Decidua
| Decidua | |
|---|---|
 Diagrammatic sections of the uterine mucous membrane: A. The non-pregnant uterus. B. Decidua parietalis; the mucous membrane in the pregnant uterus and not beneath the placenta. | |
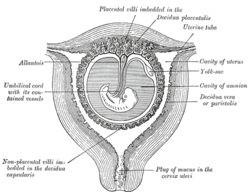 Sectional plan of the gravid uterus in the third and fourth month. | |
| Identifiers | |
| MeSH | A16.759.289 |
| Code | TE E6.0.1.4.0.0.7 |
Decidua is the term for the uterine lining (endometrium) during a pregnancy, which forms the maternal part of the placenta. It is formed under the influence of progesterone and forms highly characteristic cells.
Etymology
The word comes from the Latin deciduus, meaning falling off or shedding.
Background
After ovulation, in placental mammals, the endometrial lining becomes hypertrophic and vascular under the influence of oestrogens and progesterone.
In animals exhibiting hemochorial placentation, the endometrium then undergoes decidualization following implantation to form the decidua. If this does not occur, the secretory lining will be absorbed (estrous cycle) or shed (menstrual cycle).
The decidua is shed with the placenta during parturition.
Structure
The part of the decidua that interacts with the trophoblast is the decidua basalis (also called decidua placentalis), while the decidua capsularis grows over the embryo on the luminal side, enclosing it into the endometrium. The remainder of the decidua is termed the decidua parietalis or decidua vera, and it will fuse with the decidua capsularis by the fourth month of gestation.
Three morphologically distinct layers of the decidua basalis can then be described:
- Compact outer layer (stratum compactum)
- Intermediate layer (stratum spongiosum)
- Boundary layer adjacent to the myometrium (stratum basalis)
Within the decidua, occasional fibrinoid deposits form where the syncytiotrophoblast is damaged. The region of fibrinoid deposition where trophoblasts meet the compact portion of the decidua basalis is called Rohr's layer, while the fibrinoid deposits that occur between the compact and spongy layer of the decidua basalis is termed Nitabuch's layer. This layer is absent in placenta accreta.[1]
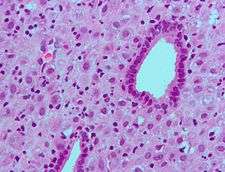
The decidua has a histologically-distinct appearance, displaying large polygonal decidual cells in the stroma. These are enlarged endometrial stromal cells, which resemble epithelium (and are referred to as "epithelioid").
Decidualization includes the process of differentiation of the spindle-shape stromal fibroblasts into the plump secretory decidual cells, which create a pericellular extracellular matrix rich in fibronectin and laminin (similar to epithelial cells).
Vascularity, as well as vascular permeability, is enhanced in the decidualizing endometrium.
Its leukocyte population is distinct, with the presence of large endometrial granular leukocytes being predominant, while polynuclear leukocytes and B cells are scant.
The large granular lymphocytes (CD56 bright) are called "uterine NK cells" or "uNK cells" in mice, and "decidual NK cells" or "dNK cells" in humans.
Role
As the maternal interface to the embryo the decidua participates in the exchanges of nutrition, gas, and waste with the gestation. It also protects the pregnancy from the maternal immune system. Further, the decidua has to allow a very controlled invasion of the trophoblast.
In invasive placental disorders like placenta accreta decidualization have been consistently found to be deficient.
Hormone production
The decidua secretes hormones, growth factors, and cytokines. It has receptors for estrogen, progesterone, growth hormone, and others.
Among its products are hormones commonly associated with other organs such as cortisol, CRF, GnRH, prolactin, and relaxin. Decidual prolactin is not under dopaminergic control.
Pregnancy protein 14 (PP-14), also called placental protein 12, and Insulin-like growth factor-binding protein 1(IGFBP1) appear to be specific products of the secretory and decidual lining.
Other factors released include interleukin-15 and vascular endothelial growth factor (VEGF). A reasonable understanding of the role and interplay of these hormones and factors has not been evolved.
Other

- In case of an extrauterine pregnancy, the endometrium nevertheless becomes decidualized. A woman may shed the lining in the form of a decidual cast, which may be mistaken as a miscarriage, when, in fact, the ectopic pregnancy still persists.
- A decidual reaction can be observed in tissue of the peritoneum and ovary during a pregnancy, and represents a response of stromal tissue to progesterone.
- Decidua in a lymph node may mimic metastatic carcinoma.[2]
Pathology
A long-lasting infection of the decidua, chronic deciduitis, is associated with pre-term labour.[3]
Additional images
 Scheme of placental circulation.
Scheme of placental circulation.
References
- ↑ Cunningham, F. Gary, ed. (2005). Williams obstetrics (22nd ed.). New York ; Toronto: McGraw-Hill Professional. ISBN 9780071413152.
- ↑ Wu, DC.; Hirschowitz, S.; Natarajan, S. (May 2005). "Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall". Arch Pathol Lab Med. 129 (5): e117–20. PMID 15859655. doi:10.1043/1543-2165(2005)129<E117:EDOPLN>2.0.CO;2 (inactive 2017-01-15).
- ↑ Edmondson, N.; Bocking, A.; Machin, G.; Rizek, R.; Watson, C.; Keating, S. (2009). "The prevalence of chronic deciduitis in cases of preterm labor without clinical chorioamnionitis". Pediatr Dev Pathol. 12 (1): 16–21. PMID 18171100. doi:10.2350/07-04-0270.1.
External links
- Histologic picture at med.utah.edu
- Gray's s12
- Histology image: 19904loa – Histology Learning System at Boston University
