Chagas disease
| Chagas disease | |
|---|---|
| Synonyms | American trypanosomiasis |
 | |
| Photomicrograph of Giemsa-stained Trypanosoma cruzi | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Symptoms | Fever, large lymph nodes, headache[1] |
| Complications | Heart failure, enlarged esophagus, enlarged colon[1] |
| Causes | Trypanosoma cruzi spread by kissing bugs[1] |
| Diagnostic method | Finding the parasite or antibodies in the blood[2] |
| Prevention | Eliminating kissing bugs and avoiding their bites[1] |
| Medication | Benznidazole, nifurtimox[1] |
| Frequency | 6.6 million (2015)[3] |
| Deaths | 8,000 (2015)[4] |
Chagas disease, also known as American trypanosomiasis, is a tropical parasitic disease caused by the protist Trypanosoma cruzi.[1] It is spread mostly by insects known as Triatominae or kissing bugs.[1] The symptoms change over the course of the infection. In the early stage, symptoms are typically either not present or mild, and may include fever, swollen lymph nodes, headaches, or local swelling at the site of the bite.[1] After 8–12 weeks, individuals enter the chronic phase of disease and in 60–70% it never produces further symptoms.[5][2] The other 30 to 40% of people develop further symptoms 10 to 30 years after the initial infection,[2] including enlargement of the ventricles of the heart in 20 to 30%, leading to heart failure.[1] An enlarged esophagus or an enlarged colon may also occur in 10% of people.[1]
T. cruzi is commonly spread to humans and other mammals by the blood-sucking "kissing bugs" of the subfamily Triatominae.[6] These insects are known by a number of local names, including: vinchuca in Argentina, Bolivia, Chile and Paraguay, barbeiro (the barber) in Brazil, pito in Colombia, chinche in Central America, and chipo in Venezuela.[7] The disease may also be spread through blood transfusion, organ transplantation, eating food contaminated with the parasites, and by vertical transmission (from a mother to her fetus).[1] Diagnosis of early disease is by finding the parasite in the blood using a microscope.[2] Chronic disease is diagnosed by finding antibodies for T. cruzi in the blood.[2]
Prevention mostly involves eliminating kissing bugs and avoiding their bites.[1] Other preventative efforts include screening blood used for transfusions.[1] A vaccine has not been developed as of 2013.[1] Early infections are treatable with the medication benznidazole or nifurtimox.[1] Medication nearly always results in a cure if given early, but becomes less effective the longer a person has had Chagas disease.[1] When used in chronic disease, medication may delay or prevent the development of end–stage symptoms.[1] Benznidazole and nifurtimox cause temporary side effects in up to 40% of people[1] including skin disorders, brain toxicity, and digestive system irritation.[5][8][9]
It is estimated that 6.6 million people, mostly in Mexico, Central America and South America, have Chagas disease as of 2015.[3][1] In 2015, Chagas was estimated to result in 8,000 deaths.[4] Most people with the disease are poor,[5] and most do not realize they are infected.[10] Large-scale population movements have increased the areas where Chagas disease is found and these include many European countries and the United States.[1] These areas have also seen an increase in the years up to 2014.[11] The disease was first described in 1909 by Carlos Chagas after whom it is named.[1] Chagas disease is classified as a neglected tropical disease.[12] It affects more than 150 other animals.[5]
Signs and symptoms

The human disease occurs in two stages: an acute stage, which occurs shortly after an initial infection, and a chronic stage that develops over many years.
The acute phase lasts for the first few weeks or months of infection. It usually occurs unnoticed because it is symptom-free or exhibits only mild symptoms that are not unique to Chagas disease. These can include fever, fatigue, body aches, muscle pain, headache, rash, loss of appetite, diarrhea, nausea, and vomiting. The signs on physical examination can include mild enlargement of the liver or spleen, swollen glands, and local swelling (a chagoma) where the parasite entered the body.[13]
The most recognized marker of acute Chagas disease is called Romaña's sign, which includes swelling of the eyelids on the side of the face near the bite wound or where the bug feces were deposited or accidentally rubbed into the eye. Rarely, young children, or adults may die from the acute disease due to severe inflammation/infection of the heart muscle (myocarditis) or brain (meningoencephalitis).[13] The acute phase also can be severe in people with weakened immune systems.[6]
If symptoms develop during the acute phase, they usually resolve spontaneously within three to eight weeks in approximately 90% of individuals.[5][8] Although the symptoms resolve, even with treatment the infection persists and enters a chronic phase. Of individuals with chronic Chagas disease, 60–80% will never develop symptoms (called indeterminate chronic Chagas disease), while the remaining 20–40% will develop life-threatening heart and/or digestive disorders during their lifetime (called determinate chronic Chagas disease). In 10% of individuals, the disease progresses directly from the acute form to a symptomatic clinical form of chronic Chagas disease.[5][8]
The symptomatic (determinate) chronic stage affects the nervous system, digestive system and heart. About two-thirds of people with chronic symptoms have cardiac damage, including dilated cardiomyopathy, which causes heart rhythm abnormalities and may result in sudden death. About one-third of patients go on to develop digestive system damage, resulting in dilation of the digestive tract (megacolon and megaesophagus), accompanied by severe weight loss. Swallowing difficulties (secondary achalasia) may be the first symptom of digestive disturbances and may lead to malnutrition.[14]
20% to 50% of individuals with intestinal involvement also exhibit cardiac involvement.[14] Up to 10% of chronically infected individuals develop neuritis that results in altered tendon reflexes and sensory impairment. Isolated cases exhibit central nervous system involvement, including dementia, confusion, chronic encephalopathy and sensory and motor deficits.[15]
The clinical manifestations of Chagas disease are due to cell death in the target tissues that occurs during the infective cycle, by sequentially inducing an inflammatory response, cellular lesions, and fibrosis. For example, intracellular amastigotes destroy the intramural neurons of the autonomic nervous system in the intestine and heart, leading to megaintestine and heart aneurysms, respectively. If left untreated, Chagas disease can be fatal, in most cases due to heart muscle damage.[14]
Transmission

