Aerobic vaginitis
| Aerobic vaginitis | |
|---|---|
| Classification and external resources | |
| Specialty | Gynecology |
Aerobic vaginitis (AV) is a form of vaginitis first described by Donders et al. in 2002.[1][2] It is characterized by a more or less severe disruption of the lactobacillary flora, along with inflammation, atrophy, and the presence of a predominantly aerobic microflora, composed of enteric commensals or pathogens.[3]
It can be considered the aerobic counterpart of bacterial vaginosis. The lack of acknowledgement of the difference between the two conditions might have led to inaccurate conclusions in several studies in the past.[4] The entity that has been described as "desquamative inflammatory vaginitis" probably corresponds to the more severe forms of aerobic vaginitis.[5]
Epidemiology
About 5 to 10% of women are affected by aerobic vaginitis.[6] Reports in pregnant women point to a prevalence of 8.3–10.8%.[7][8]
When considering symptomatic women, the prevalence of AV can be as high as 23%.[9][10][11]
Signs and symptoms
Women with aerobic vaginitis usually present with a thinned reddish vaginal mucosa, sometimes with extensive erosions or ulcerations and abundant yellowish discharge (without the fishy amine odour, typical of bacterial vaginosis). The pH is usually high. Symptoms can include burning, stinging and dyspareunia. The symptoms can last for long periods of time—sometimes even years. Typically, patients have been treated several times with antimycotic and antibiotic drugs without relief.[3] In asymptomatic cases, there is microscopic evidence but no symptoms. The prevalence of asymptomatic cases is unknown.[3]
Diagnosis
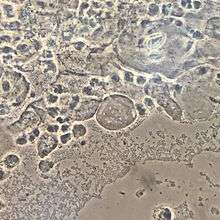
The diagnosis is based on microscopic criteria. Ideally, phase-contrast microscopy is used with a magnification of 400x (high-power field).[12] For scoring purposes, along with relative number of leucocytes, percentage of toxic leucocytes, background flora and proportion of epitheliocytes, lactobacillary grade must be evaluated:
- grade I
- numerous pleiomorphic lactobacilli; no other bacteria
- grade IIa
- mixed flora, but predominantly lactobacilli
- grade IIb
- mixed flora, but proportion of lactobacilli severely decreased because of an increased number of other bacteria
- grade III
- lactobacilli severely depressed or absent because of overgrowth of other bacteria
| AV score | Lactobacillary grades | Number of leukocytes | Proportion of toxic leucocytes | Background flora | Proportion of parabasal epitheliocytes |
|---|---|---|---|---|---|
| 0 | I and IIa | <10/hpf | None or sporadic | Unremarkable or cytolysis | None or <1% |
| 1 | IIb | >10/hpf and; <10/epithelial cell | <50% of leukocytes | Small coliform bacilli | ≤10% |
| 2 | III | >10/epithelial cell | >50% of leukocytes | Cocci or chains | >10% |
The "AV score" is calculated according to what is described in the table.
- AV score <3: no signs of AV
- AV score 3 or 4: light AV
- AV score 5 or 6: moderate AV
- AV score ≥6: severe AV.
pH measurement alone is not enough for the diagnosis.
Complications
Aerobic vaginitis has been associated with several gynecological and obstetrical complications, including:
- Premature rupture of membranes
- Preterm labour
- Ascending chorioamnionitis.[13]
- Increased risk to acquire sexually transmitted infections (including HIV)[14]
- Abnormal Pap test results[15][16]
Treatment
Treatment is not always easy and aims at correcting the three key changes encountered in aerobic vaginitis: the presence of atrophy, inflammation and abnormal flora. The treatment can include topical steroids to diminish the inflammation and topical estrogen to reduce the atrophy. The use and choice of antibiotics to diminish the load/proportion of aerobic bacteria is still a matter of debate. The use of local antibiotics, preferably local non-absorbed and broad spectrum, covering enteric gram-positive and gram-negative aerobes, like kanamycin can be an option. In some cases, systemic antibiotics can be helpful, such as amoxyclav or moxifloxacin.[17] Vaginal rinsing with povidone iodine can provide rapid relief of symptoms but does not provide long-term reduction of bacterial loads.[18] Dequalinium chloride can also be an option for treatment.[19]
References
- ↑ Donders, Gilbert G.G.; Vereecken, Annie; Bosmans, Eugene; Dekeersmaecker, Alfons; Salembier, Geert; Spitz, Bernard (2002). "Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis". BJOG. 109 (1): 34–43. PMID 11845812. doi:10.1111/j.1471-0528.2002.00432.x.
