Cyclophosphamide
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌsaɪkloʊˈfɒsfəˌmaɪd, -lə-/[1][2] |
| Trade names | Lyophilized Cytoxan, Endoxan, Cytoxan, Neosar, Procytox, Revimmune, Cycloblastin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682080 |
| Pregnancy category | |
| Routes of administration | by mouth, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | >75% (by mouth) |
| Protein binding | >60% |
| Metabolism | Liver |
| Biological half-life | 3–12 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.000.015 |
| Chemical and physical data | |
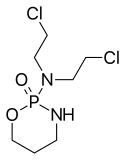
| Formula | C7H15Cl2N2O2P |
| Molar mass | 261.086 g/mol |
| 3D model (JSmol) | |
| Melting point | 2 °C (36 °F) |
| |
| |
| (verify) | |
Cyclophosphamide (CP), also known as cytophosphane among other,[3] is a medication used as chemotherapy and to suppress the immune system.[4] As chemotherapy it is used to treat lymphoma, multiple myeloma, leukemia, ovarian cancer, breast cancer, small cell lung cancer, neuroblastoma, and sarcoma. As an immune suppressor it is used in nephrotic syndrome and following organ transplant. It is taken by mouth or injection into a vein.[4]
Most people develop side effects. Common side effects include low white blood cell counts, loss of appetite, vomiting, hair loss, and bleeding from the bladder. Other severe side effects include an increased future risk of cancer, infertility, allergic reactions, and pulmonary fibrosis. Cyclophosphamide is in the alkylating agent and nitrogen mustard family of medications. It works by interfering with the duplication of DNA and the creation of RNA.[4]
Cyclophosphamide was approved for medical use in the United States in 1959.[4] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[5] The wholesale cost in the developing world is about 3.65 to 14.30 USD per 1 g vial.[6] In the United Kingdom this dose costs the NHS about 17.06 pounds.[7] In the United States this dose by mouth is about 19.56 USD.[8]
Medical uses
Cyclophosphamide is used to treat cancers and autoimmune diseases. It is used to quickly control the disease. Because of its toxicity, it is replaced as soon as possible by less toxic drugs. Regular and frequent laboratory evaluations are required to monitor kidney function, avoid drug-induced bladder complications and screen for bone marrow toxicity.
It is used in medicine for treating certain cancers of the Islets of Langerhans and used in medical research to produce an animal model for Type 1 diabetes in a large dose as well as Type 2 diabetes with multiple low doses.
Cancer

The main use of cyclophosphamide is with other chemotherapy agents in the treatment of lymphomas, some forms of brain cancer, neuroblastoma, leukemia,[9] and some solid tumors.[10] It is a chemotherapy drug that works by inducing the death of certain T cells.
Autoimmune diseases
Cyclophosphamide decreases the immune system's response, and although concerns about toxicity restrict its use to patients with severe disease, it remains an important treatment for life-threatening autoimmune diseases where disease-modifying antirheumatic drugs (DMARDs) have been ineffective. For example, systemic lupus erythematosus with severe lupus nephritis[11] may respond to pulsed cyclophosphamide. Cyclophosphamide is also used to treat minimal change disease,[12] severe rheumatoid arthritis,[13] granulomatosis with polyangiitis[14] and multiple sclerosis.[15]
AL amyloidosis
Cyclophosphamide, used in combination with thalidomide or lenalidomide and dexamethasone has documented efficacy as an off-label treatment of AL amyloidosis. It appears to be an alternative to the more traditional treatment with melphalan in people who are ill-suited for autologous stem cell transplant.[16]
Contraindications
Like other alkylating agents, cyclophosphamide is teratogenic and contraindicated in pregnant women (Pregnancy Category D) except for life-threatening circumstances in the mother.[17][18] Additional relative contraindications to the use of cyclophosphamide include lactation, active infection, neutropenia or bladder toxicity.
