmanship, and technical functional acumen to effectually stem the epidemic and save the local population from imminent decimation. His achievement was recognized accordingly among the Bukusu people who denoted him a great leader and healer by officially crowning him with an honorary title of “omukasa”—a paramount Bukusu chieftain.
By leveraging from his notably efficacious Bukusu strategy he made it possible to swiftly stem the disease and save lives in Kenya and Uganda, and other East African regions. This feat of accomplishment earned him a research stipend by the London School of Hygiene & Tropical Medicine at London, United Kingdom.
The Fight Against Kwashiorkor— a protein deficiency disease
In the 1940s kwashiorkor was an ill-defined and one of the widespread nutritional disorders in East Africa and other regions of the African continent.[56][57] The mortality-rates especially among infants and children were disturbingly high. In 1960, based on his prior successful campaigns against epidemic disease outbreaks, the colonial authorities tasked him with formulating a roadmap to guide and coordinate the interdisciplinary and interagency crisis-management team to deal with kwashiorkor crisis. Using available data, he unpretentiously focused on the Kikuyu ethnic group, one of the localities where the disease was endemic. Yet again, the Kikuyu campaign was utterly successful. The lessons learnt from the Kikuyu campaign gave impetus to an effective regional strategy. One of the key elements of the program was the national school milk program which provided daily provision of milk to kindergarten through preparatory school children during morning and afternoon recess sessions; moreover, educators were mandated to somatically check pupils for health and hygiene during physical education (PE) periods; further, schools were duty-bound to maintain up-to-date requisite immunization records. Indeed, this was one of the constituents of a multi-part dynamic public health strategy—which had been explicitly adapted by the East African Commission—toward health wellness; thus, socioeconomic, sociocultural, and socioecological progressions in the region.[Notes 8]
Plasmodium falciparum malaria epidemics campaign
During the late 1950s and 1960s (prior to his inexplicable death in 1966) he championed, coordinated, and buoyed the campaign against malaria amongst Africans and Asiatics communities in East Africa where the disease epidemics was poignantly endemic and had exacted a heavy mortality toll. Those communities, especially the native African tribes were mostly remote and in disadvantaged settings. Preceding his efforts, those communities had received, at best, spasmodic attention from the colonial regime.[32][50][50][51][53][54][58] For instance, the 1961 heavy rainfall brought flooding and the rise of the outbreaks of malaria epidemics that extended deeply into the hinterland. He was a major force behind the resourcefulness in formulating and implementing an extensive public health control program; elements of the program entailed leveraging-in successful aspects from the Nairobi campaign of 1940 epidemic, scouting and mapping out the breeding sites, conducting entomological and epidemiological studies, oiling and larviciding of stagnant waters and bushes, and mass chemoprophylaxis administration.[32][52][54][59] The approach succeeded in containing malaria epidemics in several remote and disadvantaged settings amongst Africans and Asiatics communities.[Notes 9][60][61]
Situational, tactical, operational, and strategical national health system
He was an unbendable crusader of an important performance indexed healthcare quality improvement program[Notes 10][32] which raised immunization coverage levels of inoculation preventable diseases by lessening missed opportunities to vaccinate, vigilant administration of accountability requirements, and the overall improved standards of practices for health wellness and fitness, at all levels, in the Eastern Africa region. In 1960 he was one of the key architects of a dynamical interdisciplinary multicomponent and multigenerational public health, a healthcare and hygiene, strategy of long-term planning based on the application of preventative modalities that helped shift the medical science paradigm—in East Africa—away from the undue emphasis on curative means, and more so towards a balanced approach; that which seeks to adapt public health strategies that effectively integrates epidemiological, parasitological, and etiological knowledge with tactical and situational curative approaches.The desired key outcomes included the prevention of disease or infectious agents, disability, malnutrition, and mortality rate—especially among the vulnerable populations of children, youth, and young adults—by means of immunization, hygiene, nutrition (e.g., providing free fluid whole milk for school children as part of his campaign against kwashiorkor epidemic outbreaks), and dietary supplement with multivitamins, and by control of contagious, parasitic and related diseases. The antecedent healthcare and hygiene strategy received the commendation of the British colonial East African High Commission and the British Colonial Medical Services in London; the strategy was adapted by the commission and Kenya’s Ministry of Health and Housing. The program forms the organizational rudiments of the present healthcare and hygiene strategy in East Africa.[62][63][64]
Dr. BV Oriedo, in person, conducted surprise compliance audits across mostly remote regions of Kenya and Uganda—he wrote meticulously cogent observations outlining his findings and recommendations for corrective measures, and a timeline for full compliance. In cases of systemic failures, he was known to summarily discharge the absconding individual(s).
