Cavernous hemangioma
| Cavernous hemangioma | |
|---|---|
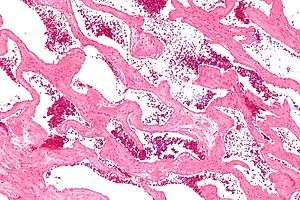 | |
| Micrograph of a cavernous liver hemangioma. H&E stain. | |
| Classification and external resources |
Cavernous hemangioma, also called cavernous angioma, cavernoma, or cerebral cavernous malformation (CCM) (when referring to presence in the brain)[1] is a type of blood vessel malformation or hemangioma, where a collection of dilated blood vessels form a benign tumor. Because of this malformation, blood flow through the cavities, or caverns, is slow. Additionally, the cells that form the vessels do not form the necessary junctions with surrounding cells. Also, the structural support from the smooth muscle is hindered, causing leakage into the surrounding tissue. It is the leakage of blood, known as a hemorrhage from these vessels that causes a variety of symptoms known to be associated with this disease.
Cause
Cavernous hemangiomas can arise nearly anywhere in the body where there are blood vessels and are considered to be benign tumours. They are often described as raspberry-like because of the bubble-like caverns. Unlike the capillary hemangiomas, cavernous ones can be disfiguring and do not tend to regress. Most cases of cavernomas are congenital, however they can develop over the course of a lifetime.[2] While there is no definitive cause, research shows that genetic mutations result in the onset. Congenital hemangiomas that appear on the skin are known as either vascular or red birthmarks.
Genetics
Familial cerebral cavernous malformations are known to occur. The mutations may be inherited in an autosomal dominant fashion or occur sporadically. Overall familial disease is responsible for one third to one half of cases.[3] In the US approximately 50% of Hispanic patients with cerebral cavernous malformations have a familial form: in contrast in this occurs in only 10 to 20% of Caucasians.[4] The reason for this difference is not presently known.
Several genes - K-Rev interaction trapped 1 (ССМ1), Malcavernin (CCM2) and Programmed cell death protein 10 (ССМ3) - have been identified as having mutations thought to be related to these lesions.[5][6][7] These genes are located at 7q21.2 (chromosome 7 long arm), 7q13 (chromosome 7 long arm) and 3q25.2-q27 (chromosome 3 long arm) respectively. These lesions are further discussed in the Online Mendelian Inheritance in Man site - the reference numbers are OMIM 116860, OMIM 603284 and OMIM 603285 respectively.
Diagnosis
Gradient-Echo T2WI magnetic resonance imaging (MRI) is most sensitive method for diagnosing cavernous hemangiomas.[8] MRI is such a powerful tool for diagnosis, it has led to an increase in diagnosis of cavernous hemangiomas since the technology's advent in the 1980s.[9] The radiographic appearance is most commonly described as "popcorn" or "mulberry"-shaped.[10] Computed tomography (CT) scanning is not a sensitive or specific method for diagnosing cavernous hemangiomas.[11] Angiography is typically not necessary, unless it is required to rule out other diagnoses. Additionally, biopsies can be obtained from tumor tissue for examination under a microscope. It is essential to diagnose cavernous hemangioma because treatments for this benign tumor are less aggressive than that of cancerous tumors, such as angiosarcoma. However, since MRI appearance is practically pathognomonic, biopsy is rarely needed for verification.[11]
Variations
Cerebral cavernous malformations
Cavernous hemangiomas located on the brain are referred to as cerebral cavernomas or more usually as cerebral cavernous malformations (CCMs)[1] and can be found in the white matter, but often abut the cerebral cortex. When they contact the cortex, they can represent a potential seizure focus for the patient. Unlike other cavernous hemangiomas, there is no tissue within the malformation and its borders are not encapsulated. Therefore, they can change in size and number over time.[2]
Liver cavernous hemangioma
Cavernous hemangiomas are the most common benign tumors of the liver.[12] Usually one tumor exists, but multiple lesions can occur in the left or right lobe of the liver in 40% of patients.[13] Their sizes can range from a few millimeters to 20 centimetres. Those over 5 cm are often referred to as giant hemangiomas.[13]
Eye cavernous hemangioma
In the eye, it is known as orbital cavernous hemangioma and is found in women more frequently than men, most commonly between the ages of 20-40.[14] This neoplasm is usually located within the muscle cone, which is lateral to the optic nerve. It is not usually treated unless the patient is symptomatic. Visual impairment happens when the optic nerve is compressed or the extraocular muscles are surrounded.
