Central venous catheter
| Central venous catheter | |
|---|---|
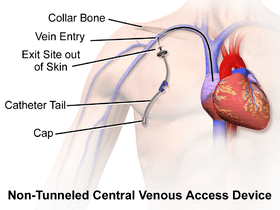 Diagram showing a tunneled central line inserted into the right subclavian vein. | |
| MeSH | D002405 |
A central venous catheter (CVC), also known as a central line, central venous line, or central venous access catheter, is a catheter placed into a large vein. Catheters can be placed in veins in the neck (internal jugular vein), chest (subclavian vein or axillary vein), groin (femoral vein), or through veins in the arms (also known as a PICC line, or peripherally inserted central catheters). It is used to administer medication or fluids that are unable to be taken by mouth or would harm a smaller peripheral vein, obtain blood tests (specifically the "central venous oxygen saturation"), and measure central venous pressure.[1][2]
Medical uses

- Syringe with local anesthetic
- Scalpel in case venous cutdown is needed
- Sterile gel for ultrasound guidance
- Introducer needle (here 18 Ga) on syringe with saline to detect backflow of blood upon vein penetration
- Guide wire
- Tissue dilator
- Indwelling catheter (here 16 Ga)
- Additional fasteners, and corresponding surgical thread
- Dressing

Reasons for the use of central lines include:
- Long-term intravenous antibiotics
- Long-term parenteral nutrition, especially in chronically ill persons
- Long-term pain medications
- Chemotherapy
- Drugs that are prone to cause phlebitis in peripheral veins (caustic), such as:
- Calcium chloride
- Chemotherapy
- Hypertonic saline
- Potassium chloride (KCl)
- Amiodarone
- Vasopressors (for example, epinephrine, dopamine)
- Plasmapheresis
- Peripheral blood stem cell collections
- Dialysis
- Frequent blood draws
- Frequent or persistent requirement for intravenous access
- Need for intravenous therapy when peripheral venous access is impossible
- Monitoring of the central venous pressure (CVP) in acutely ill people to quantify fluid balance[1]
Central venous catheters usually remain in place for a longer period than other venous access devices, especially when the reason for their use is longstanding (such as total parenteral nutrition in a chronically ill person). For such indications, a Hickman line, a PICC line, or a Port-a-Cath may be considered because of their smaller infection risk. Sterile technique is highly important here, as a line may serve as an entry point for pathogenic organisms. Additionally, the line itself may become infected with bacteria such as Staphylococcus aureus and coagulase-negative Staphylococci.[3]
Complications
Central line insertion may cause several complications. The benefit expected from their use should outweigh the risk of those complications.
Pneumothorax
Pneumothorax (for central lines placed in the chest); the incidence is thought to be higher with subclavian vein catheterization. In catheterization of the internal jugular vein, the risk of pneumothorax is minimized by the use of ultrasound guidance. For experienced clinicians, the incidence of pneumothorax is about 1.5-3.1%. The National Institute for Health and Clinical Excellence (UK) and other medical organizations recommend the routine use of ultrasonography to minimize complications.[4]
Bloodstream infections
All catheters can introduce bacteria into the bloodstream, but CVCs are known for occasionally causing Staphylococcus aureus and Staphylococcus epidermidis sepsis. The problem of central line-associated bloodstream infections (CLABSI) has gained increasing attention in recent years.[5] They cause a great deal of morbidity (harm) and deaths, and increase health care costs. Historically, a few CVC infections were considered an acceptable risk of placing central lines. However, the groundbreaking work by Dr. Peter Pronovost at Johns Hopkins Hospital turned that perspective on its head. From 2003 to 2006, the Agency for Healthcare Research and Quality provided $300,000 a year to fund the Comprehensive Unit-Based Safety Program (CUSP) that helped participating hospitals in Michigan lower CLABSIs. By 2012, the project had become a $20 million nationwide initiative.[6] Additionally, the Institute for Healthcare Improvement (IHI) has done a tremendous amount of work in improving hospitals' focus on central line-associated bloodstream infections (CLABSI), and is working to decrease the incidence of this particular complication among US hospitals. The IHI and CLABSI has identified proper hand washing by the performing provider, sterile draping over the person, thorough cleaning of the insertion site, and daily review for ongoing CVC need as key ways to decrease infection rate.