An epidemiological perspective to economic consequences of disease
A frontier statesman and a scientist he developed an interdisciplinarity pioneering approach that connected the struggle for political freedom in Kenya with fully integrated healthcare, intellectual, socioeconomic, and civil infrastructures; especially in the rural regions that bore the brunt of disease epidemics and its dire socioeconomic and sociocultural consequences. Antecedently, he embraced a revolutionary du jour epidemiological perspective towards the economic and intellectual consequences of disease or public health strategy across the East African region. Indeed, he understood that a viable independent Kenya would require not only a cadre of well-educated native professionals but also inevitably a sustainable robust and dynamic local healthcare and intellectual infrastructures able to fuel and drive a sustainable economic development, hence an equitable holistic wellness of all her peoples. To this effect, he ardently lobbied—albeit unsuccessfully—to adapt health care as an expressly stipulated right endowed under the new constitution of the nascent postcolonial Kenya. This prescient interdisciplinary consummate statesmanship made him distinct from the effusive political cadre of his contemporaries that are prominently chronicled with Kenya’s freedom struggle.[34]
Regulating native African ethno-medicinal practices
Throughout his career he sought to regulate, through explication and behavioral modification, the passé pluralistic medicine and mysticism that had remained a central sociocultural institution across East Africa.[65] Antecedently, he was an austere vocal critic of indigenous practices that placed the wellbeing of native communities in peril and easy prey to the quackery of guileful practitioners—he worked towards getting those charlatanism practices extirpated. Moreover, he advocated for regulating native ethno-medicinal practices and outlawing those that were insanitary or insalubrious through erudition programs tailored to specific native communities’ socioculturalism. Congruently, he encouraged a scientific approach to traditional medicinal modalities, vis-à-vis, enacting of quality control criteria such as dosage guidelines in conjunction with promoting proven evidence-based time-tested and outcome-driven ethno-medicine. He presciently cognized that this could only be achieved through colorable scientifically modeled studies to authenticate the safety and efficacies of indigenous healing methods akin to the European or westernized medicine. To accomplish the antecedent initiative, he recommended founding an ethnomedicine advisory board, at the national and provincial levels, under the auspices of the Ministry of Health and Housing; a board whose composition would include traditional healers and modern healthcare practitioners.[46] Regrettably, his precipitously inexplicable death led to the demise of the initiative; as it lacked a natural vigilant and persuasive sponsor of his acumen and stature.
Medical Scientific Research
He was a consummate medical scientific research and an intellectual. He was motivated by a quest for perfectionism, and dedication to his profession and those whom he served; a scholarly and fastidious scientific researcher and medical epidemiological and parasitological practitioner. His research thesis was in the field of tropical medicine’s parasitological epidemiology of infectious diseases or agents. Indeed, he is known for his contributions to tropical medicine via a myriad of practical field campaigns against a range of disease epidemics in East and Central Africa, and the Sudan. His most notable contribution to tropical medicine stems from the studies and fieldwork in the epidemiology of East African leishmaniasis. He amassed aplenty informative medical studies, clinical and field observations data, and his analyses and postulations in the medical disciplines of tropical medicine and hygiene.
Moreover, he embraced the peer review scholarly processes and made full use of it. In the 1950s he called for and helped champion, with the backing of Sir Manson-Bahr and B.A. Southgate, for the creation of an official peer-reviewed comprehensive healthcare reference database for East Africa akin of the U.S. National Library of Medicine. Similarly, he ardently championed for a creation of a robust and dynamic healthcare infrastructure in the rural regions —a “National Reference Health Centre for Kenya”.
In 1953 and ‘54, he was an invited panelist at the East Africa High Commission Scientific Conference. The conference which was under the aegis of the London based Colonial Office of United Kingdom was an exclusive citadel for the European research expatriates. On January 11th, 1961, an abstract of the first series of his pioneering epidemiological medical studies of the East African Leishmaniasis (kala-azar) was presented before the East Africa High Commission Scientific Conference on “The Epidemiology of Arthropod-borne Diseases”, at Nairobi. The work was very well received, and has enjoyed sweeping application and has been widely cited, across the globe.[66][67][67][5][68][69][70][71][72][73][74] A large volume of his work—in the field of Tropical Medicine, Hygiene, and Infectious Diseases (agents)—has been posthumously published by collaborators, such as fellow laureate Dr. BA Southgate, and others.[75][76][77][78][79][80]
He was a panelist at a Rural Health Conference of the South Pacific Commission, Tahiti, April 1963.
All things considered, his achievements are utterly remarkable for two main reasons. Firstly, these epic feats could be attained by one so young and within a very short amount of time—prior to his precipitous death at age 34; secondly, these feats occurred during the epoch of colonialism at which time Africans—especially in professional scientific fields—were relegated to servitude roles and faced perpetual subordination.[Notes 11]
In 1964 he was a recipient of a coveted medical research grant furnished by the United States National Institutes of Health (NIH), Extramural Research Program. The grant was in support of his pioneering epidemiological, parasitological, and etiological research—field and clinical research and development in the spread, control, and eradication of infectious agents—in Tropical Medicine and Infectious Diseases in East Africa. Albeit a life short lived, his pioneering work has received global acclaim and application.[46]
Studies in the Epidemiological and Parasitological of East African Leishmaniasis
His Epidemiological and Parasitological Studies of East Africa Leishmaniasis led to the chivalrous stemming of October, 1952 visceral leishmaniasis epidemic outbreak in Kenya—a British colony du jour. In 1952 he stoically, in a profound demonstration of his commitment to the human cause of the lives of indigenous peoples,(ii) relocated to the remote hinterland outpost District Hospital and Public Health Office at Kitui in Kenya—moving to the fore personally—to spearhead a hands-on crusade against a major kala-azar epidemic outbreak in October, 1952. Kala-azar (black fever) or visceral leishmaniasis is a deadly parasitic disease endemic to the tropics, subtropics, and southern Europe. The disease was first diagnosed in the Kitui region of the British colony of Kenya du jour in 1946.(iii)(iv) The Kitui epidemic was a portentously existential peril to thousands of indigenous lives; it threatened to wipeout entire ethnic Kamba villages. He devised a savvy strategy to stem the tide of the epidemic, and managed to save thousands of lives. In 1954 the disease was arrested.