Epidemiology
The true incidence of cavernous hemangiomas is difficult to estimate because they are frequently misdiagnosed as other venous malformations.[15] Cavernous hemangiomas of the brain and spinal cord (cerebral cavernous hemangiomas (malformations) (CCM)), can appear at all ages but usually occur in the third to fourth decade of a person's life with no sexual preference. In fact, CCM is present in 0.5% of the population. However, approximately 40% of those with malformations have symptoms. Asymptomatic individuals are usually individuals that developed the malformation sporadically, while symptomatic individuals usually have inherited the genetic mutation.[2] The majority of diagnoses of CCM are in adults; however, 25% of cases of CCM are children.[2] Approximately 5% of adults have liver hemangiomas in the United States, but most are asymptomatic.[16] Liver hemangiomas usually occur between the ages of 30-50 and more commonly in women.[17] Cases of infantile liver cavernomas are extremely rare. Cavernous hemangioma of the eye is more prevalent in women than men and between the ages of 20-40.[14]
Mechanism
There are several known causes for cavernous hemangiomas, but some cases are still unknown. Radiation treatment used for other medical conditions has been suggested to cause cavernous malformation in some patients.[9] Hemangioma tumors are a result of rapid proliferation of endothelial cells and pericytic hyperplasia, or the enlargement of tissue as a result of abnormal cell division pericytes. The pathogenesis of hemangioma is still not understood. It has been suggested that growth factors and hormonal influences contribute to the abnormal cell proliferation. Cavernous liver hemangiomas are more commonly diagnosed in women who have been pregnant.[17] As a result of this, it is believed that estrogen levels may play a role in the incidence of liver cavernomas.
Genetic studies show that specific gene mutations or deletions are causes for the disease. The genes identified for cerebral cavernous hemangiomas (or malformations), are CCM1 (also KRIT1), CCM2 (also MGC4607, malcavernin) and CCM3 (also PDCD10). The loss of function of these genes is believed to be responsible for cerebral cavernous malformations.[18] Furthermore, it is also believed that a "second hit mutation" is necessary for the onset of the disease. This means that having a mutation in one of the two genes present on a chromosome is not enough to cause the cavernous malformation, but mutation of both alleles would cause the malformation. Additionally, research on hemangiomas in general has shown that loss of heterozygosity is common in tissue where hemangioma develops.[19] This would confirm that more than a single allele mutation is needed for the abnormal cell proliferation. KRIT1 has been shown to act as a transcription factor in the development of arterial blood vessels in mice. CCM2 has overlapping structure with CCM1 (KRIT1) and acts as a scaffolding protein when expressed. Both genes are involved with MAP3K3 and thus appear to be a part of the same pathway.

CCM2 has been shown to cause embryonic death in mice. Lastly, the CCM3 gene has been shown to have similar expression to CCM1 and CCM2, suggesting a link in its functionality. Currently, no experiments have determined its exact function.[20] The lack of function of these genes in control of a proliferative signaling pathway would result in uncontrolled proliferation and the development of a tumor.
Symptoms
Most people with cavernous hemangioma are asymptomatic.[21]
Cerebral
Major
- Seizures due to the compression of the brain tissue or hemorrhaging of angioma scarring surrounding tissue
- Stroke or intraparenchymal hemorrhage
- Double vision or other vision problems
- Language difficulties can arise
- Memory loss or attention problems
- Incidental hydrocephalus
Minor
- Headaches
- Weakness or numbness in the arms or legs
- Balancing problems
Liver
Usually liver cavernoma patients are asymptomatic.[13][17]
Major
- Pain in the upper right abdomen
Minor
- Feeling full after eating only a small amount of food
- Lack of appetite
- Nausea
- Vomiting
Eye
In cavernous hemangioma of the eye, patients report an onset of symptoms from 6 months to 2 years.[14]
Major
- As the tumor grows and involves the extraocular muscles and optic nerve, patients report double vision and decreased vision
Minor
- Painless, progressive proptosis
Treatment
