Achilles tendon
| Achilles tendon | |
|---|---|
 Posterior view of the foot and leg, showing the Achilles tendon (tendo calcaneus). The gastrocnemius muscle is cut to expose the soleus. | |
|
Lateral view of the human ankle, including the Achilles tendon | |
| Details | |
| Identifiers | |
| Latin | tendo calcaneus, tendo Achillis |
| MeSH | A02.880.176 |
| Dorlands /Elsevier | t_04/12793915 |
| TA | A04.7.02.048 |
| FMA | 51061 |
The Achilles tendon or heel cord, also known as the calcaneal tendon (Latin: Tendo calcaneus), is a tendon of the back of the leg, and the thickest in the human body. It serves to attach the plantaris, gastrocnemius (calf) and soleus muscles to the calcaneus (heel) bone. These muscles, acting via the tendon, cause plantar flexion of the foot at the ankle, and (except soleus) flexion at the knee.
The tendon can rupture and become inflamed.
Etymology
The oldest-known written record of the tendon being named for Achilles is in 1693 by the Flemish/Dutch anatomist Philip Verheyen. In his widely used text Corporis Humani Anatomia, Chapter XV, page 328, he described the tendon's location and said that it was commonly called "the cord of Achilles" ("quae vulgo dicitur chorda Achillis"), now also called "tendo achillies" by anatomists. Verheyen referred to the mythological account of Achilles being held by the heel when dipped in the River Styx to protect his body from harm.
The Achilles tendon is also known as the calcaneal tendon. Because eponyms (names relating to people) have no relationship to the subject matter, most anatomical eponyms also have scientifically descriptive terms. The term calcaneal comes from the Latin calcaneum, meaning heel.
Structure
The Achilles tendon connects muscle to bone, like other tendons, and is located at the back of the lower leg. The Achilles tendon connects the gastrocnemius and soleus muscles to the calcaneal tuberosity on the calcaneus (heel bone).[1] The tendon begins near the middle of the calf, and receives fleshy fibers on its inner surface, almost to its lower end. Gradually thinning below, it inserts into the middle part of the back of the calcaneus bone. The tendon spreads out somewhat at its lower end, so that its narrowest part is about 4 centimetres (1.6 in) above its insertion.
The tendon is covered by the fascia and the integument, and stands out prominently behind the bone; the gap is filled up with areolar and adipose tissue. A bursa lies between the tendon and the upper part of the calcaneus. It is the thickest and strongest tendon in the body. It is about 15 centimetres (6 in) long. Along the side of the muscle, and superficial to it, is the small saphenous vein. The tendon can receive a load stress 3.9 times body weight during walking and 7.7 times body weight when running.[2]
Function
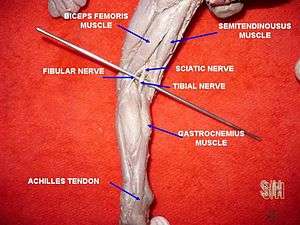
Acting via the Achilles tendon, the gastrocnemius and soleus muscles cause plantar flexion of the foot at the ankle. This action brings the sole of the foot closer to the back of the leg. The gastrocnemius also flexes the leg at the knee. Both muscles are innervated by the tibial nerve.[1]
Vibration of the tendon without vision has a major impact on postural orientation.[3] Vibration of the tendon causes movement backwards and the illusion of a forward body tilt in standing subjects.[4] This is because vibrations stimulate muscle spindles in the calf muscles. The muscle spindles alert the brain that the body is moving forward, so the central nervous system compensates by moving the body backwards.
Clinical significance
Inflammation
Inflammation of the Achilles tendon is called Achilles tendinitis. Achilles tendinosis is the soreness or stiffness of the tendon, generally due to overuse. Inflammation was thought to be the cause of most tendon pain, until the late 1990s, when scientists discovered no evidence of inflammation.
Degeneration
Achilles tendon degeneration (tendinosis) is typically investigated with either MRI or ultrasound. In both cases, the tendon is thickened, may demonstrate surrounding inflammation by virtue of the presence of paratenonitis, retrocalcaneal or retroAchilles bursitis. Within the tendon, increased blood flow, tendon fibril disorganisation and partial thickness tears may be identified. Achilles tendinosis frequently involves the mid portion of the tendon, however may involve the insertion where this is known as enthesopathy. Though enthesopathy may be seen in the context of advancing age, it is also associated with arthritis such as gout and the seronegative spondyloarthitides. Achilles tendinosis is a known risk factor for calf muscle tears.[5]
Rupture
Achilles tendon rupture is a partial or complete break in the tendon. Partial and full Achilles tendon ruptures are most likely to occur in sports requiring sudden eccentric stretching, such as sprinting. The area approximately two inches above the calcaneal attachment is most susceptible to these ruptures due to a zone of avascularity. Maffulli et al.[6] suggested that the clinical label of tendinopathy be given to the combination of tendon pain, swelling and impaired performance. They require immobilization or surgery.