Albeit the stemming the tide of the Kitui kala-azar epidemic in 1954 and afterwards in other regions of the Kenyan colony, a plethora of epidemiological questions remained unanswered; moreover, the disease was still gnawingly ubiquitous in numerous other regions of East Africa and the Sudan. Thus, with the keen encouragement and support of Sir P. E. C. Manson-Bahr and Dr. B. A. Southgate, a Briton and his research associate and close friend, he proposed a collaborative approach—between himself and Dr. B. A. Southgate, and two other researchers at the Medical Research Laboratory’s Division of Insect-borne Diseases at Nairobi—to perform in-depth medical epidemiological and parasitological studies of visceral leishmaniasis in East and Central Africa, and the Sudan. The collaboration became the impetus of his concurrently synchronous kala-azar epidemiological vocation and dissertational research studies at the London School of Hygiene & Tropical Medicine in the Great Britain. His sponsors and main contributing entities to this novel work were the London School of Hygiene & Tropical Medicine; Sir Philip Henry Manson-Bahr; East African High Commission’s East Africa Bureau of Research in Medicine and Hygiene; the British Colonial Medical Services at London; Ministry of Health and Housing, Kenya; the Division of Insect-borne Diseases, Medical Research Laboratory, Nairobi; and Tulane University's Medical College's School of Tropical and Infectious Diseases in the United States.
His astute epidemiological and parasitological medical research and field observations of visceral leishmaniasis in East and Central Africa, and the Sudan revealed that under ceteris paribus male and female populations exposed to the disease experience different symptoms or sometimes no symptoms; further, the seropositivity rate was higher in females than the males; whereas, using the leishmanin skin test, higher prevalence in males has been recorded. His observations played a major role in the elucidation of the multi-etiological factors in the gestation of the disease; the delineation of which, is of the essence in precluding the misclassification of the induction and latent phases of the disease or infectious agents. Another key elucidation based on his work is that infected people are not needed to maintain the natural transmission cycle of the leishmania protozoan parasite; viz., the natural transmission cycle is sustainable by means of animal reservoir hosts along with sandflies. These findings helped pave the way for a more effective characterization of the incubation process of the disease through a more erudite complex multifarious modern epidemiological and parasitological approaches. This work has been widely cited and the complex multifarious approach widely applied.[24]
Statesmanship
He was quasi-antithetical to donning sumptuous political office; thus, despite incessant lobbying by his fellow countrymen in the political cadre—among them his confidante Tom Mboya—who were au courant with his intuitively superb oratory, articulatory, charisma, and leadership (situational, tactical, and strategic and transformational) skills, coupled with his acuity for local and international geopolitical affairs that were congruent with their perceived needs of Kenya's liberation movement. Albeit a caritas assent for politics per se, he espoused differing strategic considerations and philosophical approaches, vis-à-vis Kenya's liberation initiative; he gave precedence to the activism of healthcare, socioeconomic, and intellectual infrastructure needs of the region. In a communiqué to his confidante Tom Mboya, he cautioned the nascent Kenyan political cadre of the liberation movement against a gullibility towards an impetuous independency—opining that such impetuous move, meagerly developed civil institutions, could lead to vassalage statehood and a vacuous independence, unless wholesome tactical and strategic civil institution infrastructures were in place to remedy the situation at the time of independence. He argued that Africans du jour had yet to achieve sufficient critical-to-success intellectual, healthcare, and socioeconomic resources and infrastructures for a comprehensive wholesome liberation—a truly Africanized self-governance.
Whilst spearheading campaigns against a myriad of disease epidemics and parasitological epidemiology research—in the rustic and urbanite regions across East and Central Africa—he’d come face-to-face with the abominable high rates of poverty among the native populations and the ensuing undue repugnant healthcare and hygiene woes borne by those communities. This shattering firsthand experience led him to explicate that excessive emphasis was being placed on political fulcrum at the detriment of critical socioeconomic, healthcare, and intellectual infrastructural rudiments. This experience caused him to ardently use his skills and influence crusading for the latter, while engaging peripherally in the former. He cognized health care as a basic human right long before the 1978 Alma Ata Declaration proclamation. This cognizance is evident in his intrepid and transformative role in East Africa’s healthcare, socioeconomic, and intellectual infrastructures. His precipitously inexplicable death in the springtime of life at age 34, robbed these causes an ardently eloquent advocate and consummate statesman.
Patron of Academics
Apart from Dr. BV Oriedo’s venerable contribution to the healthcare system in the East and Central Africa region, du jour, he was an indubitable patron of higher education and a boon to the impetus of intellectual infrastructure in the nascent postcolonial East Africa. In the late 1950s (and thereafter) he was a silent force behind the fostering of indispensable rapports with likeminded contemporaries abroad that led to the inception of higher education opportunities in North America for talented East African students. It’s worth noting that during the colonial and embryonic postcolonial East Africa, higher education (college and university) opportunities, both the quality and quantity, were severely inadequate for the native African students. Thus, the antecedent initiative was part of his abiding furtherance of a robustly dynamic intellectual infrastructure in the countries of the eastern and central African region, du jour, via a strategy of multipartite cross-functional partnerships abroad. The higher education initiative (concept of opportunities in North America) resonated very well with his confidante and compatriot, Thomas Joseph Odhiambo "Tom" Mboya (d. July 1969)—a dynamic and compelling political figure in Kenya's liberation movement. The two friends were utterly indispensable in their combined efforts; moreover, they teamed up with other key protagonists, locally and abroad, to champion the program as a key policy initiative. Some of these key partners included John F. Kennedy (a U.S. president, who was then a senator), William X. Scheinman (businessman), Jackie Robinson (former baseball star), Harry Belafonte (singer and actor), and Sidney Poitier (actor); William X. Scheinman is undoubtedly the pillar that buttressed the campaign, and the engine and fuel that sustained the process—a man to whom Kenya owes a great debt.[25] Tom Mboya played a key role in securing air transportation to North America, in September 1959, for the initial eighty-one students with scholarship in the United States and Canada; whereas, Dr. BV Oriedo was an esoteric boon of the concept and the scholarship initiative—including directing and advising Tom Mboya accordingly.[8][26] Thereafter, Mboya would become the dominant political face of this laudable and unquestionably successful initiative.[8] Perhaps the crowning achievement of the initiative was the 1959 founding of the African American Students Foundation (AASF), which further obtained hundreds of new scholarships in North America for students from the East African countries. In addition, the AASF raised funds for airfare and living expenses for the scholarship recipients.[27] Moreover, the AASF, with the facilitation of John F. Kennedy, secured a contribution of $200,000 from Joseph P. Kennedy, Jr. Foundation that entailed the entire amount needed for the 1960-61 academic year airlift, and the assisting of students with basic living expenses in the United States.[28] In this regard, it can be argued that Dr. BV Oriedo is an embodiment of the epic odyssey of Kenya’s (Africa’s) unheralded protagonists. On the other hand, he was a performance-driven pragmatist with a focus on the salient outcome.
