Abdominal trauma
| Abdominal trauma | |
|---|---|
|
| |
| Abdominal trauma resulting in a right kidney contusion (open arrow) and blood surrounding the kidney (closed arrow) as seen on CT | |
| Classification and external resources | |
| Specialty | emergency medicine |
| ICD-10 | S30-S39 |
| ICD-9-CM | 868 |
| eMedicine | med/2805 emerg/1 |
| Patient UK | Abdominal trauma |
| MeSH | D000007 |
Abdominal trauma is an injury to the abdomen. It may be blunt or penetrating and may involve damage to the abdominal organs.[1] Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Abdominal trauma presents a risk of severe blood loss and infection. Diagnosis may involve ultrasonography, computed tomography, and peritoneal lavage, and treatment may involve surgery.[2] Injury to the lower chest may cause splenic or liver injuries.[3]
Classification
Abdominal trauma is divided into blunt and penetrating types. While penetrating abdominal trauma (PAT) is usually diagnosed based on clinical signs, diagnosis of blunt abdominal trauma is more likely to be delayed or altogether missed because clinical signs are less obvious.[2] Blunt injuries predominate in rural areas, while penetrating ones are more frequent in urban settings.[4] Penetrating trauma is further subdivided into stab wounds and gunshot wounds, which require different methods of treatment.[5]
Signs and symptoms

Signs and symptoms are not seen in early days and after some days initial pain is seen. People injured in motor vehicle collisions may present with a "seat belt sign," bruising on the abdomen along the site of the lap portion of the safety belt; this sign is associated with a high rate of injury to the abdominal organs.[6] Seatbelts may also cause abrasions and hematomas; up to 30 percent of people with such signs have associated internal injuries.[4] Early indications of abdominal trauma include nausea, vomiting, blood in the urine, and fever.[6][7] The injury may present with abdominal pain, tenderness,[5] distension, or rigidity to the touch, and bowel sounds may be diminished or absent. Abdominal guarding is a tensing of the abdominal wall muscles to guard inflamed organs within the abdomen. Pneumoperitoneum, air or gas in the abdominal cavity, may be an indication of rupture of a hollow organ. In penetrating injuries, an evisceration (protrusion of internal organs out of a wound) may be present.[8]
Injuries associated with intra-abdominal trauma include rib fractures, vertebral fractures, pelvic fractures, and injuries to the abdominal wall.[9]
Causes
Motor vehicle collisions are a common source of blunt abdominal trauma.[4] Seat belts reduce the incidence of injuries such as head injury and chest injury, but present a threat to such abdominal organs as the pancreas and the intestines, which may be displaced or compressed against the spinal column.[4] Children are especially vulnerable to abdominal injury from seat belts, because they have softer abdominal regions and seat belts were not designed to fit them.[6] In children, bicycle mishaps are also a common cause of abdominal injury, especially when the abdomen is struck by the handlebars.[6] Sports injuries can affect abdominal organs such as the spleen and kidneys.[5] Falls and sports are also frequent mechanisms of abdominal injury in children.[6] Abdominal injury may result from child abuse and is the second leading cause of child abuse-related death, after traumatic brain injury.[7]
Gunshot wounds, which are higher energy than stab wounds, are usually more damaging than the latter.[10] Gunshot wounds that penetrate the peritoneum result in significant damage to major intra-abdominal structures in some 90 percent of cases.[10]
Pathophysiology
Abdominal trauma can be life-threatening because abdominal organs, especially those in the retroperitoneal space, can bleed profusely, and the space can hold a great deal of blood.[11] Solid abdominal organs, such as the liver and kidneys, bleed profusely when cut or torn, as do major blood vessels such as the aorta and vena cava.[11] Hollow organs such as the stomach, while not as likely to result in shock from profuse bleeding, present a serious risk of infection,[11] especially if such an injury is not treated promptly.[4] Gastrointestinal organs such as the bowel can spill their contents into the abdominal cavity.[4] Hemorrhage and systemic infection are the main causes of deaths that result from abdominal trauma.[4]
One or more of the intra-abdominal organs may be injured in abdominal trauma. The characteristics of the injury are determined in part by which organ or organs are injured.
