African trypanosomiasis
| African trypanosomiasis | |
|---|---|
| Synonyms | African sleeping sickness |
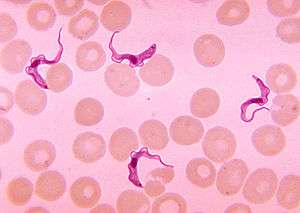 | |
| Trypanosoma forms in a blood smear | |
| Specialty | Infectious disease |
| Symptoms | Fevers, headaches, itchiness, joint pains[1] |
| Usual onset | 1–3 weeks post exposure[2] |
| Causes | Trypanosoma brucei spread by tsetse flies[1] |
| Diagnostic method | Blood smear, lumbar puncture[2] |
| Medication | Pentamidine, suramin, eflornithine[1] |
| Frequency | 11,000[3] |
| Deaths | 3,500[4] |
African trypanosomiasis, also known as sleeping sickness, is an insect-borne parasitic disease of humans and other animals.[1] It is caused by protozoa of the species Trypanosoma brucei.[1] There are two types that infect humans, Trypanosoma brucei gambiense (TbG) and Trypanosoma brucei rhodesiense (TbR).[1] TbG causes over 98% of reported cases.[1] Both are usually transmitted by the bite of an infected tsetse fly and are most common in rural areas.[1]
Initially, in the first stage of the disease, there are fevers, headaches, itchiness, and joint pains.[1] This begins one to three weeks after the bite. Weeks to months later the second stage begins with confusion, poor coordination, numbness and trouble sleeping. Diagnosis is via finding the parasite in a blood smear or in the fluid of a lymph node. A lumbar puncture is often needed to tell the difference between first and second stage disease.[2]
Prevention of severe disease involves screening the population at risk with blood tests for TbG.[1] Treatment is easier when the disease is detected early and before neurological symptoms occur.[1] Treatment of the first stage is with the medications pentamidine or suramin.[1] Treatment of the second stage involves: eflornithine or a combination of nifurtimox and eflornithine for TbG.[2] While melarsoprol works for both stages, it is typically only used for TbR, due to serious side effects.[1] Without treatment it typically results in death.[1]
The disease occurs regularly in some regions of sub-Saharan Africa with the population at risk being about 70 million in 36 countries.[5] An estimated 11,000 people are currently infected with 2,800 new infections in 2015.[3][1] In 2015 it caused around 3,500 deaths, down from 34,000 in 1990.[4][6] More than 80% of these cases are in the Democratic Republic of the Congo.[1] Three major outbreaks have occurred in recent history: one from 1896 to 1906 primarily in Uganda and the Congo Basin and two in 1920 and 1970 in several African countries.[1] It is classified as a neglected tropical disease.[7] Other animals, such as cows, may carry the disease and become infected in which case it is known as animal trypanosomiasis.[1]
Signs and symptoms
African trypanosomiasis symptoms occur in two stages. The first stage, known as the hemolymphatic phase, is characterized by fever, headaches, joint pains, and itching. Fever is intermittent, with attacks lasting from a day to a week, separated by intervals of a few days to a month or longer. Invasion of the circulatory and lymphatic systems by the parasites is associated with severe swelling of lymph nodes, often to tremendous sizes. Winterbottom's sign, the tell-tale swollen lymph nodes along the back of the neck, may appear.[8] Occasionally, a chancre (red sore) will develop at the location of the tsetse fly bite. If left untreated, the disease overcomes the host's defenses and can cause more extensive damage, broadening symptoms to include anemia, endocrine, cardiac, and kidney dysfunctions.