In Chagas-endemic areas, the main mode of transmission is through an insect vector called a triatomine bug.[6] A triatomine becomes infected with T. cruzi by feeding on the blood of an infected person or animal. During the day, triatomines hide in crevices in the walls and roofs.[6]
The bugs emerge at night, when the inhabitants are sleeping. Because they tend to feed on people's faces, triatomine bugs are also known as "kissing bugs". After they bite and ingest blood, they defecate on the person. Triatomines pass T. cruzi parasites (called trypomastigotes) in feces left near the site of the bite wound.[6]
Scratching the site of the bite causes the trypomastigotes to enter the host through the wound, or through intact mucous membranes, such as the conjunctiva. Once inside the host, the trypomastigotes invade cells, where they differentiate into intracellular amastigotes. The amastigotes multiply by binary fission and differentiate into trypomastigotes, which are then released into the bloodstream. This cycle is repeated in each newly infected cell. Replication resumes only when the parasites enter another cell or are ingested by another vector.[6] (See also: Life cycle and transmission of T. cruzi)
Dense vegetation (such as that of tropical rainforests) and urban habitats are not ideal for the establishment of the human transmission cycle. However, in regions where the sylvatic habitat and its fauna are thinned by economic exploitation and human habitation, such as in newly deforested areas, piassava palm culture areas, and some parts of the Amazon region, a human transmission cycle may develop as the insects search for new food sources.[16]
T. cruzi can also be transmitted through blood transfusions. With the exception of blood derivatives (such as fractionated antibodies), all blood components are infective. The parasite remains viable at 4 °C for at least 18 days or up to 250 days when kept at room temperature. It is unclear whether T. cruzi can be transmitted through frozen-thawed blood components.[17]
Other modes of transmission include organ transplantation, through breast milk,[18] and by accidental laboratory exposure. Chagas disease can also be spread congenitally (from a pregnant woman to her baby) through the placenta, and accounts for approximately 13% of stillborn deaths in parts of Brazil.[19]
Oral transmission is an unusual route of infection, but has been described. In 1991, farm workers in the state of Paraíba, Brazil, were infected by eating contaminated food; transmission has also occurred via contaminated açaí palm fruit juice and garapa.[20][21][22][23][24] A 2007 outbreak in 103 Venezuelan school children was attributed to contaminated guava juice.[25]
Chagas disease is a growing problem in Europe, because the majority of cases with chronic infection are asymptomatic and because of migration from Latin America.[26]
Diagnosis
The presence of T. cruzi is diagnostic of Chagas disease. It can be detected by microscopic examination of fresh anticoagulated blood, or its buffy coat, for motile parasites; or by preparation of thin and thick blood smears stained with Giemsa, for direct visualization of parasites. Microscopically, T. cruzi can be confused with Trypanosoma rangeli, which is not known to be pathogenic in humans. Isolation of T. cruzi can occur by inoculation into mice, by culture in specialized media (for example, NNN, LIT); and by xenodiagnosis,[27] where uninfected Reduviidae bugs are fed on the patient's blood, and their gut contents examined for parasites.[14]
Various immunoassays for T. cruzi are available and can be used to distinguish among strains (zymodemes of T.cruzi with divergent pathogenicities). These tests include: detecting complement fixation, indirect hemagglutination, indirect fluorescence assays, radioimmunoassays, and ELISA. Alternatively, diagnosis and strain identification can be made using polymerase chain reaction (PCR).[14]
Prevention
There is currently no vaccine against Chagas disease.[28] Prevention is generally focused on decreasing the numbers of the insect that spreads it (Triatoma) and decreasing their contact with humans. This is done by using sprays and paints containing insecticides (synthetic pyrethroids), and improving housing and sanitary conditions in rural areas.[29] For urban dwellers, spending vacations and camping out in the wilderness or sleeping at hostels or mud houses in endemic areas can be dangerous; a mosquito net is recommended. Some measures of vector control include:
- A yeast trap can be used for monitoring infestations of certain species of triatomine bugs (Triatoma sordida, Triatoma brasiliensis, Triatoma pseudomaculata, and Panstrongylus megistus).[30]
- Promising results were gained with the treatment of vector habitats with the fungus Beauveria bassiana.[31]
- Targeting the symbionts of Triatominae through paratransgenesis can be done.[32]
A number of potential vaccines are currently being tested. Vaccination with Trypanosoma rangeli has produced positive results in animal models.[33] More recently, the potential of DNA vaccines for immunotherapy of acute and chronic Chagas disease is being tested by several research groups.[34]
Blood transfusion was formerly the second-most common mode of transmission for Chagas disease, but the development and implementation of blood bank screening tests has dramatically reduced this risk in the 21st century. Blood donations in all endemic Latin American countries undergo Chagas screening, and testing is expanding in countries, such as France, Spain and the United States, that have significant or growing populations of immigrants from endemic areas.[35][36] In Spain, donors are evaluated with a questionnaire to identify individuals at risk of Chagas exposure for screening tests.[36]
The US FDA has approved two Chagas tests, including one approved in April 2010, and has published guidelines that recommend testing of all donated blood and tissue products.[36][37] While these tests are not required in US, an estimated 75–90% of the blood supply is currently tested for Chagas, including all units collected by the American Red Cross, which accounts for 40% of the U.S. blood supply.[37][38] The Chagas Biovigilance Network reports current incidents of Chagas-positive blood products in the United States, as reported by labs using the screening test approved by the FDA in 2007.[39]
Management
There are two approaches to treating Chagas disease: antiparasitic treatment, to kill the parasite; and symptomatic treatment, to manage the symptoms and signs of the infection. Management uniquely involves addressing selective incremental failure of the parasympathetic nervous system. Autonomic disease imparted by Chagas may eventually result in megaesophagus, megacolon and accelerated dilated cardiomyopathy. The mechanisms that explain why Chagas targets the parasympathetic autonomic nervous system and spares the sympathetic autonomic nervous system remain poorly understood.