Relationships
Dr. BV Oriedo was an accomplished and charismatic figure, who possessed an innate capacity to cultivate an interdisciplinary network of far-reaching and ecumenical professional and proletarian relationships that transcended race, and across geographies. For instance, albeit not having attended Makerere Medical School at Mengo in Uganda, as early as 1950 he enjoyed piquant professional and social kindred with a cadre of Makerere medical community[29]—which consisted of Africans, Indians, Arabs, and whites.
Consonant with his fêted cerebral abilities, he was a trendsetter and socialite. He boasted a charismatic persona, splendid nobility, and clairvoyant interlocution with a quick wit to boot. A cadre of diverse and multidisciplinary contemporaries (Africans, Indo-Asiatics, Caucasians, Arabs, etc.) from across East Africa flocked to his residence to indulge in social intercourse—interchange of ideals and ideas, entertainment, debate local and international affairs and geopolitics du jour. He was known to his contemporaries as “Jaraha”—a hybrid Kiswahili-Dhuluo idiom for “en vogue socialite” or the “cosmopolitan”! His camaraderie was quite encompassing. It included some of the most accomplished scientists, politicians, civil servants, academicians, businessmen/merchants, administrators, and a plethora of common people du jour. The list included such international luminaries as Sir Philip Edmund Clinton Manson-Bahr (d. 1966)—the son-in-law of Sir Patrick Mason, the doyen founder of the field of tropical medicine, Tom Mboya—Cabinet Minister who was also a very close confidante, Professor Hillary Ojiambo—Kenyan Chief Cardiologist & the late President Jomo Kenyatta’s personal physician, Masinde Muliro—Cabinet Minister, Charles Njonjo—Kenyan’s Attorney General during Jomo Kenyatta’ presidency; Kitili Maluki Mwendwa—1st African Chief Justice of Kenya; Dr. BA Southgate—Research Scientist & Medical Physician, Paul Ngei—Cabinet Minister; Dr. Apollo Milton Obote—led Uganda to independence from Britain in 1962, becoming Prime Minister and the President twice; Fred Kubai—Cabinet Minister, Achieng Oneko—Cabinet Minister; Andrew Omanga Cabinet Minister; Joseph Otiende—Cabinet Minister; Elijah Mwangale—Cabinet Minister; Dr. Julius Gikonyo Kiano—Cabinet Minister; Dr. R. Bowen; Dr. RB Heisch; Dr. James O. W. Ang'awa; Dr. Nelson Awori (the first East African to perform a kidney transplant); Argwings Kodhek (Kenya’s first African degreed lawyer); etc.
Professional Memberships
- The Royal Society of Tropical Medicine and Hygiene — London-based organization promoting the study, control and prevention of tropical diseases
- The Dutch Royal Tropical Institute (KIT) — a foundation located in Amsterdam, The Netherlands
- The Royal Sanitary Institute, The U.K. — Sanitary Inspectors Association, Public Health
- Specialist Officer Staff Member—The East African High Commission’s Bureau of Research in Medicine and Hygiene
- East African Standing Advisory Committee for Medical Research.
- Collegiate Membership of the Royal Colleges of Physicians of the United Kingdom
- The British Medical Association (BMA)—Uganda and Kenya Branches (colonial era)
- The Kenya Medical Association (KMA)
- Kenya Medical Department of the colonial British East Africa
- Royal Entomological Society of London
- International Congresses of Entomology
Awards and Honors
- Research fellow — The London School of Hygiene & Tropical Medicine fellowship, London, United Kingdom.
- Research Grant & Travel Stipend — The Dutch Royal Institute, The Netherlands
- Extramural Medical Research Grant — The United States National Institute of Health (NIH)
- NIH Fellow — The United States National Institute of Health (NIH)
- Bukusu “Omukasa” (a Bukusu folkloric healer or a paramount elder/leader) — Titular folkloric title conferred him by the Bukusu Kenyan ethnic group in gratitude of and respect for his perspicacious successful campaign that saved the tribe from ominous demise due the 1954 epidemic outbreak of enteric or typhoid fever.