The second phase of the disease, the neurological phase, begins when the parasite invades the central nervous system by passing through the blood–brain barrier. Disruption of the sleep cycle is a leading symptom of this stage and is the one that gave the disease the name 'sleeping sickness.' Infected individuals experience a disorganized and fragmented 24-hour rhythm of the sleep-wake cycle, resulting in daytime sleep episodes and nighttime periods of wakefulness.[8]
Other neurological symptoms include confusion, tremor, general muscle weakness, hemiparesis and paralysis of a limb. Parkinson-like movements might arise due to non-specific movement disorders and speech disorders. Individuals may also exhibit psychiatric symptoms such as irritability, psychotic reactions, aggressive behaviour, or apathy which can sometimes dominate the clinical diagnosis.[9] Without treatment, the disease is invariably fatal, with progressive mental deterioration leading to coma, systemic organ failure, and death. An untreated infection with T. b. rhodesiense will cause death within months[10] whereas an untreated infection with T. b. gambiense will cause death after several years.[11] Damage caused in the neurological phase is irreversible.[12]
Cause
Trypanosoma brucei
There are two subspecies of the parasite that are responsible for starting the disease in humans. Trypanosoma brucei gambiense causes the diseases in west and central Africa, whereas Trypanosoma brucei rhodesiense has a limited geographical range and is responsible for causing the disease in east and southern Africa. In addition, a third subspecies of the parasite known as Trypanosoma brucei brucei is responsible for affecting animals but not humans.[9]
Humans are the main reservoir for T. b. gambiense but this species can also be found in pigs and other animals. Wild game animals and cattle are the main reservoir of T. b. rhodesiense. These parasites primarily infect individuals in sub-Saharan Africa because that is where the vector (tsetse fly) is located. The two human forms of the disease also vary greatly in intensity. T. b. gambiense causes a chronic condition that can remain in a passive phase for months or years before symptoms emerge and the infection can last about 3 years before death occurs.[9]
T. b. rhodesiense is the acute form of the disease and death can occur within months since the symptoms emerge within weeks and it is more virulent and faster developing than T. b. gambiense. Furthermore, trypanosomes are surrounded by a coat that is composed of variant surface glycoproteins (VSG). These proteins act to protect the parasite from any lytic factors that are present in human plasma. The host's immune system recognizes the glycoproteins present on the coat of the parasite leading to the production of different antibodies (IgM and IgG).[9]
These antibodies will then act to destroy the parasites that circulate around the blood. However, from the several parasites present in the plasma, a small number of them will experience changes in their surface coats resulting in the formation of new VSGs. Thus, the antibodies produced by the immune system will no longer recognize the parasite leading to proliferation until new antibodies are created to combat the novel VSGs. Eventually the immune system will no longer be able to fight off the parasite due to the constant changes in VSGs and infection will arise.[9]
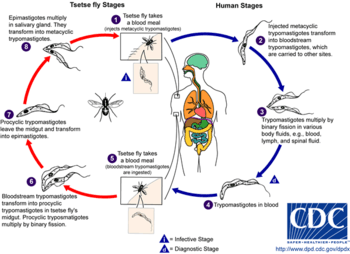
Vector
The tsetse fly (genus Glossina) is a large, brown, biting fly that serves as both a host and vector for the trypanosome parasites. While taking blood from a mammalian host, an infected tsetse fly injects metacyclic trypomastigotes into skin tissue. From the bite, parasites first enter the lymphatic system and then pass into the bloodstream. Inside the mammalian host, they transform into bloodstream trypomastigotes, and are carried to other sites throughout the body, reach other body fluids (e.g., lymph, spinal fluid), and continue to replicate by binary fission.
The entire life cycle of African trypanosomes is represented by extracellular stages. A tsetse fly becomes infected with bloodstream trypomastigotes when taking a blood meal on an infected mammalian host. In the fly's midgut, the parasites transform into procyclic trypomastigotes, multiply by binary fission, leave the midgut, and transform into epimastigotes. The epimastigotes reach the fly's salivary glands and continue multiplication by binary fission.
The entire life cycle of the fly takes about three weeks. In addition to the bite of the tsetse fly, the disease can be transmitted by:
- Mother-to-child infection: the trypanosome can sometimes cross the placenta and infect the fetus.[13]
- Laboratories: accidental infections, for example, through the handling of blood of an infected person and organ transplantation, although this is uncommon.