Medication
Antiparasitic treatment is most effective early in the course of infection, but is not limited to cases in the acute phase. Drugs of choice include azole or nitro derivatives, such as benznidazole[40] or nifurtimox. Both agents are limited in their capacity to completely eliminate T. cruzi from the body (parasitologic cure), especially in chronically infected patients, and resistance to these drugs has been reported.[41]
Studies suggest antiparasitic treatment leads to parasitological cure in more than 90% of infants but only about 60–85% of adults treated in the first year of acute phase Chagas disease. Children aged six to 12 years with chronic disease have a cure rate of about 60% with benznidazole. While the rate of cure declines the longer an adult has been infected with Chagas, treatment with benznidazole has been shown to slow the onset of heart disease in adults with chronic Chagas infections.[5][14]
Treatment of chronic infection in women prior to or during pregnancy does not appear to reduce the probability the disease will be passed on to the infant. Likewise, it is unclear whether prophylactic treatment of chronic infection is beneficial in persons who will undergo immunosuppression (for example, organ transplant recipients) or in persons who are already immunosuppressed (for example, those with HIV infection).[14]
Complications
In the chronic stage, treatment involves managing the clinical manifestations of the disease. For example, pacemakers and medications for irregular heartbeats, such as the anti-arrhythmia drug amiodarone, may be life saving for some patients with chronic cardiac disease,[42] while surgery may be required for megaintestine. The disease cannot be cured in this phase, however. Chronic heart disease caused by Chagas disease is now a common reason for heart transplantation surgery. Until recently, however, Chagas disease was considered a contraindication for the procedure, since the heart damage could recur as the parasite was expected to seize the opportunity provided by the immunosuppression that follows surgery.[43]
Epidemiology

Chagas disease affects 8 to 10 million people living in endemic Latin American countries, with an additional 300,000–400,000 living in nonendemic countries, including Spain and the United States. An estimated 41,200 new cases occur annually in endemic countries, and 14,400 infants are born with congenital Chagas disease annually.[5][14] in 2010 it resulted in approximately 10,300 deaths up from 9,300 in 1990.[44]
The disease is present in 18 countries on the American continents, ranging from the southern United States to northern Argentina.[6] Chagas exists in two different ecological zones. In the Southern Cone region, the main vector lives in and around human homes. In Central America and Mexico, the main vector species lives both inside dwellings and in uninhabited areas. In both zones, Chagas occurs almost exclusively in rural areas, where triatomines breed and feed on the more than 150 species from 24 families of domestic and wild mammals, as well as humans, that are the natural reservoirs of T. cruzi.[45]
Although Triatominae bugs feed on them, birds appear to be immune to infection and therefore are not considered to be a T. cruzi reservoir. Even when colonies of insects are eradicated from a house and surrounding domestic animal shelters, they can re-emerge from plants or animals that are part of the ancient, sylvatic (referring to wild animals) infection cycle. This is especially likely in zones with mixed open savannah, with clumps of trees interspersed by human habitation.[46]
The primary wildlife reservoirs for Trypanosoma cruzi in the United States include opossums, raccoons, armadillos, squirrels, woodrats, and mice.[47] Opossums are particularly important as reservoirs, because the parasite can complete its life cycle in the anal glands of this animal without having to re-enter the insect vector.[47] Recorded prevalence of the disease in opossums in the U.S. ranges from 8.3%[47] to 37.5%.[48]
Studies on raccoons in the Southeast have yielded infection rates ranging from 47%[49] to as low as 15.5%.[47] Armadillo prevalence studies have been described in Louisiana, and range from a low of 1.1%[48] to 28.8%.[50] Additionally, small rodents, including squirrels, mice, and rats, are important in the sylvatic transmission cycle because of their importance as bloodmeal sources for the insect vectors. A Texas study revealed 17.3% percent T. cruzi prevalence in 75 specimens representing four separate small rodent species.[51]
Chronic Chagas disease remains a major health problem in many Latin American countries, despite the effectiveness of hygienic and preventive measures, such as eliminating the transmitting insects. However, several landmarks have been achieved in the fight against it in Latin America, including a reduction by 72% of the incidence of human infection in children and young adults in the countries of the Southern Cone Initiative, and at least three countries (Uruguay, in 1997, and Chile, in 1999, and Brazil in 2006) have been certified free of vectorial and transfusional transmission.[14][52][53] In Argentina, vectorial transmission has been interrupted in 13 of the 19 endemic provinces,[52] and major progress toward this goal has also been made in both Paraguay and Bolivia.