- ↑ Donders, Gilbert G. G.; Bellen, Gert; Grinceviciene, Svitrigaile; Ruban, Kateryna; Vieira-Baptista, Pedro (2017-05-11). "Aerobic vaginitis: no longer a stranger". Research in Microbiology. ISSN 1769-7123. PMID 28502874. doi:10.1016/j.resmic.2017.04.004.
- 1 2 3 Donders, G; Bellen, G; Rezeberga, D (2011). "Aerobic vaginitis in pregnancy". BJOG. 118 (10): 1163–70. PMID 21668769. doi:10.1111/j.1471-0528.2011.03020.x.
- ↑ Han, Cha; Wu, Wenjuan; Fan, Aiping; Wang, Yingmei; Zhang, Huiying; Chu, Zanjun; Wang, Chen; Xue, Fengxia (2015). "Diagnostic and therapeutic advancements for aerobic vaginitis". Archives of Gynecology and Obstetrics. 291 (2): 251–7. PMID 25367602. doi:10.1007/s00404-014-3525-9.
- ↑ Newbern, EC; Foxman, B; Leaman, D; Sobel, JD (2002). "Desquamative Inflammatory Vaginitis An Exploratory Case-Control Study". Annals of Epidemiology. 12 (5): 346–52. PMID 12062923. doi:10.1016/S1047-2797(01)00316-7.
- ↑ Tansarli, G. S.; Kostaras, E. K.; Athanasiou, S.; Falagas, M. E. (2013). "Prevalence and treatment of aerobic vaginitis among non-pregnant women: evaluation of the evidence for an underestimated clinical entity". European Journal of Clinical Microbiology & Infectious Diseases. 32 (8): 977–84. PMID 23443475. doi:10.1007/s10096-013-1846-4.
- ↑ Donders, GG; Van Calsteren, K; Bellen, G; Reybrouck, R; Van den Bosch, T; Riphagen, I; Van Lierde, S (2009). "Predictive value for preterm birth of abnormal vaginal flora, bacterial vaginosis and aerobic vaginitis during the first trimester of pregnancy". BJOG. 116 (10): 1315–24. PMID 19538417. doi:10.1111/j.1471-0528.2009.02237.x.
- ↑ Zodzika, Jana; Rezeberga, Dace; Jermakova, Irina; Vasina, Olga; Vedmedovska, Natalija; Donders, Gilbert (2011). "Factors related to elevated vaginal pH in the first trimester of pregnancy". Acta Obstetricia et Gynecologica Scandinavica. 90 (1): 41–6. PMID 21275914. doi:10.1111/j.1600-0412.2010.01011.x.
- ↑ Fan, Aiping; Yue, Yingli; Geng, Nv; Zhang, Huiying; Wang, Yingmei; Xue, Fengxia (2013). "Aerobic vaginitis and mixed infections: comparison of clinical and laboratory findings". Archives of Gynecology and Obstetrics. 287 (2): 329–35. PMID 23015152. doi:10.1007/s00404-012-2571-4.
- ↑ Bologno, Romina; Díaz, Yanina M.; Giraudo, María C.; Fernández, Rosa; Menéndez, Viviana; Brizuela, Juan C.; Gallardo, Adriana A.; Álvarez, Laura A.; Estevao Belchior, Silvia G. (2011). "Importancia del estudio del balance del contenido vaginal (BACOVA) en el control preventivo de las trabajadoras sexuales" [Importance of studying the balance of vaginal content (BAVACO) in the preventive control of sex workers]. Revista Argentina De Microbiología (in Spanish). 43 (4): 246–50. PMID 22274820. doi:10.1590/S0325-75412011000400002 (inactive 2017-01-31).