Cyclophosphamide is a Pregnancy Category D drug and causes birth defects. First trimester exposure to cyclophosphamide for the treatment of cancer or lupus displays a pattern of anomalies labeled "cyclophosphamide embryopathy," including growth restriction, ear and facial abnormalities, absence of digits and hypoplastic limbs.[19][20] Women previously treated with alkylating agents are often able to conceive and deliver healthy children.[21][22]
Side effects
Adverse drug reactions from cyclophosphamide are related to the cumulative medication dose and include chemotherapy-induced nausea and vomiting,[23] bone marrow suppression,[24] stomach ache, hemorrhagic cystitis, diarrhea, darkening of the skin/nails, alopecia (hair loss) or thinning of hair, changes in color and texture of the hair and lethargy. Other side effects may include easy bruising/bleeding, joint pain, mouth sores, slow-healing existing wounds, unusual decrease in the amount of urine or unusual tiredness or weakness.
Pulmonary injury appears rare,[25] but can present with two clinical patterns: an early, acute pneumonitis and a chronic, progressive fibrosis.[26] Cardiotoxicity is a major problem with people treated with higher dose regimens.[27]
High-dose intravenous cyclophosphamide can cause the syndrome of inappropriate antidiuretic hormone secretion (SIADH) and a potentially fatal hyponatremia when compounded by intravenous fluids administered to prevent drug-induced cystitis.[28] While SIADH has been described primarily with higher doses of cyclophosphamide, it can also occur with the lower doses used in the management of inflammatory disorders.[29]
Bladder bleeding
Acrolein is toxic to the bladder epithelium and can lead to hemorrhagic cystitis, which is associated with microscopic or gross hematuria and occasionally dysuria.[30] Risks of hemorrhagic cystitis can be minimized with adequate fluid intake, avoidance of nighttime dosage and mesna (sodium 2-mercaptoethane sulfonate), a sulfhydryl donor which binds and detoxifies acrolein.[31][32] Intermittent dosing of cyclophosphamide decreases cumulative drug dose, reduces bladder exposure to acrolein and has equal efficacy to daily treatment in the management of lupus nephritis.[33]
Infection
Neutropenia or lymphoma arising secondary to cyclophosphamide usage can predispose people to a variety of bacterial, fungal and opportunistic infections.[34] No published guidelines cover PCP prophylaxis for people with rheumatological diseases receiving immunosuppressive drugs, but some advocate its use when receiving high-dose medication.[35][36]
Infertility
Cyclophosphamide has been found to significantly increase the risk of premature menopause in females and of infertility in males and females, the likelihood of which increases with cumulative drug dose and increasing patient age. Such infertility is usually temporary, but can be permanent.[37] The use of leuprolide in women of reproductive age before administration of intermittently dosed cyclophosphamide may diminish the risks of premature menopause and infertility.[38]
Cancer
Cyclophosphamide is carcinogenic and may increase the risk of developing lymphomas, leukemia, skin cancer, transitional cell carcinoma of the bladder or other malignancies.[39] Myeloproliferative neoplasms, including acute leukemia, non-Hodgkin lymphoma and multiple myeloma, occurred in 5 of 119 rheumatoid arthritis patients within the first decade after receiving cyclophosphamide, compared with one case of chronic lymphocytic leukemia in 119 rheumatoid arthritis patients with no history.[40] Secondary acute myeloid leukemia (therapy-related AML, or "t-AML") is thought to occur either by cyclophosphamide-inducing mutations or selecting for a high-risk myeloid clone.[41] This risk may be dependent on dose and other factors, including the condition, other agents or treatment modalities (including radiotherapy), treatment length and intensity. For some regimens, it is rare. For instance, CMF-therapy for breast cancer (where the cumulative dose is typically less than 20 grams of cyclophosphamide) carries an AML risk of less than 1/2000, with some studies finding no increased risk compared to background. Other treatment regimens involving higher doses may carry risks of 1–2% or higher. Cyclophosphamide-induced AML, when it happens, typically presents some years after treatment, with incidence peaking around 3–9 years. After nine years, the risk falls to background. When AML occurs, it is often preceded by a myelodysplastic syndrome phase, before developing into overt acute leukemia. Cyclophosphamide-induced leukemia will often involve complex cytogenetics, which carries a worse prognosis than de novo AML.
