Adie syndrome
| Adie's syndrome | |
|---|---|
| Synonyms | Holmes–Adie syndrome, Adie's tonic pupil, Holmes-Adie pupil |
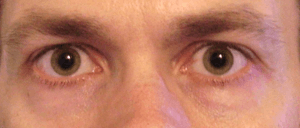 | |
| Bilateral mydriasis given the observational diagnosis Adie's pupils by an ophthalmologist | |
| Pronunciation |
|
| Classification and external resources | |
| Specialty | ophthalmology |
| ICD-10 | H57.0 |
| ICD-9-CM | 379.46 |
| DiseasesDB | 29742 |
| MeSH | D015845 |
Adie syndrome is a neurological disorder characterized by a tonically dilated pupil that reacts slowly to light but shows a more definite response to accommodation (i.e., light-near dissociation).[1] It is frequently seen in females with absent knee or ankle jerks and impaired sweating. It is named after the British neurologist William John Adie. It is caused by damage to the postganglionic fibers of the parasympathetic innervation of the eye, usually by a viral or bacterial infection which causes inflammation, and affects the pupil of the eye and the autonomic nervous system.[1]
Signs and symptoms
Adie syndrome presents with three hallmark symptoms, namely at least one abnormally dilated pupil (mydriasis) which does not constrict in response to light, loss of deep tendon reflexes, and abnormalities of sweating.[1] Other signs may include hyperopia due to accommodative paresis, photophobia and difficulty reading.[2]
Pathophysiology
Pupillary symptoms of Holmes–Adie syndrome are thought to be the result of a viral or bacterial infection that causes inflammation and damage to neurons in the ciliary ganglion, located in the posterior orbit, that provides parasympathetic control of eye constriction. Additionally, patients with Holmes-Adie Syndrome can also experience problems with autonomic control of the body. This second set of symptoms is caused by damage to the dorsal root ganglia of the spinal cord.[1]
Diagnosis
Clinical exam may reveal sectoral paresis of the iris sphincter or vermiform iris movements. The tonic pupil may become smaller (miotic) over time which is referred to as "little old Adie's".[3] Testing with low dose (1/8%) pilocarpine may constrict the tonic pupil due to cholinergic denervation supersensitivity.[1] A normal pupil will not constrict with the dilute dose of pilocarpine.[3] CT scans and MRI scans may be useful in the diagnostic testing of focal hypoactive reflexes.[4]
Treatment
The usual treatment of a standardised Adie syndrome is to prescribe reading glasses to correct for impairment of the eye(s).[1] Pilocarpine drops may be administered as a treatment as well as a diagnostic measure.[1] Thoracic sympathectomy is the definitive treatment of diaphoresis, if the condition is not treatable by drug therapy.[1]
Prognosis
Adie's syndrome is not life-threatening or disabling.[1] As such, there is no mortality rate relating to the condition; however, loss of deep tendon reflexes is permanent and may progress over time.[1]
Epidemiology
It most commonly affects younger women (2.6:1 female preponderance) and is unilateral in 80% of cases.[3] Average age of onset is 32 years.
See also
References
- 1 2 3 4 5 6 7 8 9 10 National Institute of Neurological Disorders and Stroke. "Holmes-Adie syndrome Information Page". Retrieved 2008-01-21.
- ↑ Stedman's Medical Dictionary, 27th Edition. 2000. ISBN 0-683-40007-X.
- 1 2 3 Haines, Duane E. (2002). Fundamental Neuroscience, 2nd edition. ISBN 0-443-06603-5.
- ↑ "Diagnosis of Adie syndrome". WrongDiagnosis.com. Retrieved 2008-01-21.
External links
- Animation at mrcophth.com