- Blood transfusion
- Sexual contact (This may be possible)[14]
Horse-flies (Tabanidae) and stable flies (Muscidae) possibly play a role in transmission of nagana (the animal form of sleeping sickness) and the human disease form.[15]
Mechanism
Tryptophol is a chemical compound that induces sleep in humans. It is produced by the trypanosomal parasite in sleeping sickness.[16]
Diagnosis
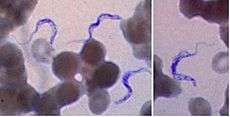
The gold standard for diagnosis is identification of trypanosomes in a patient sample by microscopic examination. Patient samples that can be used for diagnosis include chancre fluid, lymph node aspirates, blood, bone marrow, and, during the neurological stage, cerebrospinal fluid. Detection of trypanosome-specific antibodies can be used for diagnosis, but the sensitivity and specificity of these methods are too variable to be used alone for clinical diagnosis. Further, seroconversion occurs after the onset of clinical symptoms during a T. b. rhodesiense infection, so is of limited diagnostic use.
Trypanosomes can be detected from patient samples using two different preparations. A wet preparation can be used to look for the motile trypanosomes. Alternatively, a fixed (dried) smear can be stained using Giemsa's or Field's technique and examined under a microscope. Often, the parasite is in relatively low abundance in the sample, so techniques to concentrate the parasites can be used prior to microscopic examination. For blood samples, these include centrifugation followed by examination of the buffy coat; mini anion-exchange/centrifugation; and the quantitative buffy coat (QBC) technique. For other samples, such as spinal fluid, concentration techniques include centrifugation followed by examination of the sediment.
Three serological tests are also available for detection of the parasite: the micro-CATT, wb-CATT, and wb-LATEX. The first uses dried blood, while the other two use whole blood samples. A 2002 study found the wb-CATT to be the most efficient for diagnosis, while the wb-LATEX is a better exam for situations where greater sensitivity is required.[17]
Prevention
Currently there are few medically related prevention options for African Trypanosomiasis (i.e. no vaccine exists for immunity). Although the risk of infection from a tsetse fly bite is minor (estimated at less than 0.1%), the use of insect repellants, wearing long-sleeved clothing, avoiding tsetse-dense areas, implementing bush clearance methods and wild game culling are the best options to avoid infection available for local residents of affected areas.[18]
At the 25th ISCTRC (International Scientific Council for Trypanosomiasis Research and Control) in Mombasa, Kenya, in October 1999, the idea of an African-wide initiative to control tsetse and trypanosomiasis populations was discussed. During the 36th summit of the Organization for African Unity in Lome, Togo, in July 2000, a resolution was passed to form the Pan African Tsetse and Trypanosomiasis Eradication Campaign (PATTEC). The campaign works to eradicate the tsetse vector population levels and subsequently the protozoan disease, by use of insecticide-impregnated targets, fly traps, insecticide-treated cattle, ultra-low dose aerial/ground spraying (SAT) of tsetse resting sites and the sterile insect technique (SIT).[19] The use of SIT in Zanzibar proved effective in eliminating the entire population of tsetse flies but was expensive and is relatively impractical to use in many of the endemic countries afflicted with African trypanosomiasis.[18]
Regular active surveillance, involving detection and prompt treatment of new infections, and tsetse fly control is the backbone of the strategy used to control sleeping sickness. Systematic screening of at-risk communities is the best approach, because case-by-case screening is not practical in endemic regions. Systematic screening may be in the form of mobile clinics or fixed screening centres where teams travel daily to areas of high infection rates. Such screening efforts are important because early symptoms are not evident or serious enough to warrant patients with gambiense disease to seek medical attention, particularly in very remote areas. Also, diagnosis of the disease is difficult and health workers may not associate such general symptoms with trypanosomiasis. Systematic screening allows early-stage disease to be detected and treated before the disease progresses, and removes the potential human reservoir.[20] A single case of sexual transmission of West African sleeping sickness has been reported.[14]
Treatment
First stage
The current treatment for first-stage disease is intravenous or intramuscular pentamidine for T. b. gambiense or intravenous suramin for T. b. rhodesiense.[1]