Pharmacology
Oral cyclophosphamide is rapidly absorbed and then converted by mixed-function oxidase enzymes (cytochrome P450 system) in the liver to active metabolites.[42][43] The main active metabolite is 4-hydroxycyclophosphamide, which exists in equilibrium with its tautomer, aldophosphamide. Most of the aldophosphamide is then oxidised by the enzyme aldehyde dehydrogenase (ALDH) to make carboxycyclophosphamide. A small proportion of aldophosphamide freely diffuses into cells, where it is decomposed into two compounds, phosphoramide mustard and acrolein.[44] The active metabolites of cyclophosphamide are highly protein bound and distributed to all tissues, are assumed to cross the placenta and are known to be present in breast milk.[45]
It is specifically in the oxazaphosphorine group of medications.[46]
Cyclophosphamide metabolites are primarily excreted in the urine unchanged, and drug dosing should be appropriately adjusted in the setting of renal dysfunction.[47] Drugs altering hepatic microsomal enzyme activity (e.g., alcohol, barbiturates, rifampicin, or phenytoin) may result in accelerated metabolism of cyclophosphamide into its active metabolites, increasing both pharmacologic and toxic effects of the drug; alternatively, drugs that inhibit hepatic microsomal enzymes (e.g. corticosteroids, tricyclic antidepressants, or allopurinol) result in slower conversion of cyclophosphamide into its metabolites and consequently reduced therapeutic and toxic effects.[48]
Cyclophosphamide reduces plasma pseudocholinesterase activity and may result in prolonged neuromuscular blockade when administered concurrently with succinylcholine.[49][50] Tricyclic antidepressants and other anticholinergic agents can result in delayed bladder emptying and prolonged bladder exposure to acrolein.
Mechanism of action
The main effect of cyclophosphamide is due to its metabolite phosphoramide mustard. This metabolite is only formed in cells that have low levels of ALDH. Phosphoramide mustard forms DNA crosslinks both between and within DNA strands at guanine N-7 positions (known as interstrand and intrastrand crosslinkages, respectively). This is irreversible and leads to cell apoptosis.[51]
Cyclophosphamide has relatively little typical chemotherapy toxicity as ALDHs are present in relatively large concentrations in bone marrow stem cells, liver and intestinal epithelium. ALDHs protect these actively proliferating tissues against toxic effects of phosphoramide mustard and acrolein by converting aldophosphamide to carboxycyclophosphamide that does not give rise to the toxic metabolites phosphoramide mustard and acrolein. This is because carboxycyclophosphamide cannot undergo β-elimination (the carboxylate acts as an electron-donating group, forbidding the transformation), preventing nitrogen mustard activation and subsequent alkylation.[30][52][53]
Cyclophosphamide induces beneficial immunomodulatory effects in adaptive immunotherapy. Suggested mechanisms include:[54]
- Elimination of T regulatory cells (CD4+CD25+ T cells) in naive and tumor-bearing hosts
- Induction of T cell growth factors, such as type I IFNs, and/or
- Enhanced grafting of adoptively transferred, tumor-reactive effector T cells by the creation of an immunologic space niche.
Thus, cyclophosphamide preconditioning of recipient hosts (for donor T cells) has been used to enhance immunity in naïve hosts, and to enhance adoptive T cell immunotherapy regimens, as well as active vaccination strategies, inducing objective antitumor immunity.
History
As reported by O. M. Colvin in his study of the development of cyclophosphamide and its clinical applications,
Phosphoramide mustard, one of the principal toxic metabolites of cyclophosphamide, was synthesized and reported by Friedman and Seligman in 1954[55] …It was postulated that the presence of the phosphate bond to the nitrogen atom could inactivate the nitrogen mustard moiety, but the phosphate bond would be cleaved in gastric cancers and other tumors which had a high phosphamidase content. However, in studies carried out after the clinical efficacy of cyclophosphamide was demonstrated, phosphoramide mustard proved to be cytotoxic in vitro (footnote omitted), but to have a low therapeutic index in vivo.[56]
Cyclophosphamide and the related nitrogen mustard–derived alkylating agent ifosfamide were developed by Norbert Brock and ASTA (now Baxter Oncology). Brock and his team synthesised and screened more than 1,000 candidate oxazaphosphorine compounds.[57] They converted the base nitrogen mustard into a nontoxic "transport form". This transport form was a prodrug, subsequently actively transported into cancer cells. Once in the cells, the prodrug was enzymatically converted into the active, toxic form. The first clinical trials were published at the end of the 1950s.[58][59][60] In 1959 it became the eighth cytotoxic anticancer agent to be approved by the FDA.[30]
Society and culture
The abbreviation CP is common, although abbreviating drug names is not best practice in medicine.[61]
Research
Because of its impact on the immune system, it is used in animal studies. Rodents are injected intraperitoneally with either a single dose of 150 mg/kg or two doses (150 and 100 mg/kg) spread over two days.[62] This can be used for applications such as:
- The EPA may be concerned about potential human pathogenicity of an engineered microbe when conducting an MCAN review. Particularly for bacteria with potential consumer exposure they require testing of the microbe on immuno-compromised rats [63]
- Cyclophosphamide provides a positive control when studying immune-response of a new drug.[64]
References
- ↑ "cyclophosphamide - definition of cyclophosphamide in English from the Oxford dictionary". OxfordDictionaries.com. Retrieved 2016-01-20.