Screening of donated blood, blood components, and solid organ donors, as well as donors of cells, tissues, and cell and tissue products for T. cruzi is mandated in all Chagas-endemic countries and has been implemented.[54] Approximately 300,000 infected people live in the United States, which is likely the result of immigration from Latin American countries,[55] and there have been 23 cases acquired from kissing bugs in the United States reported between 1955 and 2014.[56] With increased population movements, the possibility of transmission by blood transfusion became more substantial in the United States. Transfusion blood and tissue products are now actively screened in the U.S., thus addressing and minimizing this risk.[57]
History
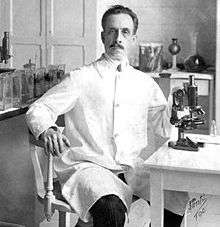
The disease was named after the Brazilian physician and epidemiologist Carlos Chagas, who first described it in 1909.[58][59][60][61] The disease was not seen as a major public health problem in humans until the 1960s (the outbreak of Chagas disease in Brazil in the 1920s went widely ignored[62]). Dr Chagas discovered that the intestines of Triatomidae (now Reduviidae: Triatominae) harbored a flagellate protozoan, a new species of the Trypanosoma genus, and was able to demonstrate experimentally that it could be transmitted to marmoset monkeys that were bitten by the infected bug. Later studies showed squirrel monkeys were also vulnerable to infection.[63]
Chagas named the pathogenic parasite as Trypanosoma cruzi[58] and later that year as Schizotrypanum cruzi,[60] both honoring Oswaldo Cruz, the noted Brazilian physician and epidemiologist who successfully fought epidemics of yellow fever, smallpox, and bubonic plague in Rio de Janeiro and other cities in the beginning of the 20th century. Chagas was also the first to unknowingly discover and illustrate the parasitic fungal genus Pneumocystis, later infamously linked to PCP (Pneumocystis pneumonia in AIDS victims).[59] Confusion between the two pathogens' life-cycles led him to briefly recognize his genus Schizotrypanum, but following the description of Pneumocystis by others as an independent genus, Chagas returned to the use of the name Trypanosoma cruzi.
In Argentina, the disease is known as mal de Chagas-Mazza, in honor of Salvador Mazza, the Argentine physician who in 1926 began investigating the disease and over the years became the principal researcher of this disease in the country.[64] Mazza produced the first scientific confirmation of the existence of Trypanosoma cruzi in Argentina in 1927, eventually leading to support from local and European medical schools and Argentine government policy makers.[65]
It has been hypothesized that Charles Darwin might have suffered from Chagas disease as a result of a bite of the so-called great black bug of the Pampas (vinchuca) (see Charles Darwin's illness). The episode was reported by Darwin in his diaries of the Voyage of the Beagle as occurring in March 1835 to the east of the Andes near Mendoza. Darwin was young and generally in good health, though six months previously he had been ill for a month near Valparaiso, but in 1837, almost a year after he returned to England, he began to suffer intermittently from a strange group of symptoms, becoming incapacitated for much of the rest of his life. Attempts to test Darwin's remains at Westminster Abbey by using modern PCR techniques were met with a refusal by the Abbey's curator.[66]
Research
Several experimental treatments have shown promise in animal models. These include inhibitors of oxidosqualene cyclase and squalene synthase,[67][68] cysteine protease inhibitors,[67][69] dermaseptins collected from frogs in the genus Phyllomedusa (P. oreades and P. distincta),[70] the sesquiterpene lactone dehydroleucodine (DhL), which affects the growth of cultured epimastigote-phase Trypanosoma cruzi,[71] inhibitors of purine uptake,[67] and inhibitors of enzymes involved in trypanothione metabolism.[72] Hopefully, new drug targets may be revealed following the sequencing of the T. cruzi genome.[73]
Chagas disease has a serious economic impact on the United States and the world. The cost of treatment in the United States alone, where the disease is not indigenous, is estimated to be $900 million annually, which includes hospitalization and medical devices such as pacemakers. The global cost is estimated at $7 billion.[74]
Megazol in a study seems more active against Chagas than benznidazole but has not been studied in humans.[75] A Chagas vaccine (TcVac3) has been found to be effective in mice with plans for studies in dogs. It is hoped that it will be commercially available by 2018.[76]
See also
- Drugs for Neglected Diseases Initiative
- Chagas: Time to Treat campaign
- Association for the Promotion of Independent Disease Control in Developing Countries
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 "Chagas disease (American trypanosomiasis) Fact sheet N°340". World Health Organization. March 2013. Retrieved 23 February 2014.
- 1 2 3 4 5 Rassi A Jr, Rassi A, Marcondes de Rezende J (June 2012). "American trypanosomiasis (Chagas disease)". Infectious disease clinics of North America. 26 (2): 275–91. PMID 22632639. doi:10.1016/j.idc.2012.03.002.
- 1 2 GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015.". Lancet. 388 (10053): 1545–1602. PMC 5055577
 . PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/S0140-6736(16)31678-6. - 1 2 GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015.". Lancet. 388 (10053): 1459–1544. PMID 27733281. doi:10.1016/s0140-6736(16)31012-1.
- 1 2 3 4 5 6 7 8 Rassi A, Rassi A, Marin-Neto JA (April 2010). "Chagas disease". Lancet. 375 (9723): 1388–402. PMID 20399979. doi:10.1016/S0140-6736(10)60061-X.