The National Patient Safety Goals require documentation of a checklist for CVC insertion and Disinfection of intravenous (IV) access ports before use (scrub the hub). Some literature has suggested the use of a safer vascular access route, like intraosseous (IO) vascular access, when central lines are not necessary (for example, when central lines are being placed only for vascular access). Infection risks were initially thought to be less in jugular lines, but the decreased rate of infection is only seen in obese people.[7]
If a central line infection is suspected in a person, blood cultures are taken from both the catheter and a vein elsewhere in the body. If the culture from the central line grows bacteria much earlier (>2 hours) than the other vein site, the line is likely infected. Quantitative blood culture is even more accurate, but this method is not widely available.[8]
Generally, antibiotics are used, and occasionally the catheter will have to be removed. Infections resulting in bacteremia from Staphylococcus aureus require removal of the catheter and antibiotics. If the catheter is removed without giving antibiotics, 38% of people may still develop endocarditis.[9]
In a clinical practice guideline, the American Centers for Disease Control and Prevention recommends against routine culturing of central venous lines upon their removal.[10] The guideline makes several other recommendations to prevent line infections.[10]
To prevent infection, stringent cleaning of the catheter insertion site is advised. Povidone-iodine solution is often used for such cleaning, but chlorhexidine appears to be twice as effective as iodine.[11] Routine replacement of lines makes no difference in preventing infection.[12]
Thrombosis
CVCs are a risk factor for forming blood clots (venous thrombosis) including upper extremity deep vein thrombosis.[13][14] It is thought this risk stems from activation of clotting substances in the blood by trauma to the vein during placement.[15] The risk of blood clots is higher in a person with cancer, as cancer is also a risk factor for blood clots. Anti-clotting drugs such as heparin and fondaparinux have been shown to decrease the incidence of blood clots, specifically deep vein thrombosis, in a person with cancer with central lines.[16] Additionally, studies suggest that short term use of CVCs in the subclavian vein is less likely to be associated with blood clots than CVCs placed in the femoral vein in non-cancer patients.[17]
Misplacement
CVC misplacement is more common when the anatomy of the person is different or difficult due to injury or past surgery.[15]
CVCs can be mistakenly placed in an artery during insertion (for example, the carotid artery or vertebral artery when placed in the neck or common femoral artery when placed in the groin). This error can be quickly identified by special tubing that can show the pressure of the catheter (arteries have a higher pressure than veins). In addition, sending blood samples for acidity, oxygen, and carbon dioxide content (pH, pO2, pCO2 respectively) can show the characteristics of an artery (higher pH/pO2, lower pCO2) or vein (lower pH/pO2, higher pCO2).[1]
During subclavian vein central line placement, the catheter can be accidentally pushed into the internal jugular vein on the same side instead of the superior vena cava. A chest x-ray is performed after insertion to rule out this possibility.[18] The tip of the catheter can also be misdirected into the contralateral (opposite side) subclavian vein in the neck, rather than into the superior vena cava.
