Calcium pyrophosphate dihydrate crystal deposition disease
| Calcium pyrophosphate dihydrate disease | |
|---|---|
 | |
| Micrograph showing crystal deposition in an intervertebral disc. H&E stain. | |
| Classification and external resources | |
| Specialty | rheumatology |
| ICD-10 | M11.1-M11.2 |
| ICD-9-CM | [712.3 275.49 [712.3]] |
| OMIM | 600668 118600 |
| DiseasesDB | 10832 DDB 30784 |
| MedlinePlus | 000421 |
| eMedicine | med/1938 radio/125 orthoped/382 emerg/221 |
| Patient UK | Calcium pyrophosphate dihydrate crystal deposition disease |
| MeSH | D002805 |
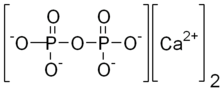
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy is a rheumatologic disorder with varied symptoms and signs arising from the resultant accumulation of crystals of calcium pyrophosphate dihydrate in the connective tissues. The alternative names emphasize particular aspects of the clinical or radiographic findings. The knee joint is the most commonly affected.[1]
Terminology
Calcium pyrophosphate dihydrate crystals are associated with a range of clinical syndromes, which have been given various names, based upon which clinical symptoms or radiographic findings are most prominent.[2] A task force of the European League Against Rheumatism (EULAR) made recommendations on preferred terminology.[3] Accordingly, calcium pyrophosphate deposition (CPPD) is an umbrella term for the various clinical subsets, whose naming reflects an emphasis on particular features. For example, pseudogout refers to the acute symptoms of joint inflammation or synovitis: red, tender, and swollen joints that may resemble gouty arthritis (a similar condition in which monosodium urate crystals are deposited within the joints). Chondrocalcinosis,[1][4] on the other hand, refers to the radiographic evidence of calcification in hyaline and/or fibrocartilage. "Osteoarthritis (OA) with CPPD" reflects a situation where osteoarthritis features are the most apparent. Pyrophosphate arthropathy refers to several of these situations.[5]
Cause
The exact cause of CPPD is unknown, although increased breakdown of adenosine triphosphate (ATP; the molecule used as energy currency in all living things), which results in increased pyrophosphate levels in joints, is thought to be one reason why crystals may develop.[4]
Familial forms are rare.[3] One genetic study found an association between CPPD and a region of chromosome 8q.[6]
The gene ANKH is involved in crystal-related inflammatory reactions and inorganic phosphate transport.[4][7]
Signs and symptoms
The disorder is more common in older adults.[7] The disease is often occult until crystal deposits are coincidentally detected and diagnosed by a pathologist in various orthopedic specimens. It may be asymptomatic, or it can be associated with osteoarthritis, or it can present as an acute or chronic inflammatory arthritis that causes pain in one or more joints.[4][7] The white blood cell count is often raised.[4]
The arthritis is usually polyarticular (i.e., it leads to an inflammation of several joints in the body), although it may begin as monoarticular (i.e., confined to just one joint).[8] CPPD crystals tend to form within articular tissues.[8] In theory, any joint may be affected, but statistics show that the knees are the most commonly affected joints, as well as wrists and hips.[4] In rare cases, pseudogout may affect the spinal canal and cause damage to the spinal cord.[9]
In many instances, patients may also have signs of carpal tunnel syndrome.[4] This condition can also be associated with Milwaukee shoulder syndrome.
Diagnosis
Two elements are considered: radiology and joint fluid analysis.

Radiology has a large role to play in finding chondrocalcinosis, with radiographs, CT scans, MRIs, US, and nuclear medicine all having a part.[1] CT scans and MRIs show calcific masses (usually within the ligamentum flavum or joint capsule), however radiography is more successful.[1] At ultrasound, chondrocalcinosis may be depicted as echogenic foci with no acoustic shadow within the hyaline cartilage.[10] As with most conditions, CPPD can present with similarity to other diseases such as ankylosing spondylitis and gout.[1][4]

Arthrocentesis, or removing synovial fluid from the affected joint, is performed to test the synovial fluid for the calcium pyrophosphate crystals that are present in CPPD. When stained with H&E stain, calcium pyrophosphate crystals appears deeply blue ("basophilic").[11][12] However, CPP crystals are much better known for their rhomboid shape and weak positive birefringence on polarized light microscopy, and this method remains the most reliable method of identifying the crystals under the microscope.[13] However, even this method suffers from poor sensitivity, specificity, and inter-operator agreement.[13]
These two modalities currently define CPPD disease but lack diagnostic accuracy,[2] and are potentially epiphenomenological.