- 1 2 3 4 5 6 7 "DPDx – Trypanosomiasis, American. Fact Sheet". Centers for Disease Control (CDC). Retrieved 12 May 2010.
- ↑ Maudlin I, Holmes PH, Miles MA, eds. (2004). The Trypanosomiases. Wallingford: CAB International. p. 184. ISBN 9780851990347.
- 1 2 3 Bern C, Montgomery SP, Herwaldt BL, et al. (November 2007). "Evaluation and treatment of chagas disease in the United States: a systematic review". JAMA. 298 (18): 2171–81. PMID 18000201. doi:10.1001/jama.298.18.2171.
- ↑ Rassi A, Dias JC, Marin-Neto JA, Rassi A (April 2009). "Challenges and opportunities for primary, secondary, and tertiary prevention of Chagas' disease". Heart. 95 (7): 524–34. PMID 19131444. doi:10.1136/hrt.2008.159624.
- ↑ Capinera JL, ed. (2008). Encyclopedia of entomology (2nd ed.). Dordrecht: Springer. p. 824. ISBN 9781402062421.
- ↑ Bonney, Kevin M. (2014). "Chagas disease in the 21st Century: a public health success or an emerging threat?". Parasite. 21: 11. ISSN 1776-1042. PMC 3952655
 . PMID 24626257. doi:10.1051/parasite/2014012.
. PMID 24626257. doi:10.1051/parasite/2014012. 
- ↑ "Neglected Tropical Diseases". cdc.gov. June 6, 2011. Retrieved 28 November 2014.
- 1 2 Guimarães FN, da Silva NN, Clausell DT, de Mello AL, Rapone T, Snell T, Rodrigues N (1968). "Um surto epidêmico de doença de Chagas de provável transmissão digestiva, ocorrido em Teutonia (Estrêla – Rio Grande Do Sul)". Hospital (Rio J) (in Portuguese). 73 (6): 1767–804. PMID 4976999.
- 1 2 3 4 5 6 7 8 9 Louis V Kirchhoff (17 December 2010). "Chagas Disease (American Trypanosomiasis)". eMedicine. Retrieved 12 May 2010.
- ↑ Córdova E, Maiolo E, Corti M, Orduña T (April 2010). "Neurological manifestations of Chagas' disease". Neurol. Res. 32 (3): 238–44. PMID 20406601. doi:10.1179/016164110X12644252260637.
- ↑ Teixeira AR, Monteiro PS, Rebelo JM (2001). "Emerging Chagas disease: trophic network and cycle of transmission of Trypanosoma cruzi from palm trees in the Amazon". Emerging Infect Dis. 7 (1): 100–12. PMC 2631687
 . PMID 11266300. doi:10.3201/eid0701.010115.
. PMID 11266300. doi:10.3201/eid0701.010115. - ↑ Wendel S (January 2010). "Transfusion transmitted Chagas disease: Is it really under control?". Acta Trop. 115 (1–2): 28–34. PMID 20044970. doi:10.1016/j.actatropica.2009.12.006. Retrieved 13 May 2010.
- ↑ Santos Ferreira C, Amato Neto V, Gakiya E, Bezerra RC, Alarcón RS (2003). "Microwave treatment of human milk to prevent transmission of Chagas disease". Revista do Instituto de Medicina Tropical de São Paulo. 45 (1): 41–2. PMID 12751321. doi:10.1590/S0036-46652003000100008.
- ↑ Hudson L, Turner MJ (November 1984). "Immunological consequences of infection and vaccination in South American trypanosomiasis [and discussion]". Philosophical Transactions of the Royal Society B. 307 (1131): 51–61. Bibcode:1984RSPTB.307...51H. JSTOR 2990154. PMID 6151688. doi:10.1098/rstb.1984.0108. Retrieved 22 February 2007 through JSTOR.
- ↑ Benchimol-Barbosa PR (2006). "The oral transmission of Chagas' disease: an acute form of infection responsible for regional outbreaks.". Int J Cardiol. 112 (1): 132–3. PMID 16600406. doi:10.1016/j.ijcard.2005.11.087.
- ↑ Benchimol-Barbosa PR (2010). "Trends on acute Chagas' disease transmitted by oral route in Brazil: steady increase in new cases and a concealed residual fluctuation.". Int J Cardiol. 145 (3): 494–6. PMID 19762096. doi:10.1016/j.ijcard.2009.08.030.
- ↑ "Chagas' disease (American trypanosomiasis) in southern Brazil" (PDF). CDR Weekly. United Kingdom Health Protection Agency. 15 (13). April 2005. Retrieved 26 November 2007.
- ↑ Shikanai-Yasuda MA, Marcondes CB, Guedes LA (1991). "Possible oral transmission of acute Chagas' disease in Brazil". Rev Inst Med Trop São Paulo. 33 (5): 351–7. PMID 1844961. doi:10.1590/S0036-46651991000500003.
- ↑ da Silva Valente SA, de Costa Valente V, Neto HF (1999). "Considerations on the epidemiology and transmission of Chagas disease in the Brazilian Amazon". Mem Inst Oswaldo Cruz. 94 Suppl 1: 395–8. PMID 10677763. doi:10.1590/s0074-02761999000700077.
- ↑ Alarcón de Noya B, Díaz-Bello Z, Colmenares C, et al. (2010). "Large urban outbreak of orally acquired acute Chagas disease at a school in Caracas, Venezuela". J Infect Dis. 201 (9): 1308–15. PMID 20307205. doi:10.1086/651608.