Benign tumors may not require treatment but may need to be monitored for any change in the growth. Growth of the tumors in the nose, lips, or eyelids can be treated with steroid drugs to slow its progress. Steroids can be taken orally or injected directly into the tumor. Applying pressure to the tumor can also be used to minimize swelling at the site of the hemangioma. A procedure that uses small particles to close off the blood supply is known as sclerotherapy. This allows for tumor shrinkage and less pain. It is possible for the tumor to regrow its blood supply after the procedure has been done.[22] If the lesion caused by the cavernous hemangioma is destroying healthy tissue around it or if the patient is experiencing major symptoms, then surgery can be used to remove the tumor piecemeal.[11] A common complication of the surgery is hemorrhage and the loss of blood. There is also the possibility of the hemangioma reoccurring after its removal.[22] Additionally, the risk of a stroke or death is also possible.[23]
Prognosis
A few studies have worked on providing details related to the outlook of disease progression. Two studies show that each year 0.5% of people who have never had bleeding from their brain cavernoma, but had symptoms of seizures, were affected by bleeding.[23] In contrast, patients who have had bleeding from their brain cavernoma in the past had a higher risk of being affected by subsequent bleeding. The statistics for this are very broad, ranging from 4%-23% a year.[23] Additional studies suggest that women and patients under the age of 40 are at higher risk of bleeding, but similar conducted studies did not reach the same conclusion.[23] However, when cavernous hemangiomas are completely excised, there is very little risk of growth or rebleeding.[24] In terms of life expectancy, not enough data has been collected on patients with this malformation in order to provide a representative statistical analysis.[9]
Research
In the treatment of a brain cavernous hemangioma, neurosurgery is usually the treatment chosen.[25] Research needs to be conducted on the efficacy of treatment with stereotactic radiation therapy, especially on the long-term.[26] However, radiotherapy is still being studied as a form of treatment if neurosurgery is too dangerous due the location of the cavernoma. Genetic researchers are still working on determining the cause of the illness and the mechanism behind blood vessel formation.[23] Clinical trials are being conducted to better assess when it is appropriate to treat a patient with this malformation and with what treatment method.[9] Additionally, long term studies are being conducted because there is no information related to the long-term outlook of patients with cavernoma. A registry exists known as The International Cavernous Angioma Patient Registry collects information from patients diagnosed with cavernoma in order to facilitate discovery of non-invasive treatments.[23]
References
- 1 2 Algra, Ale; Rinkel, Gabriël J E (February 2016). "Prognosis of cerebral cavernomas: on to treatment decisions". The Lancet Neurology. 15 (2): 129–130. doi:10.1016/S1474-4422(15)00340-3.
- 1 2 3 4 Cavernous Malformation. 2014. http://www.webmd.com/brain/cavernous-malformation.
- ↑ Mindea SA, Yang BP, Shenkar R, Bendok B, Batjer HH, Awad IA (2006) Cerebral cavernous malformations: clinical insights from genetic studies. Neurosurg Focus ;21(1):e1.
- ↑ Dashti SR, Hoffer A, Hu YC, Selman WR (2005) Molecular genetics of familial cerebral cavernous malformations. Neurosurg Focus 21(1):e2
- ↑ Pagenstecher A, Stahl S, Sure U, Felbor U (Mar 2009). "A two-hit mechanism causes cerebral cavernous malformations: complete inactivation of CCM1, CCM2 or CCM3 in affected endothelial cells". Human Molecular Genetics. 18 (5): 911–8. PMC 2640205
 . PMID 19088124. doi:10.1093/hmg/ddn420.
. PMID 19088124. doi:10.1093/hmg/ddn420. - ↑ Bergametti F, Denier C, Labauge P, Arnoult M, Boetto S, Clanet M, Coubes P, Echenne B, Ibrahim R, Irthum B, Jacquet G, Lonjon M, Moreau JJ, Neau JP, Parker F, Tremoulet M, Tournier-Lasserve E (Jan 2005). "Mutations within the programmed cell death 10 gene cause cerebral cavernous malformations". American Journal of Human Genetics. 76 (1): 42–51. PMC 1196432
 . PMID 15543491. doi:10.1086/426952.
. PMID 15543491. doi:10.1086/426952. - ↑ "Entrez Gene: PDCD10 programmed cell death 10".
- ↑ Lehnhardt, Fritz-Georg; Smekal, Ulrich von; Rückriem, Benedikt; Stenzel, Werner; Neveling, Michael; Heiss, Wolf-Dieter; Jacobs, Andreas H. (2005-04-01). "Value of Gradient-Echo Magnetic Resonance Imaging in the Diagnosis of Familial Cerebral Cavernous Malformation". Archives of Neurology. 62 (4). ISSN 0003-9942. doi:10.1001/archneur.62.4.653.
- 1 2 3 4 Rustam Al-Shahi Salman. Cavernoma Alliance UK. Symptomatic brain cavernomas. https://www.cavernoma.org.uk/wp-content/uploads/2015/03/Symptomatic-booklet.pdf
- ↑ Wang, Chung-cheng; Liu, Ali; Zhang, Jun-ting; Sun, Bo; Zhao, Yuan-li. "Surgical management of brain-stem cavernous malformations: report of 137 cases". Surgical Neurology. 59 (6): 444–454. doi:10.1016/s0090-3019(03)00187-3.