Treatment
Because any medication that could reduce the inflammation of CPPD bears a risk of causing organ damage, treatment is not advised if the condition is not causing pain.[4] For acute pseudogout, treatments include intra-articular corticosteroid injection, systemic corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), or, on occasion, high-dose colchicine.[4] In general, NSAIDs are administered in low doses to help prevent CPPD. However, if an acute attack is already occurring, higher doses are administered.[4] If nothing else works, hydroxychloroquine or methotrexate may provide relief.[14] Research into surgical removal of calcifications is underway, however this still remains an experimental procedure.[4]
Epidemiology
CPPD affects people of all cultures and ethnic origins, and, in the United States, around 50% of the population over 85 years of age are affected.[4] It may cause considerable pain, but it is never fatal.[4] Women are at a slightly higher risk than men, with an estimated ratio of occurrence of 1.4:1.[4]
History
CPPD crystal deposition disease was originally described over 50 years ago.[2]
References
- 1 2 3 4 5 Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (radiology)
- 1 2 3 Rosenthal AK, Ryan LM. Crystal arthritis: Calcium pyrophosphate deposition—nothing 'pseudo' about it! Nat Rev Rheumatol. 2011 May;7(5):257-8. doi: 10.1038/nrrheum.2011.50 PMID 21532639
- 1 2 Zhang W, Doherty M, Bardin T, Barskova V, Guerne PA, Jansen TL, Leeb BF, Perez-Ruiz F, Pimentao J, Punzi L, Richette P, Sivera F, Uhlig T, Watt I, Pascual E. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011;70(4):563.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Rothschild, Bruce M Calcium Pyrophosphate Deposition Disease (rheumatology) at eMedicine
- ↑ Longmore, Murray; Ian Wilkinson; Tom Turmezei; Chee Kay Cheung (2007). Oxford Handbook of Clinical Medicine. Oxford. p. 841. ISBN 0-19-856837-1.
- ↑ Baldwin CT, Farrer LA, Adair R, Dharmavaram R, Jimenez S, Anderson L (March 1995). "Linkage of early-onset osteoarthritis and chondrocalcinosis to human chromosome 8q". Am. J. Hum. Genet. 56 (3): 692–7. PMC 1801178
 . PMID 7887424.
. PMID 7887424. - 1 2 3 Tsui FW (Apr 2012). "Genetics and mechanisms of crystal deposition in calcium pyrophosphate deposition disease". Curr Rheumatol Rep. 14 (2): 155–60. PMID 22198832. doi:10.1007/s11926-011-0230-6.
- 1 2 Wright GD, Doherty M (1997). "Calcium pyrophosphate crystal deposition is not always 'wear and tear' or aging". Ann. Rheum. Dis. 56 (10): 586–8. PMC 1752269
 . PMID 9389218. doi:10.1136/ard.56.10.586.
. PMID 9389218. doi:10.1136/ard.56.10.586. - ↑ Walid MS, Yelverton JC, Ajjan M, Grigorian AA (2008). "Pseudogout of the thoracic spine mimicking a tumor.". Russian Neurosurgery Online. 1 (20).
- ↑ Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013. Free chapter on acromioclavicular chondrocalcinosis is available at ShoulderUS.com
- ↑ Hosler, Greg. "calcinosis_cutis_2_060122". Derm Atlas. Retrieved 13 March 2012.
- ↑ "Calcium Pyrophosphate Dihydrate Deposition Disease: Synovial Biopsy, Wrist". Rheumatology Image Bank. American College of Rheumatology. Retrieved 13 March 2012.
- 1 2 Dieppe, P.; Swan, A. (1 May 1999). "Identification of crystals in synovial fluid". Annals of the Rheumatic Diseases. 58 (5): 261–3. PMC 1752883
 . PMID 10225806. doi:10.1136/ard.58.5.261.
. PMID 10225806. doi:10.1136/ard.58.5.261. - ↑ Emkey GR, Reginato AM (2009). "All about gout and pseudogout". Journal of Musculoskeletal Medicine. 26 (10).