- ↑ Roca C, Pinazo MJ, López-Chejade P, Bayó J, Posada E, López-Solana J, Gállego M, Portús M, Gascón J, Chagas-Clot Research Group (2011). Da Costa Santiago H, ed. "Chagas Disease among the Latin American Adult Population Attending in a Primary Care Center in Barcelona, Spain". PLoS Negl Trop Dis. 5 (4): e1135. PMC 3082512
 . PMID 21572511. doi:10.1371/journal.pntd.0001135.
. PMID 21572511. doi:10.1371/journal.pntd.0001135. - ↑ Brumpt E (1914). "Le xénodiagnostic. Application au diagnostic de quelques infections parasitaires et en particulier à la trypanosomose de Chagas" (PDF). Bull Soc Pathol Exot. 7 (10): 706–10. Archived from the original (PDF) on 26 November 2008.
- ↑ "A killer that preys on the poor: Chagas disease" (pdf). Médecins Sans Frontières: Activity Report 2003/2004. Retrieved 29 August 2008.
- ↑ Eduardo N. Zerba (1999). "Susceptibility and resistance to insecticides of Chagas disease vectors" (PDF). Medicina (Buenos Aires). 59 (Suppl 2): 41–6.
- ↑ Pires HH, Lazzari CR, Diotaiuti L, Lorenzo MG (June 2000). "Performance of yeast-baited traps with Triatoma sordida, Triatoma brasiliensis, Triatoma pseudomaculata, and Panstrongylus megistus in laboratory assays". Rev Panam Salud Publica. 7 (6): 384–8. PMID 10949899. doi:10.1590/S1020-49892000000600005.
- ↑ Luz C, Rocha LF, Nery GV, Magalhães BP, Tigano MS (March 2004). "Activity of oil-formulated Beauveria bassiana against Triatoma sordida in peridomestic areas in Central Brazil". Mem Inst Oswaldo Cruz. 99 (2): 211–8. PMID 15250478. doi:10.1590/S0074-02762004000200017.
- ↑ Beard CB, Cordon-Rosales C, Durvasula RV (2002). "Bacterial symbionts of the Triatominae and their potential use in control of Chagas disease transmission". Annu Rev Entomol. 47: 123–41. PMID 11729071. doi:10.1146/annurev.ento.47.091201.145144.
- ↑ Basso B, Moretti E, Fretes R (June 2008). "Vaccination with epimastigotes of different strains ofTrypanosoma rangeli protects mice against Trypanosoma cruzi infection". Mem Inst Oswaldo Cruz. 103 (4): 370–4. PMID 18660992. doi:10.1590/S0074-02762008000400010.
- ↑ Dumonteil E, Escobedo-Ortegon J, Reyes-Rodriguez N, Arjona-Torres A, Ramirez-Sierra M (2004). "Immunotherapy of Trypanosoma cruzi Infection with DNA Vaccines in Mice". Infect Immun. 72 (1): 46–53. PMC 343959
 . PMID 14688079. doi:10.1128/IAI.72.1.46-53.2004.
. PMID 14688079. doi:10.1128/IAI.72.1.46-53.2004. - ↑ Castro E (February 2009). "Chagas' disease: lessons from routine donation testing". Transfus Med. 19 (1): 16–23. PMID 19302451. doi:10.1111/j.1365-3148.2009.00915.x. Retrieved 12 May 2010.
- 1 2 3 Gascon J, Bern C, Pinazo MJ (July 2009). "Chagas disease in Spain, the United States and other non-endemic countries". Acta Trop. 115 (1–2): 22–7. PMID 19646412. doi:10.1016/j.actatropica.2009.07.019. Retrieved 12 May 2010.
- 1 2 "FDA Approves Chagas Disease Screening Test for Blood, Tissue and Organ Donors". Retrieved 12 May 2010.
- ↑ "Infectious Disease Testing". American Red Cross. Retrieved 12 May 2010.
- ↑ "Chagas' Biovigilance Network". Retrieved 12 May 2010.
- ↑ Garcia S, Ramos CO, Senra JF (April 2005). "Treatment with Benznidazole during the Chronic Phase of Experimental Chagas' Disease Decreases Cardiac Alterations". Antimicrob Agents Chemother. 49 (4): 1521–8. PMC 1068607
 . PMID 15793134. doi:10.1128/AAC.49.4.1521-1528.2005.
. PMID 15793134. doi:10.1128/AAC.49.4.1521-1528.2005. - ↑ Buckner FS, Wilson AJ, White TC, Van Voorhis WC (December 1998). "Induction of Resistance to Azole Drugs in Trypanosoma cruzi". Antimicrob Agents Chemother. 42 (12): 3245–50. PMC 106029
 . PMID 9835521.
. PMID 9835521. - ↑ Dubner S, Schapachnik E, Riera AR, Valero E (2008). "Chagas disease: state-of-the-art of diagnosis and management". Cardiol J. 15 (6): 493–504. PMID 19039752.
- ↑ Bocchi EA, Bellotti G, Mocelin AO (June 1996). "Heart transplantation for chronic Chagas' heart disease". Ann Thorac Surg. 61 (6): 1727–33. PMID 8651775. doi:10.1016/0003-4975(96)00141-5.
- ↑ Lozano R (15 December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. PMID 23245604. doi:10.1016/S0140-6736(12)61728-0.