Other complications
Rarely, small amounts of air are sucked into the vein as a result of the negative Intra-thoracic pressure and insertion technique. Valved insertion devices can reduce this risk. An air embolism is the result of air bubbles obstructing a blood vessel. Air embolisms are a very infrequent complication related to central venous catheter removal. The threat of air embolism is minimized by proper CVC removal with Trendelenburg positioning.[19]
Hemorrhage (profuse bleeding) and formation of a hematoma (bruise) is slightly more common in jugular venous lines than in others.[7]
Uncommonly, the vein can fuse with the artery after being damaged by insertion of the catheter. Ultrasound use is efficient at preventing this complication.[1]
Insertion
Before insertion, the patient is first assessed by reviewing relevant labs and indication for CVC placement, in order to minimize risks and complications of the procedure. Next, the area of skin over the planned insertion site is cleaned. A local anesthetic is applied if necessary. The location of the vein is identified by landmarks or with the use of a small ultrasound device. A hollow needle is advanced through the skin until blood is aspirated. The color of the blood and the rate of its flow help distinguish it from arterial blood (suggesting that an artery has been accidentally punctured). Within North American and Europe, ultrasound use now represents the gold standard for central venous access and skills, with diminishing use of landmark techniques.[20][21] Recent evidence shows that ultrasound-guidance for subclavian vein catheterization leads to a reduction in adverse events.[22]
The line is then inserted using the Seldinger technique: a blunt guidewire is passed through the needle, then the needle is removed. A dilating device may be passed over the guidewire to expand the tract. Finally, the central line itself is then passed over the guidewire, which is then removed. All the lumens of the line are aspirated (to ensure that they are all positioned inside the vein) and flushed with either saline or heparin.[1] A chest X-ray may be performed afterwards to confirm that the line is positioned inside the superior vena cava and no pneumothorax was caused inadvertently. On anteroposterior X-rays, a catheter tip between 55 and 29 mm below the level of the carina is regarded as acceptable placement.[23] Electromagnetic tracking can be used to verify tip placement and provide guidance during insertion, obviating the need for the X-ray afterwards.
 A central venous catheter secured to the skin with suture
A central venous catheter secured to the skin with suture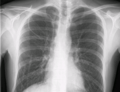 Chest x-ray with catheter in the right subclavian vein
Chest x-ray with catheter in the right subclavian vein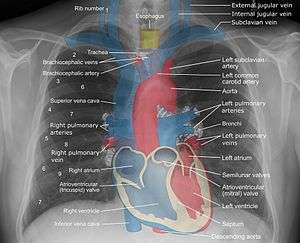 The outline of superior vena cava on a chest X-ray is labeled at left.
The outline of superior vena cava on a chest X-ray is labeled at left.
Types
There are several types of central venous catheters:[24]
Non-tunneled vs. tunneled catheters
Non-tunneled catheters are fixed in place at the site of insertion, with the catheter and attachments protruding directly. Commonly used non-tunneled catheters include Quinton catheters.
Tunneled catheters are passed under the skin from the insertion site to a separate exit site. The catheter and its attachments emerge from underneath the skin. The exit site is typically located in the chest, making the access ports less visible than catheters that protrude directly from the neck. Passing the catheter under the skin helps to prevent infection and provides stability. Commonly used tunneled catheters include Hickman catheters and Groshong catheters.
Implanted port
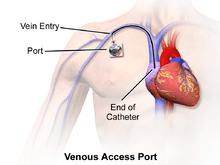
A port is similar to a tunneled catheter but is left entirely under the skin. Medicines are injected through the skin into the catheter. Some implanted ports contain a small reservoir that can be refilled in the same way. After being filled, the reservoir slowly releases the medicine into the bloodstream. An implanted port is less obvious than a tunneled catheter and requires little daily care. It has less impact on a person's activities than a PICC line or a tunneled catheter. Surgically implanted infusion ports are placed below the clavicle (infraclavicular fossa), with the catheter threaded into the heart (right atrium) through a large vein. Once implanted, the port is accessed via noncoring "Huber" needles inserted through the skin. The health care provider may need to use topical anesthetic before accessing the port. Ports can be used for medications, chemotherapy, and blood. As ports are located completely under the skin, they are easier to maintain and have a lower risk of infection than CVC or PICC catheters.[1]
Ports are typically used on patients requiring only occasional venous access over a long duration course of therapy. Since the port must be accessed using a needle, if venous access is required on a frequent basis a catheter having external access is more commonly used.[1]
PICC line
A peripherally inserted central catheter, or PICC line (pronounced "pick"), is a central venous catheter inserted into a vein in the arm (via the basilic or cephalic veins) rather than a vein in the neck or chest. The tip is positioned in the superior vena cava.[1]
Technical description

Depending on use, catheters may have a single lumen (a "monoluminal catheter") or multiple lumens. A catheter with two lumens is "biluminal", three "triluminal". Up to 4 or 5 lumens may be used, allowing multiple drug infusions to be delivered and monitored simultaneously.