Second stage
For T. b. gambiense the combination of nifurtimox and eflornithine (NECT) or eflornithine alone appear to be more effective and result in fewer side effects.[21] These treatments may replace melarsoprol when available[21] with the combination being first line.[2] NECT has the benefit of requiring less injections of eflornithine.[21]
Intravenous melarsoprol was previously the standard treatment for second-stage (neurological phase) disease and is effective for both types.[2] Melarsoprol is the only treatment for second stage T. b. rhodesiense; however, it causes death in 5% of people who take it.[2] Resistance to melarsoprol can occur.[2]
Epidemiology
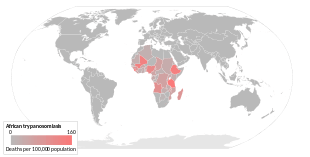
As of 2010 it caused around 9,000 deaths, down from 34,000 in 1990.[6] As of 2000, the disability-adjusted life-years (9 to 10 years) lost due to sleeping sickness are 2.0 million.[23] Over 60 million people living in some 250 locations are at risk of contracting the disease, and under 10,000 new cases were reported in 2009.[24]
The disease has been recorded as occurring in 37 countries, all in sub-Saharan Africa. It occurs regularly in southeast Uganda and western Kenya, and killed more than 48,000 Africans in 2008.[12] The population at risk being about 69 million with one third of this number being at a 'very high' to 'moderate' risk and the remaining two thirds at a 'low' to 'very low' risk.[5]
Prognosis
If untreated, T. b. gambiense almost always results in death, with only a few individuals shown in a long-term 15 year follow-up to have survived after refusing treatment. T. b. rhodesiense, being a more acute and severe form of the disease, is consistently fatal if not treated.[2] Disease progression greatly varies depending on disease form. For individuals which are infected by T. b. gambiense, which accounts for 98% of all of the reported cases, a person can be infected for months or even years without signs or symptoms until the advanced disease stage, where it is too late to be treated successfully. For individuals affected by T. b. rhodesiense, which accounts for 2% of all reported cases, symptoms appear within weeks or months of the infection. Disease progression is rapid and invades the central nervous system, causing death within a short amount of time.[25]
History
The condition has been present in Africa for thousands of years.[26] Because of a lack of travel between indigenous people, sleeping sickness in humans had been limited to isolated pockets. This changed once Arab slave traders entered central Africa from the east, following the Congo River, bringing parasites along. Gambian sleeping sickness travelled up the Congo River, then further eastwards.[27]
An Arab writer of the 14th century left the following description in the case of a sultan of the Malli [sic] Kingdom: "His end was to be overtaken by the sleeping sickness (illat an-nawm) which is a disease that frequently befalls the inhabitants of these countries especially their chieftains. Sleep overtakes one of them in such a manner that it is hardly possible to awake him."[27]

British naval surgeon John Atkins described the disease on his return from West Africa in 1734:
"The Sleepy Distemper (common among the Negroes) gives no other previous Notice, than a want of Appetite 2 or 3 days before; their sleeps are sound, and Sense and Feeling very little; for pulling, drubbing or whipping will scarce stir up Sense and Power enough to move; and the Moment you cease beating the smart is forgot, and down they fall again into a state of Insensibility, drivling constantly from the Mouth as in deep salivation; breathe slowly, but not unequally nor snort. Young people are more subject to it than the old; and the Judgement generally pronounced is Death, the Prognostik seldom failing. If now and then one of them recovers, he certainly loses the little Reason he had, and turns Ideot..."[27]
In 1901, a devastating epidemic erupted in Uganda, killing more than 250,000 people,[28] including about two-thirds of the population in the affected lakeshore areas. According to The Cambridge History of Africa, "It has been estimated that up to half the people died of sleeping-sickness and smallpox in the lands on either bank of the lower river Congo."[29]
The causative agent and vector were identified in 1903 by David Bruce, and the differentiation between the subspecies of the protozoa made in 1910. Bruce had earlier shown that T. brucei was the cause of a similar disease in horses and cattle that was transmitted by the tse-tse fly (Glossina morsitans).[27]
The first effective treatment, atoxyl, an arsenic-based drug developed by Paul Ehrlich and Kiyoshi Shiga, was introduced in 1910, but blindness was a serious side effect.