- ↑ Morel CM, Lazdins J (October 2003). "Chagas disease". Nat Rev Microbiol. 1 (1): 14–5. PMID 15040175. doi:10.1038/nrmicro735.
- ↑ Pinto-Dias JC (1992). "Epidemiology of Chagas disease". In Wendel S, Brener Z, Camargo ME, Rassi A. Chagas Disease – American Trypanosomiasis: its impact on transfusion and clinical medicine. ISBT Brazil '92. XXII Congress of the International Society of Blood Transfusion. XX Brazilian Congress of Hematology. Extraordinary Congress of the Brazilian College of Hematology. São Paulo: Editorial ISBT Brazil. OCLC 69892472. Retrieved 11 September 2008.
- 1 2 3 4 Karsten V, Davis C, Kuhn R (June 1992). "Trypanosoma cruzi in wild raccoons and opossums in North Carolina". J Parasitol. 78 (3): 547–9. JSTOR 3283667. PMID 1597808. doi:10.2307/3283667.
- 1 2 Barr SC, Brown CC, Dennis VA, Klei TR (August 1991). "The lesions and prevalence of Trypanosoma cruzi in opossums and armadillos from southern Louisiana". J Parasitol. 77 (4): 624–7. JSTOR 3283170. PMID 1907654. doi:10.2307/3283170.
- ↑ Yabsley MJ, Noblet GP (1 January 2002). "Seroprevalence of Trypanosoma cruzi in raccoons from South Carolina and Georgia". J Wildl Dis. 38 (1): 75–83. PMID 11838232. doi:10.7589/0090-3558-38.1.75.
- ↑ Yaeger RG (March 1988). "The prevalence of Trypanosoma cruzi infection in armadillos collected at a site near New Orleans, Louisiana". Am J Trop Med Hyg. 38 (2): 323–6. PMID 3128127.
- ↑ Burkholder JE, Allison TC, Kelly VP (April 1980). "Trypanosoma cruzi (Chagas) (Protozoa: Kinetoplastida) in invertebrate, reservoir, and human hosts of the lower Rio Grande valley of Texas". J Parasitol. 66 (2): 305–11. JSTOR 3280824. PMID 6771371. doi:10.2307/3280824.
- 1 2 "The Southern Cone Initiative: an update". Special Programme for Research and Training in Tropical Diseases (TDR) (Press release). WHO. 2004. Archived from the original on 22 September 2009. Retrieved 29 August 2008.
- ↑ Massad E (September 2008). "The elimination of Chagas' disease from Brazil". Epidemiol Infect. 136 (9): 1153–64. PMC 2870925
 . PMID 18053273. doi:10.1017/S0950268807009879.
. PMID 18053273. doi:10.1017/S0950268807009879. - ↑ Castro E (February 2009). "Chagas' disease: lessons from routine donation testing". Transfus Med. 19 (1): 16–23. PMID 19302451. doi:10.1111/j.1365-3148.2009.00915.x. Retrieved 13 May 2010.
- ↑ "Medical Encyclopedia: Chagas disease". National Institutes of Health. Retrieved 11 September 2008.
- ↑ Montgomery SP, Starr MC, Cantey PT, Edwards MS, Meymandi SK (May 2014). "Neglected Parasitic Infections in the United States: Chagas Disease". Am J Trop Med Hyg. 90 (5): 814–818. doi:10.4269/ajtmh.13-0726.
- ↑ Kirchhoff LV (August 1993). "American trypanosomiasis (Chagas' disease) – a tropical disease now in the United States". N Engl J Med. 329 (9): 639–44. PMID 8341339. doi:10.1056/NEJM199308263290909.
- 1 2 Chagas C (1909). "Neue Trypanosomen". Vorläufige Mitteilung Arch Schiff Tropenhyg. 13: 120–2.
- 1 2 Redhead SA, Cushion MT, Frenkel JK, Stringer JR (2006). "Pneumocystis and Trypanosoma cruzi: nomenclature and typifications". J Eukaryot Microbiol. 53 (1): 2–11. PMID 16441572. doi:10.1111/j.1550-7408.2005.00072.x.
- 1 2 Chagas C (1909). "Nova tripanozomiase humana: Estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen., n. sp., ajente etiolojico de nova entidade morbida do homem [New human trypanosomiasis. Studies about the morphology and life-cycle of Schizotripanum cruzi, etiological agent of a new morbid entity of man]". Mem Inst Oswaldo Cruz. 1 (2): 159–218. ISSN 0074-0276. doi:10.1590/S0074-02761909000200008. (in Portuguese with German full translation as "Ueber eine neue Trypanosomiasis des Menschen.")
- ↑ Kropf SP, Sá MR (July 2009). "The discovery of Trypanosoma cruzi and Chagas disease (1908–1909): tropical medicine in Brazil". Hist Cienc Saude Manguinhos. 16 (Suppl 1): 13–34. PMID 20027916. doi:10.1590/s0104-59702009000500002.
- ↑ Coutinho M (June 1999). "Review of Historical Aspects of American Trypanosomiasis (Chagas' Disease) by Matthias Perleth". Isis. 90 (2): 397. JSTOR 237120. doi:10.1086/384393.
- ↑ Hulsebos LH, Choromanski L, Kuhn RE (1989). "The effect of interleukin-2 on parasitemia and myocarditis in experimental Chagas' disease". J Protozool. 36 (3): 293–8. PMID 2499678. doi:10.1111/j.1550-7408.1989.tb05366.x.