The catheter is held in place by an adhesive dressing, suture, or staple which is covered by an occlusive dressing. Regular flushing with saline or a heparin-containing solution keeps the line open and prevents blood clots. There is no evidence that heparin is better than saline at preventing blood clots.[25] Certain lines are impregnated with antibiotics, silver-containing substances (specifically silver sulfadiazine) and/or chlorhexidine to reduce infection risk.[26]
Specific types of long-term central lines are the Hickman catheters, which require clamps to make sure that the valve is closed, and Groshong catheters, which have a valve that opens as fluid is withdrawn or infused and remains closed when not in use. Hickman lines also have a "cuff" under the skin, to prevent bacterial migration. The cuff also causes tissue ingrowth into the device for long term securement.
See also
References
- 1 2 3 4 5 6 7 8 McKean, Sylvia; Ross, John; Dressler, Daniel; Brotman, Daniel; Ginsburg, Jeffrey (2012). Principles and practice of hospital medicine. New York: McGraw-Hill. ISBN 978-0071603898.
- ↑ Ge, Xiaoli (2012). "Central venous access sites for the prevention of venous thrombosis, stenosis and infection.". The Cochrane Library. doi:10.1002/14651858.CD004084.pub3.
- ↑ Weinstein, R.A. (2015). Infections Acquired in Health Care Facilities. New York, NY: McGraw-Hill. ISBN 0071802150.
- ↑ National Institute for Health and Clinical Excellence (September 2002). "Technology appraisal: the clinical effectiveness and cost effectiveness of ultrasonic locating devices for the placement of central venous lines". Retrieved 2008-06-01.
- ↑ Murray E.C., Deighan C., Geddes C., Thomson P.C. (2014). Taurolidine-citrate-heparin catheter lock solution reduces staphylococcal bacteraemia rates in haemodialysis patients. QJMed2014
- ↑ "A National Campaign to Scale Up and Spread CUSP-CLABSI: Interviews with James B. Battles and Stephen Hines". Agency for Healthcare Research and Quality. 2012-05-30. Retrieved 2013-08-27.
- 1 2 Parienti JJ; Thirion M; Mégarbane B; et al. (May 2008). "Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial". JAMA. 299 (20): 2413–22. PMID 18505951. doi:10.1001/jama.299.20.2413.
- ↑ Safdar N, Fine JP, Maki DG (2005). "Meta-analysis: methods for diagnosing intravascular device-related bloodstream infection". Ann. Intern. Med. 142 (6): 451–66. PMID 15767623. doi:10.7326/0003-4819-142-6-200503150-00011.
- ↑ Watanakunakorn C, Baird IM (August 1977). "Staphylococcus aureus bacteremia and endocarditis associated with a removable infected intravenous device". Am. J. Med. 63 (2): 253–6. PMID 888847. doi:10.1016/0002-9343(77)90239-X.
- 1 2 O'Grady NP; Alexander M; Dellinger EP; et al. (2002). "Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention". MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 51 (RR–10): 1–29. PMID 12233868.
- ↑ Mimoz O; Villeminey S; Ragot S; et al. (October 2007). "Chlorhexidine-based antiseptic solution vs alcohol-based povidone-iodine for central venous catheter care". Arch. Intern. Med. 167 (19): 2066–72. PMID 17954800. doi:10.1001/archinte.167.19.2066.
- ↑ Cobb DK; High KP; Sawyer RG; et al. (1992). "A controlled trial of scheduled replacement of central venous and pulmonary-artery catheters". N. Engl. J. Med. 327 (15): 1062–8. PMID 1522842. doi:10.1056/NEJM199210083271505.
- ↑ Rosendaal, F. R.; Reitsma, P. H. (July 2009). "Genetics of venous thrombosis". Journal of Thrombosis and Haemostasis. 7 suppl 1: 301–304. PMID 19630821. doi:10.1111/j.1538-7836.2009.03394.x
 .
. - ↑ Lee JA, Zierler BK, Zierler RE (2012). "The risk factors and clinical outcomes of upper extremity deep vein thrombosis". Vasc Endovascular Surg. 46 (2): 139–44. PMID 22328450. doi:10.1177/1538574411432145.