Suramin was first synthesized by Oskar Dressel and Richard Kothe in 1916 for Bayer. It was introduced in 1920 to treat the first stage of the disease. By 1922, Suramin was generally combined with tryparsamide (another pentavalent organoarsenic drug), the first drug to enter the nervous system and be useful in the treatment of the second stage of the gambiense form. Tryparsamide was announced in the Journal of Experimental Medicine in 1919 and tested in the Belgian Congo by Louise Pearce of the Rockefeller Institute in 1920. It was used during the grand epidemic in West and Central Africa on millions of people and was the mainstay of therapy until the 1960s.[30] American medical missionary Arthur Lewis Piper was active in using tryparsamide to treat sleeping sickness in the Belgian Congo in 1925.[31]
Pentamidine, a highly effective drug for the first stage of the disease, has been used since 1937.[32] During the 1950s, it was widely used as a prophylactic agent in western Africa, leading to a sharp decline in infection rates. At the time, eradication of the disease was thought to be at hand.
The organoarsenical melarsoprol (Arsobal) developed in the 1940s is effective for patients with second-stage sleeping sickness. However, 3–10% of those injected have reactive encephalopathy (convulsions, progressive coma, or psychotic reactions), and 10–70% of such cases result in death; it can cause brain damage in those who survive the encephalopathy. However, due to its effectiveness, melarsoprol is still used today. Resistance to melarsoprol is increasing, and combination therapy with nifurtimox is currently under research.
Eflornithine (difluoromethylornithine or DFMO), the most modern treatment, was developed in the 1970s by Albert Sjoerdsma and underwent clinical trials in the 1980s. The drug was approved by the United States Food and Drug Administration in 1990.[33] Aventis, the company responsible for its manufacture, halted production in 1999. In 2001, Aventis, in association with Médecins Sans Frontières and the World Health Organization, signed a long-term agreement to manufacture and donate the drug.
In addition to sleeping sickness, previous names have included negro lethargy, maladie du sommeil (Fr), Schlafkrankheit (Gr), African lethargy,[34] and Congo trypanosomiasis.[34][35]
Research
The genome of the parasite has been sequenced and several proteins have been identified as potential targets for drug treatment. Analysis of the genome also revealed the reason why generating a vaccine for this disease has been so difficult. T. brucei has over 800 genes that make proteins the parasite "mixes and matches" to evade immune system detection.[36]
Using a genetically modified form of a bacterium that occurs naturally in the gut of the vectors is being studied as a method of controlling the disease.[37]
Recent findings indicate the parasite is unable to survive in the bloodstream without its flagellum. This insight gives researchers a new angle with which to attack the parasite.[38]
Trypanosomiasis vaccines are undergoing research.
Additionally, the Drugs for Neglected Disease Initiative has contributed to the African sleeping sickness research effort by developing a compound called fexinidazole. This project was originally started in April 2007 and is currently in a pivotal study in clinical phase II/III.36 The goal is to have the drug succeed and be proven effective again stage one and stage two HAT caused by T. b. gambiense, as well HAT caused by T. b. rhodesiense.[39]
Funding
For current funding statistics, human African trypanosomiasis is grouped with kinetoplastid infections. Kinetoplastids refer to a group of flagellate protozoa.[40] Kinetoplastid infections include African sleeping sickness, Chagas' disease, and Leishmaniasis. All together, these three diseases accounted for 4.4 million disability adjusted life years (DALYs) and an additional 70,075 recorded deaths yearly.[40] For kinetoplastid infections, the total global research and development funding was approximately $136.3 million in 2012. Each of the three diseases, African sleeping sickness, Chagas' disease, and Leishmaniasis each received approximately a third of the funding, which was about $36.8 million US dollars, $38.7 million US dollars, and $31.7 million US dollars, respectively.[40]
For sleeping sickness, funding was split into basic research, drug discovery, vaccines, and diagnostics. The greatest amount of funding was directed towards basic research of the disease; approximately $21.6 million US dollars were directed towards that effort. As for therapeutic development, approximately $10.9 billion were invested.[40]
The top funder for kinetoplastid infection research and development are public sources. About 62% of the funding comes from high-income countries while 9% comes from low- and middle-income countries. High-income countries public funding is largest contributors to the neglected disease research effort. However, in recent years, funding from high-income countries has been steadily decreasing; in 2007, high-income countries provided 67.5% of the total funding whereas, in 2012, high-income countries public funds only provided 60% of the total funding for kinetoplastid infections. This downwards trend leaves a gap for other funders, such as philanthropic foundations and private pharmaceutical companies to fill.[40]
Much of the progress that has been made in African sleeping sickness and neglected disease research as a whole is a result of the other non-public funders. One of these major sources of funding has come from foundations, which have increasingly become more committed to neglected disease drug discovery in the 21st century. In 2012, philanthropic sources provided 15.9% of the total funding.[40] The Bill and Melinda Gates Foundation has been a leader in providing funding for neglected disease drug development. They have provided $444.1 million US dollars towards neglected disease research in 2012. To date, they have donated over $1.02 billion US dollars towards the neglected disease discovery efforts.[41]
For kinetoplastid infections specifically, they have donated an average of $28.15 million US dollars annually between the years 2007 to 2011.[40] They have labeled human African trypanosomiasis a high-opportunity target meaning it is a disease that presents the greatest opportunity for control, elimination, and eradication, through the development on new drugs, vaccines, public-health programs, and diagnostics. They are the second highest funding source for neglected diseases, immediately behind the US National Institutes of Health.[40] At a time where public funding is decreasing and government grants for scientific research are harder to obtain, the philanthropic world has stepped in to push the research forward.