- ↑ Marconi, C.; Donders, G.G.G.; Bellen, G.; Brown, D.R.; Parada, C.M.G.L.; Silva, M.G. (2013). "Sialidase activity in aerobic vaginitis is equal to levels during bacterial vaginosis". European Journal of Obstetrics & Gynecology and Reproductive Biology. 167 (2): 205–9. PMID 23375395. doi:10.1016/j.ejogrb.2012.12.003.
- ↑ Donders, G.G.G.; Larsson, P.G.; Platz-Christensen, J.J.; Hallén, A.; van der Meijden, W.; Wölner-Hanssen, P. (2009). "Variability in diagnosis of clue cells, lactobacillary grading and white blood cells in vaginal wet smears with conventional bright light and phase contrast microscopy". European Journal of Obstetrics & Gynecology and Reproductive Biology. 145 (1): 109–12. PMID 19481329. doi:10.1016/j.ejogrb.2009.04.012.
- ↑ Donders, G. G. G.; Moerman, P.; De Wet, G. H.; Hooft, P.; Goubau, P. (1991). "The association between Chlamydia cervicitis, chorioamnionitis and neonatal complications". Archives of Gynecology and Obstetrics. 249 (2): 79–85. PMID 1953055. doi:10.1007/BF02390366.
- ↑ Donders, Gilbert; De Wet, Henry; Hooft, Peter; Desmyter, Jan (1993). "Lactobacilli in Papanicolaou Smears, Genital Infections, and Pregnancy". American Journal of Perinatology. 10 (5): 358–61. PMID 8240593. doi:10.1055/s-2007-994761.
- ↑ Jahic, Mahira; Mulavdic, Mirsada; Hadzimehmedovic, Azra; Jahic, Elmir (2013). "Association Between Aerobic Vaginitis, Bacterial Vaginosis and Squamous Intraepithelial Lesion of Low Grade". Medical Archives. 67 (2): 94–6. PMID 24341052. doi:10.5455/medarh.2013.67.94-96.
- ↑ Vieira-Baptista, P.; Lima-Silva, J.; Pinto, C.; Saldanha, C.; Beires, J.; Martinez-de-Oliveira, J.; Donders, G. (2016). "Bacterial vaginosis, aerobic vaginitis, vaginal inflammation and major Pap smear abnormalities". European Journal of Clinical Microbiology & Infectious Diseases. 35 (4): 657–64. PMID 26810061. doi:10.1007/s10096-016-2584-1.
- ↑ Wang, C.; Han, C.; Geng, N.; Fan, A.; Wang, Y.; Yue, Y.; Zhang, H.; Xue, F. (2016). "Efficacy of oral moxifloxacin for aerobic vaginitis". European Journal of Clinical Microbiology & Infectious Diseases. 35 (1): 95–101. PMID 26526787. doi:10.1007/s10096-015-2513-8.
- ↑ Donders, Gilbert G. G.; Ruban, Katerina; Bellen, Gert (2015). "Selecting Anti-Microbial Treatment of Aerobic Vaginitis". Current Infectious Disease Reports. 17 (5): 477. PMID 25896749. doi:10.1007/s11908-015-0477-6.
- ↑ Mendling, Werner; Weissenbacher, Ernst Rainer; Gerber, Stefan; Prasauskas, Valdas; Grob, Philipp (2016). "Use of locally delivered dequalinium chloride in the treatment of vaginal infections: a review". Archives of Gynecology and Obstetrics. 293 (3): 469–84. PMC 4757629
 . PMID 26506926. doi:10.1007/s00404-015-3914-8.
. PMID 26506926. doi:10.1007/s00404-015-3914-8.