In a case where Achilles tendon rupture is concerned, there are three main types of treatment: the open and the percutaneous operative methods, and nonoperative approaches.
Initial treatment of damage to the tendon is generally nonoperative. Orthotics can produce early relief to the tendon by the correction of malalignments; non-steroidal anti-inflammatory drugs (NSAIDs) are generally to be avoided as they make the more-common tendinopathy (degenerative) injuries worse,[7] though they may very occasionally be indicated for the rarer tendinitis (inflammatory) injuries. Physiotherapy by eccentric calf stretching under resistance is commonly recommended, usually in conjunction with podiatric insoles or heel cushioning.
Depending on the severity of the injury, recovery from an Achilles injury can take up to 12–16 months.
To reduce the chances of obtaining a ruptured Achilles or any other Achilles tendon complications, a few simple steps can be taken when it comes to physical activity. First, stretching the calf muscle to the point of feeling an obvious pull, as well as calf-strengthening exercises can help the muscle and tendon absorb more force resulting in less chance of injury. Second, try to avoid running or participating in physical activity on hard or slippery surfaces. Lastly, try to increase training intensity at a slow-to-medium rate. The most common Achilles tendon injuries occur when someone abruptly intensifies their training at an abnormal rate.[8][9]
Other
Tendon xanthomas are cholesterol deposits that commonly develop in the Achilles tendon of people with lipid metabolism disorders such as familial hypercholesterolemia.[10]
The Achilles' tendon is often tested as part of a neurological examination. In this examination, the tendon is hit with a tendon hammer. This tests the S1 and S2 spinal nerves. A healthy response is plantar flexion of the foot.[11]
Other animals
The Achilles tendon is short or absent in great apes, but long in arboreal gibbons and humans.[12] It provides elastic energy storage in hopping,[13] walking, and running.[12] Computer models suggest this energy storage Achilles tendon increases top running speed by >80% and reduces running costs by more than three-quarters.[12] It has been suggested that the "absence of a well-developed Achilles tendon in the nonhuman African apes would preclude them from effective running, both at high speeds and over extended distances."[12]
See also
| Wikimedia Commons has media related to Achilles tendon. |
Additional images
- Dorsum and sole of Foot. Ankle joint. Deep dissection.
References
- 1 2 Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students. Philadelphia: Elsevier/Churchill Livingstone. p. 546. ISBN 978-0-8089-2306-0.
- ↑ Giddings, VL; Beaupré, GS; Whalen, RT; Carter, DR (2000). "Calcaneal loading during walking and running". Medicine and science in sports and exercise. 32 (3): 627–34. PMID 10731005. doi:10.1097/00005768-200003000-00012.
- ↑ Effects of bilateral Achilles tendon vibration on postural orientation and balance during standing, 2007 International Federation of Clinical Neurophysiology. Published by Elsevier Inc.
- ↑ ScienceDirect – Neuroscience Letters: Effect of Achilles tendon vibration on postural orientation
- ↑ Koulouris G, Ting AY, Jhamb A, Connell D, Kavanagh EC (2007). "Magnetic resonance imaging findings of injuries to the calf muscle complex". Skeletal Radiol. 36 (10): 921–7. PMID 17483942. doi:10.1007/s00256-007-0306-6.
- ↑ Maffulli, N.; Khan, K. M.; Puddu, G. (1998). "Overuse Tendon Conditions: Time to Change a Confusing Terminology". Arthroscopy. 14 (8): 840–3. doi:10.1016/s0749-8063(98)70021-0.
- ↑ 'Achilles injuries: How to recover', RunningInjury
- ↑ Achilles Tendon Rupture Prevention, 1998 Mayo Foundation for Education and Research.
- ↑ The Influence of Stretching and Warm-up Exercises on Achilles Tendon Reflex Activity, 1995 Journal of Sports Sciences. Doi = 10.1080/02640419508732265
- ↑ Longo, D; Fauci, A; Kasper, D; Hauser, S; Jameson, J; Loscalzo, J (2012). Harrison's Principles of Internal Medicine (18th ed.). New York: McGraw-Hill. p. 3149. ISBN 978-0071748896.
- ↑ Talley, Nicholas J.; O'Connor, Simon (2013). Clinical Examination: A Systematic Guide to Physical Diagnosis (7th ed.). p. 453. ISBN 9780729541985.
- 1 2 3 4 Sellers WI, Pataky TC, Caravaggi P, Crompton RH. (2010). Evolutionary Robotic Approaches in Primate Gait Analysis. Int J Primatol 31:321–338 doi:10.1007/s10764-010-9396-4
- ↑ Lichtwark, GA; Wilson, AM (2005). "In vivo mechanical properties of the human Achilles tendon during one-legged hopping". The Journal of Experimental Biology. 208 (Pt 24): 4715–25. PMID 16326953. doi:10.1242/jeb.01950.