Another important component of increased interest and funding has come from industry. In 2012, they contributed 13.1% total to the kinetoplastid research and development effort, and have additionally played an important role by contributing to public-private partnerships (PPP) as well as product-development partnerships (PDP).[40] A public-private partnership is an arrangement between one or more public entities and one or more private entities that exists to achieve a specific health outcome or to produce a health product. The partnership can exist in numerous ways; they may share and exchange funds, property, equipment, human resources, and intellectual property. These public-private partnerships and product-development partnerships have been established to address challenges in pharmaceutical industry, especially related to neglected disease research. These partnerships can help increase the scale of the effort towards therapeutic development by using different knowledge, skills, and expertise from different sources. These types of partnerships have been shown to be more effective than industry or public groups working independently.[42]
Other animals
Trypanosoma of both the rhodesiense and gambiense types can affect other animals such as cattle and wild animals.[1] In animals it is known as animal trypanosomiasis.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 WHO Media centre (March 2014). "Fact sheet N°259: Trypanosomiasis, Human African (sleeping sickness)". World Health Organization. Retrieved 25 April 2014.
- 1 2 3 4 5 6 7 8 9 Kennedy, PG (Feb 2013). "Clinical features, diagnosis, and treatment of human African trypanosomiasis (sleeping sickness).". Lancet neurology. 12 (2): 186–94. PMID 23260189. doi:10.1016/S1474-4422(12)70296-X.
- 1 2 GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015.". Lancet. 388 (10053): 1545–1602. PMC 5055577
 . PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/S0140-6736(16)31678-6. - 1 2 GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015.". Lancet. 388 (10053): 1459–1544. PMC 5388903
 . PMID 27733281. doi:10.1016/s0140-6736(16)31012-1.
. PMID 27733281. doi:10.1016/s0140-6736(16)31012-1. - 1 2 Simarro PP, Cecchi G, Franco JR, et al. (2012). "Estimating and mapping the population at risk of sleeping sickness". PLoS Negl Trop Dis. 6 (10): e1859. PMC 3493382
 . PMID 23145192. doi:10.1371/journal.pntd.0001859.
. PMID 23145192. doi:10.1371/journal.pntd.0001859. - 1 2 Lozano, R (15 December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010.". Lancet. 380 (9859): 2095–128. PMID 23245604. doi:10.1016/S0140-6736(12)61728-0.
- ↑ "Neglected Tropical Diseases". cdc.gov. June 6, 2011. Retrieved 28 November 2014.
- 1 2 GB Lundkvist; K Kristensson; M Bentivoglio (August 2004). "Why trypanosomes cause sleeping sickness". Physiology. 19 (4): 198–206. PMID 15304634. doi:10.1152/physiol.00006.2004.
- 1 2 3 4 5 Brun R, Blum J, Chappuis F, Burri C (January 2010). "Human African trypanosomiasis". Lancet. 375 (9709): 148–59. PMID 19833383. doi:10.1016/S0140-6736(09)60829-1.
- ↑ "East African Trypanosomiasis FAQs". Parasites — African Trypanosomiasis (also known as Sleeping Sickness). Centers for Disease Control and Prevention. 29 August 2012.