- The Royal Society of Tropical Medicine and Hygiene
- Special Achievement and Contribution to Public Health—The East African Bureau of Research in Medicine and Hygiene
- The British Colonial Medical Services at London; Ministry of Health and Housing, Kenya
- Recipient of coveted the United States National Institutes of Health (NIH), Extramural (Medical) Research Program grant
- Twice Panelist at the East Africa High Commission Scientific Conference, Nairobi
- Panelist at a Rural Health Conference of the South Pacific Commission, Tahiti
Legacy
After his death, the Kenyan Ministry of Health and Housing recommended that the Kenya Medical Training Centre at Nairobi be named in his honor and memory. However, the fratricidal tribal politics du jour prevented the Kenyan national legislative body from adopting the de jure process to implement this meritorious proposal by the Ministry of Health and Housing. A multipartite initiative has been relaunched to compel the sitting national government to abide by the 1966 intent to duly honor the memory of this consummate Kenyan statesman, and many other unheralded Kenyan patrons of his generation.
At present, he is commemorated by a family monument at Iboona village in Western Kenya.
Adage
"If I am successful at doing my job, then there shouldn't be need for medical doctors and pharmacists at all; their necessity would be, but, a rarity." —By Dr. Blasio Vincent Ndale Esau Oriedo
References
- ↑ Oriedo et al. "Studies in the epidemiology of East African Leishmaniasis: 1. The circumstantial epidemiology of kala-azar in the Kitui district of Kenya." Transactions of the Royal Society of Tropical Medicine and Hygiene 56.1 (1962): 30-47.
- ↑ Southgate et. al. "Studies in the epidemiology of East African leishmaniasis 2. The human distribution and its determinants." Transactions of the Royal Society of Tropical Medicine and Hygiene 58.5 (1964): 377-390.
- ↑ B.A. Southgate, B.V.E. Oriedo "Studies in the epidemiology of East African leishmaniasis. 5. Leishmania adleri and natural immunity." Journal of Tropical Medicine and Hygiene 70.2 (1967): 33-6.
- ↑ ORIEDO et al. "Studies in Epidemiology of East African Leishmaniasis. 3. Immunity as A Determinant of Geographical Distribution." Journal of Tropical Medicine and Hygiene 70.1 (1967): 1.
- 1 2 Ngure, Peter K., et al. "A review of leishmaniasis in Eastern Africa." Journal of Nanjing Medical University 23.2 (2009): 79-86.
- ↑ World Health Organization. "Report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva 22–26 March 2010."
- ↑ Heyneman, D. "Immunology of leishmaniasis." Bulletin of the World Health Organization 44.4 (1971): 499.
- 1 2 3 The Government of Kenya, Colonial and Postcolonial, Microfilm Collection; Kenya National Archives: Correspondence and Reports 1930 -1970.
- ↑ Ho, Clement. "LibGuides: Microform Collection at American University Library: Country Development Plans & Statistics". subjectguides.library.american.edu. Retrieved 2016-10-29.
- ↑ Kenya National Assembly Official Record: “The official records of the proceedings of the Legislative Council of the Colony and Protectorate of Kenya, the House of Representatives of the Government of Kenya and the National Assembly of the Republic of Kenya.” 1964 (Hansard)
- ↑ Mboya, Tom. A development strategy for Africa: problems and proposals. Ministry of Economic Planning and Development, 1967.
- 1 2 Shachtman, Tom. Airlift to America: How Barack Obama, Sr., John F. Kennedy, Tom Mboya, and 800 East African Students Changed Their World and Ours. Macmillan, 2009.
- ↑ "JFK and the Student Airlift - John F. Kennedy Presidential Library & Museum". www.jfklibrary.org. Retrieved 2016-10-29.
- ↑ KENYA. Committee on Native Land Tenure in the North Kavirondo Reserve. Committee on Native Land Tenure in the North Kavirondo Reserve. Socioeconomic & Political History. Nairobi: Printed by the Government Printer, 1932.
- 1 2 Hastings, Adrian. The Church in Africa, 1450–1950. London: Oxford University Press, 1995.
- ↑ Anderson University and Church of God. "Church of God (Anderson, Ind.) Missionary Board. Missionary Board correspondence. [ca. 1915]-1985." Anderson University and Church of God Archives. Anderson: Anderson University and Church of God Archives, 1994.
- ↑ "Annual reports on the colon..., Vol. 1931 -- Digitized books from the University of Illinois at Urbana-Champaign". libsysdigi.library.illinois.edu. Retrieved 2016-10-30.
- 1 2 Were, Gideon S. "The Making of Kakamega High School: A Tribute to Harold Arthur Waterloo Chapman." Transafrican Journal of History 17 (1988): 186-192.
- ↑ Mukudi, Edith Simba. African contribution to the growth of secular education in North Nyanza, 1920-1945. Diss. 2012.
- ↑ Adler, S. "Leishmania." Advances in parasitology 2 1964: 35-96.
- 1 2 Oriedo et al. "Studies in the epidemiology of East African Leishmaniasis: 1. The circumstantial epidemiology of kala-azar in the Kitui district of Kenya." Transactions of the Royal Society of Tropical Medicine and Hygiene 56.1 (1962): 30-47.
- ↑ ORIEDO et al. "STUDIES IN EPIDEMIOLOGY OF EAST AFRICAN LEISHMANIASIS. 3. IMMUNITY AS A DETERMINANT OF GEOGRAPHICAL DISTRIBUTION." JOURNAL OF TROPICAL MEDICINE AND HYGIENE 70.1 (1967): 1.
- ↑ Southgate, B.A., Oriedo, B.V.E., and Manson-Bahr, P.E.C. "Studies on the vector of kala-azar in Kenya." Proceedings International Congress of Entomology. Ed. Paul. Freeman. London, 1964.