- ↑ "cyclophosphamide". Merriam-Webster Dictionary.
- ↑ "NCI Drug Dictionary". National Cancer Institute. Retrieved 20 December 2016.
- 1 2 3 4 "Cyclophosphamide". The American Society of Health-System Pharmacists. Retrieved 8 December 2016.
- ↑ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Retrieved 8 December 2016.
- ↑ "Cyclophosphamide". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- ↑ British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 580. ISBN 9780857111562.
- ↑ "NADAC as of 2016-12-07 | Data.Medicaid.gov". Centers for Medicare and Medicaid Services. Retrieved 20 December 2016.
- ↑ Shanafelt TD, Lin T, Geyer SM, et al. (June 2007). "Pentostatin, cyclophosphamide, and rituximab regimen in older patients with chronic lymphocytic leukemia". Cancer. 109 (11): 2291–8. PMID 17514743. doi:10.1002/cncr.22662.
- ↑ Young SD, Whissell M, Noble JC, Cano PO, Lopez PG, Germond CJ (May 2006). "Phase II clinical trial results involving treatment with low-dose daily oral cyclophosphamide, weekly vinblastine, and rofecoxib in patients with advanced solid tumors". Clinical Cancer Research. 12 (10): 3092–8. PMID 16707607. doi:10.1158/1078-0432.CCR-05-2255.
- ↑ Steinberg AD, Kaltreider HB, Staples PJ, Goetzl EJ, Talal N, Decker JL (August 1971). "Cyclophosphamide in lupus nephritis: a controlled trial". Annals of Internal Medicine. 75 (2): 165–71. PMID 4104337. doi:10.7326/0003-4819-75-2-165.
- ↑ Brenner and Rector's The Kidney: Volume 8
- ↑ Townes AS, Sowa JM, Shulman LE (1976). "Controlled trial of cyclophosphamide in rheumatoid arthritis". Arthritis and Rheumatism. 19 (3): 563–73. PMID 779796. doi:10.1002/art.1780190308.
- ↑ Novack SN, Pearson CM (April 1971). "Cyclophosphamide therapy in Wegener's granulomatosis". The New England Journal of Medicine. 284 (17): 938–42. PMID 5551803. doi:10.1056/NEJM197104292841703.
- ↑ Makhani N, Gorman MP, Branson HM, Stazzone L, Banwell BL, Chitnis T (June 2009). "Cyclophosphamide therapy in pediatric multiple sclerosis". Neurology. 72 (24): 2076–82. PMC 2923592
 . PMID 19439723. doi:10.1212/WNL.0b013e3181a8164c.
. PMID 19439723. doi:10.1212/WNL.0b013e3181a8164c. - ↑ Gertz (Dec 2014). "update on diagnosis, prognosis, and treatment". Am J Hematol. 89 (12): 1132–40. PMID 25407896. doi:10.1002/ajh.23828.
- ↑ Kirshon B, Wasserstrum N, Willis R, Herman GE, McCabe ER (September 1988). "Teratogenic effects of first-trimester cyclophosphamide therapy". Obstetrics and Gynecology. 72 (3 Pt 2): 462–4. PMID 3136412.
- ↑ Clowse ME, Magder L, Petri M (2005). "Cyclophosphamide for lupus during pregnancy". Lupus. 14 (8): 593–7. PMID 16175930. doi:10.1191/0961203305lu2169oa.