- ↑ "West African Trypanosomiasis FAQs". Parasites – African Trypanosomiasis (also known as Sleeping Sickness). Centers for Disease Control and Prevention. 29 August 2012.
- 1 2 "Uganda: Sleeping Sickness Reaching Alarming Levels". New Vision. 11 May 2008.
- ↑ Olowe SA (1975). "A case of congenital trypanosomiasis in Lagos". Trans. R. Soc. Trop. Med. Hyg. 69 (1): 57–9. PMID 1170654. doi:10.1016/0035-9203(75)90011-5.
- 1 2 Rocha G, Martins A, Gama G, Brandão F, Atouguia J (January 2004). "Possible cases of sexual and congenital transmission of sleeping sickness". Lancet. 363 (9404): 247. PMID 14738812. doi:10.1016/S0140-6736(03)15345-7.
- ↑ Cherenet T, Sani RA, Panandam JM, Nadzr S, Speybroeck N, van den Bossche P (December 2004). "Seasonal prevalence of bovine trypanosomosis in a tsetse-infested zone and a tsetse-free zone of the Amhara Region, north-west Ethiopia". Onderstepoort J. Vet. Res. 71 (4): 307–12. PMID 15732457. doi:10.4102/ojvr.v71i4.250.
- ↑ Cornford, E M; Bocash, W D; Braun, L D; Crane, P D; Oldendorf, W H; MacInnis, A J (1979). "Rapid distribution of tryptophol (3-indole ethanol) to the brain and other tissues". Journal of Clinical Investigation. 63 (6): 1241–8. PMC 372073
 . PMID 447842. doi:10.1172/JCI109419.
. PMID 447842. doi:10.1172/JCI109419. - ↑ Truc P; Lejon V; Magnus E; et al. (2002). "Evaluation of the micro-CATT, CATT/Trypanosoma brucei gambiense, and LATEX/T b gambiense methods for serodiagnosis and surveillance of human African trypanosomiasis in West and Central Africa". Bull. World Health Organ. 80 (11): 882–6. PMC 2567684
 . PMID 12481210. Retrieved 16 March 2009.
. PMID 12481210. Retrieved 16 March 2009. - 1 2 Brun R, Blum J, Chappuis F, Burri C (January 2010). "Human African trypanosomiasis". Lancet. 375 (9709): 148–59. PMID 19833383. doi:10.1016/S0140-6736(09)60829-1.
See pp. 154–5
- ↑ Schofield CJ, Kabayo JP (2008). "Trypanosomiasis vector control in Africa and Latin America". Parasit Vectors. 1 (1): 24. PMC 2526077
 . PMID 18673535. doi:10.1186/1756-3305-1-24.
. PMID 18673535. doi:10.1186/1756-3305-1-24. - ↑ "Strategic Direction for African Trypanosomiasis Research". Special Programme for Research and Training in Tropical Diseases. Archived from the original on 22 March 2006. Retrieved 1 March 2006.
- 1 2 3 Lutje, V; Seixas, J; Kennedy, A (28 June 2013). "Chemotherapy for second-stage human African trypanosomiasis.". The Cochrane database of systematic reviews. 6: CD006201. PMID 23807762. doi:10.1002/14651858.CD006201.pub3.
- ↑ WHO mortality and health data and statistics, accessed 10 February 2009.
- ↑ World Health Organization (Geneva) (2000). "World Health Report 2000: Health Systems Improving Performance".
- ↑ WHO Expert Committee on Control and Surveillance of African trypanosomiasis (Geneva) (1998). "WHO Technical Report Series, No.881".
- ↑ "Trypanosomiasis, human African (sleeping sickness)". World Health Organization. March 2014.
- ↑ Steverding, D (12 February 2008). "The history of African trypanosomiasis.". Parasites & vectors. 1 (1): 3. PMC 2270819
 . PMID 18275594. doi:10.1186/1756-3305-1-3.
. PMID 18275594. doi:10.1186/1756-3305-1-3. - 1 2 3 4 Strong, Richard P (1944). Stitt's Diagnosis, Prevention and Treatment of Tropical Diseases (Seventh ed.). York, PA: The Blakiston company. p. 165.