- ↑ Oriedo, BVE and BA: Manson-Bahr, P.E.C. Southgate. "Entomology of the sand fly vectors of Leishmania donovani in East Africa, Workshop." The XII International Congress of Entomology. Ed. Royal Entomological Society London. London: Royal Entomological Society of London, 1964.
- ↑ Oriedo, et. al. "Studies in the epidemiology of East African leishmaniasis." Transactions of the Royal Society of Tropical Medicine and Hygiene 1962: 30.
- ↑ Southgate, BA, Oriedo, BV, and Manson-Bahr, P E C "Studies in the epidemiology of East African leishmaniasis. 3. Epidemiological and Immunity In Kala-Azar." Transactions of the Royal Society of tropical Medicine and Hygiene 1961.
- ↑ Manson-Bahr, P. E. C., R. B. Heisch, and P. C. C. Garnham. "Studies in leishmaniasis in East Africa: IV. The Montenegro test in kala-azar in Kenya."Transactions of the Royal Society of Tropical Medicine and Hygiene 53.5 (1959): 380-383.
- ↑ D'Oliveira Júnior, Argemiro, et al. "Asymptomatic Leishmania chagasi infection in relatives and neighbors of patients with visceral leishmaniasis." Memórias do Instituto Oswaldo Cruz 92 (1997): 15-20.
- 1 2 The XII International Congress of Entomology. London, United Kingdom; 8–16 July 1964.
- ↑ WHO. Declaration of Alma Ata. International conference on primary health care, Alma-Ata, USSR, 6–12 September 1978 Geneva: WHO, 1978.
- 1 2 The colonial medical service in British East Africa. British Colonial Medical Services, London
- 1 2 3 4 5 6 The Government of Kenya “Colonial Medical Service Microfilm Collection; Kenya National Archives: Daily Correspondence and Reports 1930-1967.” (2015).
- 1 2 The Kenya Colony and Protectorate, Annual Medical Report, 1952, Nairobi, Government Printer, 1953.
- 1 2 3 Kitching, Gavin N. Class and Economic Change in Kenya: The making of an African petite bourgeoisie 1905-1970. Yale University Press, 1980.
- ↑ Oriedo, BV "Bully". Unpublished Personal Memoirs and Letters of Blasio Vincent Oriedo 1954 - January 1966.
- ↑ "Register of the Tom Mboya Papers". www.oac.cdlib.org. Retrieved 2016-10-30.
- ↑ The Government of Kenya “Development plan for the period from 1st July 1964 to 30th June 1970” Kenya Economic Policy, Nairobi, Government Printer, 1964[microform].
- ↑ Republic of Kenya. "Notice of Appointments and Personnel Changes: Public Health and Medical Officers, Ministry of Health and Housing." The Kenya Gazette. Nairobi: The Government of The Republic of Kenya, 1966.
- 1 2 3 British Colonial Medical Services, London
- 1 2 3 4 Crozia, Anna. Practising colonial medicine: The colonial medical service in British East Africa. 2007. London : IB Tauris, 2007.
- ↑ Fairfield, Letitia. “COLONIAL MEDICAL SERVICES.” British Medical Journal1.3253 (1923): 789. Print.
- ↑ Tilley, Helen. "Medicine, Empires, and Ethics in Colonial Africa." AMA Journal of Ethics 18.7 (2016): 743.
- ↑ Iliffe, John. East African Doctors: a history of the modern profession. Vol. 95. Cambridge University Press, 1998. Page 78
- 1 2 3 The National Archives of The United Kingdom: The East Africa Commission. "The Records & Correspondences of The British Colonial Medical Service in Colonial Medical Service in the Archives the Archives: The Colony of Kenya 1945 - 1966." The National Archives of The United Kingdom, 1945 - 1966.
- ↑ John B. George et. al. “Correspondences to The United States Institute of Current World Affairs, Washington, D.C.: The Interterritorial Medical Research Funding—The East African High Commission." The United States Institute of Current World Affairs 1952 - 1964
- 1 2 3 4 Institute of Current World Affairs, The United Stated States of America: "Medical Research activities in the British colonial territories of Kenya, Uganda, Tanganyika, and Zanzibar funded by the institute and facilitated via the East Africa High Commission (EAHC): The East African Bureau of Research in Medical and Hygiene". Unpublished newsletter correspondences, 1948 - 62.
- ↑ Wall, Rosemary. "Practising Colonial Medicine: The Colonial Medical Service in British East Africa." Social History of Medicine 22.1 (2009): 215-217.
- ↑ Greenwood, Anna, and Harshad Topiwala. Indian Doctors in Kenya, 1895-1940: The Forgotten History. Springer, 2016.
- ↑ Roberts, JMD “The control of epidemic malaria in the highlands of western Kenya. Part I. Before the campaign.” Journal of Tropical Medicine and Hygiene 1964; 67:161–8
- 1 2 3 Roberts, J. M. D. "The control of epidemic malaria in the highlands of western Kenya. Part II. The campaign." Journal of Tropical Medicine and Hygiene 67.8 (1964): 191-9.
- 1 2 Roberts, JMD “The control of epidemic malaria in the highlands of western Kenya. Part III. After the campaign.” Journal of Tropical Medicine and Hygiene 1964; 67:230–7
- 1 2 East African Institute of Malaria & Vector Borne Diseases, 1961/62
- 1 2 Hay, Simon I. et al. “Clinical Epidemiology of Malaria in the Highlands of Western Kenya.” Emerging Infectious Diseases 8.6 (2002): 543–548. PMC. Web. 30 Aug. 2016.