- ↑ Enns GM, Roeder E, Chan RT, Ali-Khan Catts Z, Cox VA, Golabi M (September 1999). "Apparent cyclophosphamide (cytoxan) embryopathy: a distinct phenotype?". American Journal of Medical Genetics. 86 (3): 237–41. PMID 10482872. doi:10.1002/(SICI)1096-8628(19990917)86:3<237::AID-AJMG8>3.0.CO;2-V.
- ↑ Vaux KK, Kahole NC, Jones KL (June 2003). "Cyclophosphamide, methotrexate, and cytarabine embropathy: is apoptosis the common pathway?". Birth Defects Research. Part a, Clinical and Molecular Teratology. 67 (6): 403–8. PMID 12962283. doi:10.1002/bdra.10060.
- ↑ Huong DL, Amoura Z, Duhaut P, et al. (December 2002). "Risk of ovarian failure and fertility after intravenous cyclophosphamide. A study in 84 patients". The Journal of Rheumatology. 29 (12): 2571–6. PMID 12465154.
- ↑ Ramsey-Goldman R, Mientus JM, Kutzer JE, Mulvihill JJ, Medsger TA (July 1993). "Pregnancy outcome in women with systemic lupus erythematosus treated with immunosuppressive drugs". The Journal of Rheumatology. 20 (7): 1152–7. PMID 8371208.
- ↑ Singh G, Fries JF, Williams CA, Zatarain E, Spitz P, Bloch DA (February 1991). "Toxicity profiles of disease modifying antirheumatic drugs in rheumatoid arthritis". The Journal of Rheumatology. 18 (2): 188–94. PMID 1673721.
- ↑ Lohrmann HP (1984). "The problem of permanent bone marrow damage after cytotoxic drug treatment". Oncology. 41 (3): 180–4. PMID 6374556. doi:10.1159/000225819.
- ↑ Twohig KJ, Matthay RA (March 1990). "Pulmonary effects of cytotoxic agents other than bleomycin". Clinics in Chest Medicine. 11 (1): 31–54. PMID 1691069.
- ↑ Malik SW, Myers JL, DeRemee RA, Specks U (December 1996). "Lung toxicity associated with cyclophosphamide use. Two distinct patterns". American Journal of Respiratory and Critical Care Medicine. 154 (6 Pt 1): 1851–6. PMID 8970380. doi:10.1164/ajrccm.154.6.8970380.
- ↑ Floyd JD, Nguyen DT, Lobins RL, Bashir Q, Doll DC, Perry MC (October 2005). "Cardiotoxicity of cancer therapy". Journal of Clinical Oncology. 23 (30): 7685–96. PMID 16234530. doi:10.1200/JCO.2005.08.789.
- ↑ Bressler RB, Huston DP (March 1985). "Water intoxication following moderate-dose intravenous cyclophosphamide". Archives of Internal Medicine. 145 (3): 548–9. PMID 3977522. doi:10.1001/archinte.145.3.548.
- ↑ Salido M, Macarron P, Hernández-García C, D'Cruz DP, Khamashta MA, Hughes GR (2003). "Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus". Lupus. 12 (8): 636–9. PMID 12945725. doi:10.1191/0961203303lu421cr.
- 1 2 3 Emadi A, Jones RJ, Brodsky RA (2009). "Cyclophosphamide and cancer: golden anniversary". Nat Rev Clin Oncol. 6 (11): 638–47. PMID 19786984. doi:10.1038/nrclinonc.2009.146.
- ↑ Talar-Williams C, Hijazi YM, Walther MM, et al. (March 1996). "Cyclophosphamide-induced cystitis and bladder cancer in patients with Wegener granulomatosis". Annals of Internal Medicine. 124 (5): 477–84. PMID 8602705. doi:10.7326/0003-4819-124-5-199603010-00003.
- ↑ Monach PA, Arnold LM, Merkel PA (January 2010). "Incidence and prevention of bladder toxicity from cyclophosphamide in the treatment of rheumatic diseases: a data-driven review". Arthritis and Rheumatism. 62 (1): 9–21. PMID 20039416. doi:10.1002/art.25061.
- ↑ Boumpas DT, Austin HA, Vaughn EM, et al. (September 1992). "Controlled trial of pulse methylprednisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis". Lancet. 340 (8822): 741–5. PMID 1356175. doi:10.1016/0140-6736(92)92292-n.