- ↑ Fèvre EM, Coleman PG, Welburn SC, Maudlin I (April 2004). "Reanalyzing the 1900–1920 sleeping sickness epidemic in Uganda". Emerging Infect. Dis. 10 (4): 567–73. PMID 15200843. doi:10.3201/eid1004.020626.
- ↑ Fage, John D. (5 September 1985). The Cambridge History of Africa: From the earliest times to c. 500 BC. Cambridge University Press. p. 748. ISBN 978-0-521-22803-9.
- ↑ Steverding, Dietmar (2010). "The development of drugs for treatment of sleeping sickness: a historical review". Parasites & Vectors. 3 (1): 15. PMC 2848007
 . PMID 20219092. doi:10.1186/1756-3305-3-15. Retrieved 14 October 2014.
. PMID 20219092. doi:10.1186/1756-3305-3-15. Retrieved 14 October 2014. - ↑ Klingman, Jack (1994). "Arthur Lewis Piper, M.D.: A Medical Missionary in the Belgian Congo". Journal of Community Health. 19 (2). Periodicals Archive Online accessed 15 October 2013.
- ↑ Magill, Alan J.; Strickland, G. Thomas; Maguire, James H.; Ryan, Edward T.; Solomon, Tom (2012). Hunter's Tropical Medicine and Emerging Infectious Disease (9 ed.). Elsevier Health Sciences. p. 723. ISBN 1455740438.
- ↑ Urban Hellgren; Orjan Ericsson; Yakoub AdenAbdi; Lars L Gustafsson. Handbook of Drugs for Tropical Parasitic Infections. p. 60. ISBN 9780203211519.
- 1 2 Robinson, Victor, ed. (1939). "African Lethargy, Sleeping Sickness, or Congo trypanosomiasis; Trypanosoma gambiense". The Modern Home Physician, A New Encyclopedia of Medical Knowledge. WM. H. Wise & Company (New York)., pp. 20–21.
- ↑ Strong, Richard P (1944). Stitt's Diagnosis, Prevention and Treatment of Tropical Diseases (Seventh ed.). York, PA: The Blakiston company. p. 164.
- ↑ Berriman M; Ghedin E; Hertz-Fowler C; et al. (2005). "The genome of the African trypanosome Trypanosoma brucei". Science. 309 (5733): 416–22. Bibcode:2005Sci...309..416B. PMID 16020726. doi:10.1126/science.1112642.
- ↑ Doudoumis V, Alam U, Aksoy E, et al. (March 2013). "Tsetse-Wolbachia symbiosis: comes of age and has great potential for pest and disease control". J. Invertebr. Pathol. 112 (Suppl): S94–103. PMC 3772542
 . PMID 22835476. doi:10.1016/j.jip.2012.05.010.
. PMID 22835476. doi:10.1016/j.jip.2012.05.010. - ↑ "African Sleeping Sickness Breakthrough". Archived from the original on 13 May 2006. Retrieved 7 April 2006.
- ↑ "Fexinidazole". Drugs for Neglected Disease Initiative. October 2013.
- 1 2 3 4 5 6 7 8 9 Moran, M.; Guzman, J.; Chapman, N.; Abela-Oversteengen, L.; Howard, R.; Farrell, P.; Luxford, J. "Neglected Disease Research and Development: The Public Divide." (PDF). Global Funding of Innovation for Neglected Disease. Retrieved 30 October 2016.
- ↑ "Strategy Overview". Neglected Infectious Diseases. Bill and Melinda Gates Foundation. 2013.
- ↑ "Background Paper 8: 8.1 Public-Private Partnerships and Innovation" (PDF). Priority Medicines for Europe and the World Update Report. World Health Organization. 2013.
External links
| Classification |
V · T · D |
|---|---|
| External resources |
- "Sleeping sickness". Médecins Sans Frontières.
- Links to pictures of Sleeping Sickness (Hardin MD/ University of Iowa) archived 2006-02-19.
- Hale Carpenter, G.D. (1920). A Naturalist on Lake Victoria, with an Account of Sleeping Sickness and the Tse-tse Fly. Unwin. OCLC 2649363.