- ↑ "Enfermedad de Chagas – Mazza" (in Spanish). Asociación Lucha Contra el Mal de Chagas. Archived from the original on 16 September 2011. Retrieved 15 September 2011.
- ↑ "Historia de la enfermedad de Chagas" (in Spanish). Archived from the original on 4 December 2009.
- ↑ Adler D (1989). "Darwin's Illness". Isr J Med Sci. 25 (4): 218–21. PMID 2496051.
- 1 2 3 Scientific Working Group on Chagas Disease [April 2005] (July 2007). Guhl F, Lazdins-Helds JK (eds.): Reporte del grupo de trabajo científico sobre la enfermedad de Chagas Archived 17 December 2008 at the Wayback Machine. (in Spanish). Geneva: WHO. Retrieved on 29 August 2008. summary in English
- ↑ Urbina JA, Concepcion JL, Rangel S, Visbal G, Lira R (2002). "Squalene synthase as a chemotherapeutic target in Trypanosoma cruzi and Leishmania mexicana". Mol Biochem Parasitol. 125 (1–2): 35–45. PMID 12467972. doi:10.1016/S0166-6851(02)00206-2.
- ↑ Engel JC, Doyle PS, Hsieh I, McKerrow JH (August 1998). "Cysteine Protease Inhibitors Cure an Experimental Trypanosoma cruzi Infection". J Exp Med. 188 (4): 725–34. PMC 2213346
 . PMID 9705954. doi:10.1084/jem.188.4.725.
. PMID 9705954. doi:10.1084/jem.188.4.725. - ↑ Brand GD, Leite JR, Silva LP (December 2002). "Dermaseptins from Phyllomedusa oreades and Phyllomedusa distincta. Anti-Trypanosoma cruzi activity without cytotoxicity to mammalian cells". J Biol Chem. 277 (51): 49332–40. PMID 12379643. doi:10.1074/jbc.M209289200.
- ↑ Brengio SD, Belmonte SA, Guerreiro E, Giordano OS, Pietrobon EO, Sosa MA (April 2000). "The sesquiterpene lactone dehydroleucodine (DhL) affects the growth of cultured epimastigotes of Trypanosoma cruzi". J Parasitol. 86 (2): 407–12. ISSN 0022-3395. PMID 10780563. doi:10.1645/0022-3395(2000)086[0407:TSLDDA]2.0.CO;2.
- ↑ Fairlamb AH, Cerami A (1992). "Metabolism and functions of trypanothione in the Kinetoplastida". Annu Rev Microbiol. 46: 695–729. PMID 1444271. doi:10.1146/annurev.mi.46.100192.003403.
- ↑ El-Sayed NM, Myler PJ, Bartholomeu DC (July 2005). "The genome sequence of Trypanosoma cruzi, etiologic agent of Chagas disease". Science. 309 (5733): 409–15. Bibcode:2005Sci...309..409E. PMID 16020725. doi:10.1126/science.1112631.
- ↑ Bruce Y Lee; Kristina M Bacon; Maria Elena Bottazzi; Peter J Hotez (April 2013). "Global economic burden of Chagas disease: a computational simulation model". The Lancet infectious diseases. 13 (4): 342–348. doi:10.1016/S1473-3099(13)70002-1.
- ↑ Hall BS, Wilkinson SR (2012). "Activation of Benznidazole by Trypanosomal Type I Nitroreductases Results in Glyoxal Formation". Antimicrob. Agents Chemother. 56 (1): 115–123. PMC 3256028
 . PMID 22037852. doi:10.1128/AAC.05135-11.
. PMID 22037852. doi:10.1128/AAC.05135-11. - ↑ "Potential Chagas vaccine candidate shows unprecedented efficacy". ScienceDaily. March 26, 2013. Retrieved 12 January 2015.
Further reading
- "Blood donor screening for Chagas disease — (United States, 2006–2007)". Morbidity and Mortality Weekly Report. 56 (7): 141–43. 23 February 2007. PMID 17318113.
- Franco-Paredes C, Von A, Hidron A, et al. (2007). "Chagas disease: an impediment in achieving the Millennium Development Goals in Latin America". BMC International Health and Human Rights. 7: 7. PMC 2034380
 . PMID 17725836. doi:10.1186/1472-698X-7-7.
. PMID 17725836. doi:10.1186/1472-698X-7-7. - Hotez PJ, Dumonteil E, Woc-Colburn L, et al. (29 May 2012). "Chagas disease: 'The new HIV/AIDS of the Americas'". PLoS Neglected Tropical Diseases. 6 (5): e1498. PMC 3362306
 . PMID 22666504. doi:10.1371/journal.pntd.0001498. An editorial.
. PMID 22666504. doi:10.1371/journal.pntd.0001498. An editorial. - "International symposium to commemorate the 90th anniversary of the discovery of Chagas disease (Rio de Janeiro, April 11–16, 1999)". Memorias do Instituto Oswaldo Cruz. 94 (Suppl. I). 1999. A special issue of the Memórias do Instituto Oswaldo Cruz, covering all aspects of Chagas Disease
- Miles MW, Tyler KM (2003). American trypanosomiasis. Boston: Kluwer Academic. ISBN 978-1-4020-7323-6. OCLC 50685296.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
| Wikimedia Commons has media related to Chagas disease. |
- Chagas disease at DMOZ
- Chagas information at the U.S. Centers for Disease Control
- Chagas information from the Drugs for Neglected Diseases initiative
- UNHCO site on Chagas Disease
- Chagas Disease information for travellers from IAMAT (International Association for Medical Assistance to Travellers)