- ↑ Pryor BD, Bologna SG, Kahl LE (September 1996). "Risk factors for serious infection during treatment with cyclophosphamide and high-dose corticosteroids for systemic lupus erythematosus". Arthritis and Rheumatism. 39 (9): 1475–82. PMID 8814058. doi:10.1002/art.1780390906.
- ↑ Ognibene FP, Shelhamer JH, Hoffman GS, et al. (March 1995). "Pneumocystis carinii pneumonia: a major complication of immunosuppressive therapy in patients with Wegener's granulomatosis". American Journal of Respiratory and Critical Care Medicine. 151 (3 Pt 1): 795–9. PMID 7881673. doi:10.1164/ajrccm/151.3_Pt_1.795.
- ↑ Suryaprasad A, Stone JH (July 2008). "When is it safe to stop Pneumocystis jiroveci pneumonia prophylaxis? Insights from three cases complicating autoimmune diseases". Arthritis and Rheumatism. 59 (7): 1034–9. PMID 18576286. doi:10.1002/art.23822.
- ↑ Balow JE, Austin HA, Tsokos GC, Antonovych TT, Steinberg AD, Klippel JH (January 1987). "NIH conference. Lupus nephritis". Annals of Internal Medicine. 106 (1): 79–94. PMID 3789582. doi:10.7326/0003-4819-106-1-79.
- ↑ Periti P, Mazzei T, Mini E (2002). "Clinical pharmacokinetics of depot leuprorelin". Clinical Pharmacokinetics. 41 (7): 485–504. PMID 12083977. doi:10.2165/00003088-200241070-00003.
- ↑ Bernatsky S, Clarke AE, Suissa S (February 2008). "Hematologic malignant neoplasms after drug exposure in rheumatoid arthritis". Archives of Internal Medicine. 168 (4): 378–81. PMID 18299492. doi:10.1001/archinternmed.2007.107.
- ↑ Radis CD, Kahl LE, Baker GL, et al. (August 1995). "Effects of cyclophosphamide on the development of malignancy and on long-term survival of patients with rheumatoid arthritis. A 20-year follow-up study". Arthritis and Rheumatism. 38 (8): 1120–7. PMID 7639809. doi:10.1002/art.1780380815.
- ↑ Larson RA (2007). "Etiology and management of therapy-related myeloid leukemia". Hematology. 2007: 453–9. PMID 18024664. doi:10.1182/asheducation-2007.1.453.
- ↑ Cohen JL, Jao JY (August 1970). "Enzymatic basis of cyclophosphamide activation by hepatic microsomes of the rat". The Journal of Pharmacology and Experimental Therapeutics. 174 (2): 206–10. PMID 4393764.
- ↑ Huttunen KM, Raunio H, Rautio J (September 2011). "Prodrugs--from serendipity to rational design". Pharmacological Reviews. 63 (3): 750–71. PMID 21737530. doi:10.1124/pr.110.003459.
- ↑ Boddy AV, Yule SM (April 2000). "Metabolism and pharmacokinetics of oxazaphosphorines". Clinical Pharmacokinetics. 38 (4): 291–304. PMID 10803453. doi:10.2165/00003088-200038040-00001.
- ↑ Wiernik PH, Duncan JH (May 1971). "Cyclophosphamide in human milk". Lancet. 1 (7705): 912. PMID 4102054. doi:10.1016/s0140-6736(71)92474-3.
- ↑ Giraud, B; et al. (2010), "Oxazaphosphorines: new therapeutic strategies for an old class of drugs", Expert Opin Drug Metab Toxicol, 6 (8): 919–938, PMID 20446865, doi:10.1517/17425255.2010.487861.
- ↑ Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D (April 2002). "Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency". Kidney International. 61 (4): 1495–501. PMID 11918757. doi:10.1046/j.1523-1755.2002.00279.x.
- ↑ Donelli MG, Bartosek I, Guaitani A, et al. (April 1976). "Importance of pharmacokinetic studies on cyclophosphamide (NSC-26271) in understanding its cytotoxic effect". Cancer Treatment Reports. 60 (4): 395–401. PMID 1277213.