- 1 2 Polderman, Kees H.; Girbes, Armand R. (2001-12-04). "Central venous catheter use". Intensive Care Medicine. 28 (1): 1–17. ISSN 0342-4642. doi:10.1007/s00134-001-1154-9.
- ↑ Akl, Elie A; Ramly, Elie P; Kahale, Lara A; Yosuico, Victor E D; Barba, Maddalena; Sperati, Francesca; Cook, Deborah; Schünemann, Holger (2014-10-15). Anticoagulation for people with cancer and central venous catheters. John Wiley & Sons, Ltd. ISSN 1465-1858. doi:10.1002/14651858.cd006468.pub5.
- ↑ Ge, Xiaoli; Cavallazzi, Rodrigo; Li, Chunbo; Pan, Shu Ming; Wang, Ying Wei; Wang, Fei-Long (2012-03-14). Central venous access sites for the prevention of venous thrombosis, stenosis and infection. John Wiley & Sons, Ltd. ISSN 1465-1858. doi:10.1002/14651858.cd004084.pub3.
- ↑ "ABerrant locations and complications in initial placement of subclavian vein catheters". Archives of Surgery. 119 (3): 293–295. 1984-03-01. ISSN 0004-0010. doi:10.1001/archsurg.1984.01390150035009.
- ↑ Bartolini, Luca (2015). "Pearls & Oy-sters: Cerebral venous air embolism after central catheter removal". Neurology. 84: e94–e96. PMID 25825470. doi:10.1212/WNL.0000000000001414.
- ↑ O'Leary, R; Bodenham, A (2011). "Future directions for ultrasound-guided central venous access.". European Journal of Anaesthesiology. 28 (5): 327–8. PMID 21487264. doi:10.1097/EJA.0b013e328343b148.
- ↑ Bodenham, A (2011). "Reducing major procedural complications from central venous catheterisation". Anaesthesia. 66 (1): 6–9. PMID 21198502. doi:10.1111/j.1365-2044.2010.06583.x.
- ↑ Lalu, M. M.; Fayad, A; Ahmed, O; Bryson, G. L.; Fergusson, D. A.; Barron, C. C.; Sullivan, P; Thompson, C; Canadian Perioperative Anesthesia Clinical Trials Group (2015). "Ultrasound-Guided Subclavian Vein Catheterization: A Systematic Review and Metaanalysis". Critical Care Medicine. 43: 1498–507. PMID 25803646. doi:10.1097/CCM.0000000000000973.
- ↑ Venugopal, AchuthanNair; Koshy, RachelCherian; Koshy, SumodM (2013). "Role of chest X-ray in citing central venous catheter tip: A few case reports with a brief review of the literature". Journal of Anaesthesiology Clinical Pharmacology. 29 (3): 397. ISSN 0970-9185. doi:10.4103/0970-9185.117114.
- ↑ Central Venous Catheters - Topic Overview from WebMD
- ↑ López-Briz, E; Ruiz Garcia, V; Cabello, JB; Bort-Marti, S; Carbonell Sanchis, R; Burls, A (Oct 8, 2014). "Heparin versus 0.9% sodium chloride intermittent flushing for prevention of occlusion in central venous catheters in adults.". The Cochrane database of systematic reviews. 10: CD008462. PMID 25300172. doi:10.1002/14651858.CD008462.pub2.
- ↑ Schiffer, Charles A.; Mangu, Pamela B.; Wade, James C.; Camp-Sorrell, Dawn; Cope, Diane G.; El-Rayes, Bassel F.; Gorman, Mark; Ligibel, Jennifer; Mansfield, Paul (2013-04-01). "Central Venous Catheter Care for the Patient With Cancer: American Society of Clinical Oncology Clinical Practice Guideline". Journal of Clinical Oncology. 31 (10): 1357–1370. ISSN 0732-183X. PMID 23460705. doi:10.1200/JCO.2012.45.5733.
External links
| Wikimedia Commons has media related to Venous catheters. |
- Central Venous Catheter Placement & Pulmonary Artery Catheter - Vìdeo Dailymotion (without ultrasound guidance)
- Video tutorial on how to start central venous lines in various locations
- Central venous line care, comparison, indications, complications and uses