- 1 2 3 Greenberg., Mark S. (2010-01-01). Handbook of neurosurgery. Greenberg Graphics. ISBN 9781604063264. OCLC 892183792.
- ↑ John T. G.; et al. (1994). "Superior staging of liver tumors with laparoscopy and laparoscopic ultrasound". Ann. Surg. 220 (6): 711–719. PMC 1234471
 . PMID 7986136. doi:10.1097/00000658-199412000-00002.
. PMID 7986136. doi:10.1097/00000658-199412000-00002. - 1 2 3 Curry M. P., MD; Chopra S, MD. Hepatic Hemangioma, 2014. http://www.uptodate.com/contents/hepatic-hemangioma?source=search_result&search=hepatic+hemangioma&selectedTitle=2~46
- 1 2 3 Pargament J., MD; Nerad J., MD. Cavernous hemangioma. http://eyewiki.aao.org/Cavernous_hemangioma
- ↑ Neurovascular Surgery Brain Aneurysm & AVM Center. Cavernous malformations. http://neurosurgery.mgh.harvard.edu/neurovascular/v-w-94-2.htm
- ↑ American Liver Foundation. Benign Liver Tumors. 2011. http://www.liverfoundation.org/abouttheliver/info/benigntumors/
- 1 2 3 MayoClinic. Liver Hemangioma. 2013. http://www.mayoclinic.org/diseases-conditions/liver-hemangioma/basics/risk-factors/con-20034197
- ↑ Mouchtouris, Nikolaos; Chalouhi, Nohra; Chitale, Ameet; Starke, Robert M.; Tjoumakaris, Stavropoula I.; Rosenwasser, Robert H.; Jabbour, Pascal M. (2015). "Management of Cerebral Cavernous Malformations: From Diagnosis to Treatment". The Scientific World Journal. 2015: 1–8. doi:10.1155/2015/808314.
- ↑ Marchuk D. A. (2001). "Pathogenesis of hemangioma". J Clin Invest. 107 (6): 665–666. doi:10.1172/jci12470.
- ↑ Mattassi R., Loose D. A., Vaghi M. Hemangiomas and Vascular Malformations. Springer-Verlag Italia 2009. http://download.springer.com/static/pdf/512/bok%253A978-88-470-0569-3.pdf?auth66=1398881485_a65ad7e1e0ca732b64c590de9fdf46fc&ext=.pdf
- ↑ Northwestern memorial Hospital Pediatric and Adolescent Neurovascular Disease and Stroke. 2012. http://www.nmh.org/nm/cavernoma-about
- 1 2 American Academy of Orthopedic Surgeons. Hemangioma. 2012. http://orthoinfo.aaos.org/topic.cfm?topic=A00630
- 1 2 3 4 5 6 NHS. Cavernoma. 2012. http://www.nhs.uk/conditions/cavernoma/Pages/Introduction.aspx
- ↑ 1944-, Spetzler, Robert F. (Robert Friedrich),; Yashar,, Kalani,; Peter,, Nakaji,. Neurovascular surgery. ISBN 9781604067590. OCLC 967842929.
- ↑ Poorthuis, MHF; Klijn, CJM; Algra, A; Rinkel, GJE; Al-Shahi Salman, R (2014). "Treatment of cerebral cavernous malformations: a systematic review and meta-regression analysis". Journal of Neurology, Neurosurgery, and Psychiatry. 85: 1319–1323. doi:10.1136/jnnp-2013-307349.
- ↑ Poorthuis, M; Samarasekera, N; Kontoh, K; Stuart, I; Cope, B; Kitchen, N; Al-Shahi Salman, R (2013). "Comparative studies of the diagnosis and treatment of cerebral cavernous malformations in adults: systematic review". Acta Neurochirurgica. 155: 643–649. doi:10.1007/s00701-013-1621-4.
External links
- Angioma Alliance, a non-profit organization providing information for patients and medical professionals.
- Robinson JR Jr; Awad IA; Little JR (1991). "Natural history of the cavernous angioma". J Neurosurg. 75: 709–714. doi:10.3171/jns.1991.75.5.0709.
- Curling OD Jr; Kelly DL Jr; Elster AD; et al. (1991). "An analysis of the natural history of cavernous angiomas". J Neurosurg. 75: 702–708.