- 1 2 3 Snow RW, Ikoku A, Omumbo J, Ouma J “The epidemiology, politics and control of malaria epidemics in Kenya: 1900–1998.” Report prepared for Roll Back Malaria, Resource Network on Epidemics, World Health Organization. Nairobi: KEMRI/Wellcome Trust Collaborative Programme; 1999
- ↑ Kohn, George C. Encyclopedia of plague and pestilence: from ancient times to the present. Infobase Publishing, 2007.
- ↑ Dean, Reginald FA. "Treatment of kwashiorkor with moderate amounts of protein." The Journal of pediatrics 56.5 (1960): 675-689.
- ↑ Davies, J. N. P. "Nutrition and nutritional diseases." Annual review of medicine 3.1 (1952): 99-132.
- ↑ Roberts, J. M. D., et al. "Onchocerciasis in Kenya 9, 11 and 18 years after elimination of the vector." Bulletin of the World Health Organization 37.2 (1967): 195.
- ↑ WHO Report on Malaria in Sub-Saharan Africa 1900 - 1990
- ↑ Mudhune, Sandra A., et al. "The clinical burden of malaria in Nairobi: a historical review and contemporary audit." Malaria journal 10.1 (2011): 1.
- ↑ Hay, S., et al. "Clinical epidemiology of malaria in the highlands of western Kenya." Emerging infectious diseases 8.6 (2002).
- ↑ "British, African, American & Asian studies archival online and microfilm publications | Microform Academic Publishers - ISBN prefix 978185117". microform.digital. Retrieved 2016-10-31.
- ↑ The Kenya Colony and Protectorate, Annual Medical Report, 1960, Nairobi, Government Printer, 1961.
- ↑ Annual Report of the Colonies, Kenya, 1961
- ↑ Abdullahi, Ali Arazeem. “Trends and Challenges of Traditional Medicine in Africa.” African Journal of Traditional, Complementary, and Alternative Medicines 8.5 Suppl (2011): 115–123.
- ↑ Bettini, S., S. Pampiglione, and M. Maroli. "Studies on Mediterranean leishmaniasis: V. A preliminary epidemiological survey of human leishmaniasis in Tuscany." Transactions of the Royal Society of Tropical Medicine and Hygiene71.1 (1977): 73-79.
- 1 2 Elnaiem, Dia‐Eldin A. "Ecology and control of the sand fly vectors of Leishmania donovani in East Africa, with special emphasis on Phlebotomus orientalis." Journal of Vector Ecology 36.s1 (2011): S23-S31.
- ↑ Shaw, J. J., and Ralph Lainson. "Leishmaniasis in Brazil: X. Some observations on intradermal reactions to different trypanosomatid antigens of patients suffering from cutaneous and mucocutaneous leishmaniasis." Transactions of the Royal Society of Tropical Medicine and Hygiene 69.3 (1975): 323-335.
- ↑ D'Oliveira Júnior, Argemiro, et al. "Asymptomatic Leishmania chagasi infection in relatives and neighbors of patients with visceral leishmaniasis."Memórias do Instituto Oswaldo Cruz 92 (1997): 15-20.
- ↑ Malaria Consortium. "Leishmaniasis control in eastern Africa: Past and present efforts and future needs." Situation and gap analysis 86 (2010).
- ↑ Diesfeld, Hans Jochen, and Hans K. Hecklau.Kenya: a geomedical monograph. Vol. 5. Springer Science & Business Media, 2013.
- ↑ Dechant, W., et al. "Post kala-azar uveitis." British Journal of Ophthalmology 64.9 (1980): 680-683.
- ↑ Pampiglione, S., et al. "Studies in Mediterranean leishmaniasis: 3. The leishmanin skin test in kala-azar." Transactions of the Royal Society of Tropical Medicine and Hygiene 69.1 (1975): 60-68.
- ↑ Mutinga, M. J., et al. "The isolation and identification of leishmanial parasites from domestic dogs in the Machakos District of Kenya, and the possible role of dogs as reservoirs of kala-azar in East Africa." Annals of Tropical Medicine & Parasitology 74.2 (1980): 139-144.
- ↑ Southgate, B. A. "Studies in the epidemiology of East African leishmaniasis. 5. Leishmania adleri and natural immunity." Journal of Tropical Medicine and Hygiene 70.2 (1967): 33-6.
- ↑ Southgate, B. A., and P. E. C. Manson-Bahr. "Studies in the epidemiology of East African leishmaniasis. 4. The significance of the positive leishmanin test." Journal of Tropical Medicine and Hygiene 70.2 (1967): 29-33.
- ↑ Wijers, D. J. B., and D. M. Minter. "Studies on the vector of kala-azar in Kenya: V.—The outbreak in Meru district." Annals of Tropical Medicine & Parasitology 1966: 11-21.
- ↑ Wijers, D. J. B., and D. M. Minter. "Studies on the vector of kala-azar in Kenya: V.—The outbreak in Meru district." Annals of Tropical Medicine & Parasitology 1966: 11-21.
- ↑ Wijers, D. J. B., and S. Mwangi. "Studies on the vector of kala-azar in Kenya: VI.—Environmental epidemiology in Meru district." . Annals of Tropical Medicine & Parasitology 1966: 373-391.
- ↑ SOUTHGATE, BA. "MANSON-BAHR PEC-Studies in the epidemiology of East African leishmaniasis." J Trop Med Hyg 70 (1968): 29-36.
Notes
- 1 2 Interesting to note that his father, Esau Oriedo, as a district representative to the Local Native Council (LNC) of North Nyanza — a.k.a. North Kavirondo District Council — was an ardent advocate for literacy and higher education, and a key protagonist in the founding of the school under the auspices of the North Kavirondo District LNC in 1932.