- ↑ Koseoglu V, Chiang J, Chan KW (December 1999). "Acquired pseudocholinesterase deficiency after high-dose cyclophosphamide". Bone Marrow Transplantation. 24 (12): 1367–8. PMID 10627651. doi:10.1038/sj.bmt.1702097.
- ↑ Vigouroux D, Voltaire L (1995). "Curarisation prolongée après mivacurium chez une patiente traitée par cyclophosphamide" [Prolonged neuromuscular block induced by mivacurium in a patient treated with cyclophosphamide]. Annales Françaises d'Anesthésie et de Réanimation (in French). 14 (6): 508–10. PMID 8745976. doi:10.1016/S0750-7658(05)80493-9. INIST:2947795.
- ↑ Hall AG, Tilby MJ (September 1992). "Mechanisms of action of, and modes of resistance to, alkylating agents used in the treatment of haematological malignancies". Blood Reviews. 6 (3): 163–73. PMID 1422285. doi:10.1016/0268-960X(92)90028-O.
- ↑ Kohn FR, Sladek NE (1985). "Aldehyde dehydrogenase activity as the basis for the relative insensitivity of murine pluripotent hematopoietic stem cells to oxazaphosphorines". Biochem. Pharmacol. 34 (19): 3465–71. PMID 2996550. doi:10.1016/0006-2952(85)90719-1.
- ↑ Friedman OM, Wodinsky I, Myles A (1976). "Cyclophosphamide (NSC-26271)-related phosphoramide mustards- recent advances and historical perspective". Cancer Treat Rep. 60 (4): 337–46. PMID 1277209.
- ↑ Sistigu A, Viaud S, Chaput N, Bracci L, Proietti E, Zitvogel L (July 2011). "Immunomodulatory effects of cyclophosphamide and implementations for vaccine design". Seminars in Immunopathology. 33 (4): 369–83. PMID 21611872. doi:10.1007/s00281-011-0245-0.
- ↑ Friedman OM, Seligman AM (1954). "Preparation of N-Phosphorylated Derivatives of Bis-β-chloroethylamine1a". Journal of the American Chemical Society. 76 (3): 655–8. doi:10.1021/ja01632a006.
- ↑ Colvin OM (August 1999). "An overview of cyclophosphamide development and clinical applications". Current Pharmaceutical Design. 5 (8): 555–60. PMID 10469891.
- ↑ Brock N (August 1996). "The history of the oxazaphosphorine cytostatics". Cancer. 78 (3): 542–7. PMID 8697402. doi:10.1002/(SICI)1097-0142(19960801)78:3<542::AID-CNCR23>3.0.CO;2-Y.
- ↑ Wilmanns, Hilmar (1958). Chemotherapie maligner Tumoren [Chemotherapy of malignant tumors]. Asta-Forschung und Therapie (in German). OCLC 73296245.
- ↑ Gross R, Wulf G (1959). "Klinische und experimentelle Erfahrungen mit zyk lischen und nichtzyklischen Phosphamidestern des N-Losl in der Chemotherapie von Tumoren" [Clinical and experimental experiences with metallic cyclical and non-cyclical Phosphamidestern the N-losl in the chemotherapy of tumors]. Strahlentherapie (in German). 41: 361–7.
- ↑ Brock N (January 1989). "Oxazaphosphorine cytostatics: past-present-future. Seventh Cain Memorial Award lecture". Cancer Research. 49 (1): 1–7. PMID 2491747.
- ↑ Institute for Safe Medication Practices, ISMP’s List of Error-Prone Abbreviations, Symbols, and Dose Designations (PDF).
- ↑ Zuluaga, Andres F; Salazar, Beatriz E; Rodriguez, Carlos A; Zapata, Ana X; Agudelo, Maria; Vesga, Omar (2006-03-17). "BMC Infectious Diseases". BMC Infectious Diseases. 6 (1): 55. PMC 1434751
 . PMID 16545113. doi:10.1186/1471-2334-6-55.
. PMID 16545113. doi:10.1186/1471-2334-6-55. - ↑ http://www.epa.gov/biotech_rule/pubs/submiss.htm
- ↑ "Immunosuppressive effect of cyclophosphamide on white blood cells and lymphocyte subpopulations from peripheral blood of Balb/c mice". International Immunopharmacology. 11: 1293–1297. doi:10.1016/j.intimp.2011.04.011.