- ↑ Robbed of his intrepid and prescient advocacy at the fore personally, the region's healthcare, akin to other civil infrastructures became derelict.
- ↑ In a communiqué, he cautioned the nascent Kenyan political cadre of the liberation movement against a gullibility towards an impetuous independence—opining that such impetuous move, meagerly developed civil institutions, could lead to a vacuous independence and vassalage statehood, unless wholesome tactical and strategic civil institution infrastructures were in place to remedy the situation at the time of independence. He argued that Africans du jour had yet to achieve sufficient critical-to-success intellectual, healthcare, and socioeconomic resources and infrastructure for a comprehensive wholesome liberation—Africanized self-governance. During his epidemiological research and fight against disease epidemics, in the rustic and urbanite regions across East and Central Africa, he’d come face-to-face with the abominable high rates of poverty among the native populations those regions, the economic hardship that was a consequence of the repugnantly undue health care and hygienic woes which most aboriginals endured.
- ↑ Below is an abstract of the book "Indians in the Colonial Medical Service. Indian Doctors in Kenya, 1895–1940." by Greenwood and Topiwala which cogently contextualizes lack of attention and the unheralded fate of African and Indian healthcare practitioners, such as Dr. BV “Bully” Oriedo, who worked contemporaneously in higher status positions within the British African Colonial Medical Services. “It is very curious that Indian [and African] doctors have been ignored in the colonial medical history of Africa. Although scholars have examined the European doctors of the various African Colonial Medical Services, non-white personnel have received comparatively little attention. Some studies have looked at the lower ranked African personnel, but the experiences of the Indian [and African] doctors that worked contemporaneously in higher status positions have received no attention. Indeed, the studies of non-European doctors in the Indian and African Empires have been so infrequent that one could be forgiven for thinking that Indians and Africans had no access to medical education and therefore were not employed in anything other than positions that did not require professional qualifications. Mark Harrison has briefly touched upon the Indian staff cohort of the Indian Medical Service (IMS) and Ryan Johnson has examined the progressive exclusion of the small numbers of black doctors from the West African Medical Service from the beginnings of the twentieth century. But these studies are exceptions, with much of the historiography focusing on either the white elites or the black subordinates, with little or no acknowledgement of non-white qualified practitioners. Indeed, even the broad histories of the East African medical administration written by Anne Beck in the 1960s and 1970s did not consider the work of Indians [and Africans who worked contemporaneously in higher status positions] within the colonial health department.”
- ↑ He was a dedicated medical research scientist and prolific technical writer. He meticulously gathered and documented clinical experiments and patient biomedical data, patient biometric screening, and practical field observations. This is evident by the innumerable notebooks which he accumulated.
- ↑ The Filariasis Research Unit was established in the British colonial East Africa in 1949. 1950 the British colonial East Africa High Commission assumed direct responsibility of the unit. Its establishment was at the initiative of the Colonial Medical Research Committee.
- ↑ It’s utterly incomprehensible and outright iniquitous that following Dr. Oriedo’s precipitously inexplicable death at age 34 the postcolonial Kenyan authorities and those who succeeded him were derelict of the valuable progress, successes, and a robustly dynamic public health infrastructure he’d attained and implemented via his ardent and industrious efforts to stem not just the black fever disease but also a plethora of other tropical diseases including malaria, typhoid, and malnutrition. Not only did the postcolonial Kenyan authorities and those who succeeded him fail to sustain his achievements, but also critical resources were deallocated leading to dilapidation of civil infrastructure and a lack of a meaningful public health strategy. Today, in Kenya and east Africa, tropical diseases such as black fever and malaria have become “Neglected Tropical Diseases” (NTD)!
- ↑ Inopportunely, postcolonial Kenyan authorities failed to adequately embrace the value of intellectual property, which brought about a lack of an effective information management strategy; thus, a loss of precious apolitical knowledge—such as medical science—or critical programs and infrastructures. This has a knowledge chasm. The Kenya school milk program is a classic example of the “reinventing the wheel” cliché. Per Bwibo et. al., The Journal of nutrition 133.11 (2003): 3936S-3940S, the program was started in 1982 by the president of the Republic of Kenya. Au contraire, in 1960 the school milk program had been implemented in Kenya and Uganda by the du jour government administration pursuant to Dr. BV Oriedo’s strategy to stem the kwashiorkor disease. Moreover, the program was a constituent of a multi-part dynamic public health strategy which he helped to spearhead.
- ↑ It should be noted that these approaches had previously been successfully used in the 1940s in Nairobi
- ↑ The plan was unpretentious. The primary objective was to improve health wellness (The absence of disease or infirmity—optimal physical and mental well-being—stemming adverse socioeconomic, sociocultural and socioecological consequences of disease.) and intellectual & civic infrastructure standards across the Eastern Africa region. One of the chief provisos focused on pupils from daycare through college. Every single pupil was required to participate in health and fitness education programs. School officials were tasked with implementing and sustaining pertinent performance indexed programs which included maintaining each pupil’s health and hygiene records that included weekly hygiene, nutritional, and fitness assessments. Thus, school officials were tasked with compliance, whereas public health officials were tasked with formulation, implementation, and enforcement.
- ↑ It’s worth noting that scholarly publication was an enduring grievance for African medical or scientific researchers (i.e., a very small number, predominantly physicians, du jour in the entire East and Central African region). Whites arrogated unadulterated credit and published under their own names research often pioneered and conducted by these African scientific avant-gardists. African scientific or medical researchers, and medical professionals were relegated to servitude roles and faced perpetual subordination, whites considered themselves superior whatever their rank or intellectual capacity.