Liver
The liver, the most vulnerable abdominal organ to all forms of injury because of its size and location (in the upper right quadrant of the abdomen), is injured in about five percent of all people admitted to a hospital for trauma.[12] Liver injuries present a serious risk for shock because the liver tissue is delicate and has a large blood supply and capacity.[11] In children, the liver is the most commonly injured abdominal organ.[13] The liver may be lacerated or contused, and a hematoma may develop.[13] It may leak bile, usually without serious consequences.[13] If severely injured, the liver may cause exsanguination (bleeding to death), requiring emergency surgery to stop the bleeding.[9]
Spleen
Spleen is the most common cause of massive bleeding in blunt abdominal trauma to a solid organ. The liver, conversely, is the most commonly injured organ. The spleen is the second most commonly injured intra-abdominal organ in children.[13] A laceration of the spleen may be associated with hematoma.[13] Because of the spleen's ability to bleed profusely, a ruptured spleen can be life-threatening, resulting in shock. However, unlike the liver, penetrating trauma to the spleen, pancreas and kidneys do not present as much of an immediate threat of shock unless they lacerate a major blood vessel supplying the organs, such as the renal artery.[4] Fractures of the left lower ribs are associated with spleen lacerations in 20 percent of cases.[9]
Pancreas
The pancreas may be injured in abdominal trauma, for example by laceration or contusion.[6] Pancreatic injuries, most commonly caused by bicycle accidents (especially by impact with the handlebars) in children and vehicular accidents in adults, usually occur in isolation in children and accompanied by other injuries in adults.[6] Indications that the pancreas is injured include enlargement and the presence of fluid around the pancreas.[6]
Kidneys
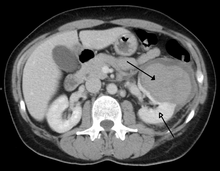
The kidneys may also be injured; they are somewhat but not completely protected by the ribs.[7] Kidney lacerations and contusions may also occur.[13] Kidney injury, a common finding in children with blunt abdominal trauma, may be associated with bloody urine.[13] Kidney lacerations may be associated with urinoma or leakage of urine into the abdomen.[6] A shattered kidney is one with multiple lacerations and an associated fragmentation of the kidney tissue.[6]
Bowel
The small intestine takes up a large part of the abdomen and is likely to be damaged in penetrating injury.[4] The bowel may be perforated.[6] Gas within the abdominal cavity seen on CT is understood to be a diagnostic sign of bowel perforation; however intra-abdominal air can also be caused by pneumothorax (air in the pleural cavity outside the lungs that has escaped from the respiratory system) or pneumomediastinum (air in the mediastinum, the center of the chest cavity).[6] The injury may not be detected on CT.[6] Bowel injury may be associated with complications such as infection, abscess, bowel obstruction, and the formation of a fistula.[6] Bowel perforation requires surgery.[6]
Diagnosis

One study found that ten percent of polytrauma patients who had no clinical signs of abdominal injury did have evidence of such injuries using radiological imaging.[2] Diagnostic techniques used include CT scanning, ultrasound,[2] and X-ray.[5] X-ray can help determine the path of a penetrating object and locate any foreign matter left in the wound, but may not be helpful in blunt trauma.[5] Diagnostic peritoneal lavage is a controversial technique but can be used to detect injury to abdominal organs: a catheter is placed in the peritoneal cavity, and if fluid is present, it is aspirated and examined for blood or evidence of organ rupture.[2] If this does not reveal evidence of injury, sterile saline is infused into the cavity and evacuated and examined for blood or other material.[2] While peritoneal lavage is an accurate way to test for bleeding, it carries a risk of injuring the abdominal organs, may be difficult to perform, and may lead to unnecessary surgery; thus it has largely been replaced by ultrasound in Europe and North America.[2] Ultrasound can detect fluid such as blood or gastrointestinal contents in the abdominal cavity,[2] and it is a noninvasive procedure and relatively safe for the patient.[6] CT scanning is the preferred technique for people who are not at immediate risk of shock, but since ultrasound can be performed right in an emergency room, the latter is recommended for people who are not stable enough to move to CT scanning.[2] However, people with abdominal trauma frequently need CT scans for other trauma (for example, head or chest CT); in these cases abdominal CT can be performed at the same time without wasting time in patient care.[6] Diagnostic laparoscopy or exploratory laparotomy may also be performed if other diagnostic methods do not yield conclusive results.[4]
CT
CT is only able to detect 76% of hollow viscous injuries and patients who have negative scans must often be observed and rechecked if they deteriorate.[14] However, CT has been demonstrated to be useful in screening patients with certain forms of abdominal trauma in order to avoid unnecessary laparotomies, which can significantly increase the cost and length of hospitalizations.[15] A meta-analysis of CT use in penetrating abdominal traumas demonstrated sensitivity, specificity and accuracy >= 95%, with a PPV of 85% and an NPV of 98%.[16] This suggests that CT is excellent for avoiding unnecessary laparotomies but must be augmented by other clinical criteria to determine the need for surgical exploration (23.37 positive likelihood ratio, 0.05 negative likelihood ratio).
Treatment
Initial treatment involves stabilizing the patient enough to ensure adequate airway, breathing, and circulation, and identifying other injuries.[5] Surgery may be needed to repair injured organs. Surgical exploration is necessary for people with penetrating injuries and signs of peritonitis or shock.[4] Laparotomy is often performed in blunt abdominal trauma,[2] and is urgently required if an abdominal injury causes a large, potentially deadly bleed.[4] The main goal is to stop any sources of bleeding before moving onto any definitive find and repair any injuries that are found.[17] Due to the time sensitive nature, this procedure also emphasizes expedience in terms of gaining access and controlling the bleeding, thus favoring a long midline incession.[18] Intra-abdominal injuries are also frequently successfully treated nonoperatively[5][6] as there is little benefit shown if there is no known active bleeding or potential for infection.[19] The use of CT scanning allows care providers to use less surgery because they can identify injuries that can be managed conservatively and rule out other injuries that would need surgery.[5] Depending on the injuries, a patient may or may not need intensive care.[6]
Prognosis
If abdominal injury is not diagnosed promptly, a worse outcome is associated.[2] Delayed treatment is associated with an especially high morbidity and mortality if perforation of the gastrointestinal tract is involved.[13]
Epidemiology
Most deaths resulting from abdominal trauma are preventable;[4] abdominal trauma is one of the most common causes of preventable, trauma-related deaths.[5]
References
- ↑ Fitzgerald, J.E.F.; Larvin, Mike (2009). "Chapter 15: Management of Abdominal Trauma". In Baker, Qassim; Aldoori, Munther. Clinical Surgery: A Practical Guide. CRC Press. pp. 192–204. ISBN 9781444109627.
- 1 2 3 4 5 6 7 8 9 10 11 Jansen JO, Yule SR, Loudon MA (April 2008). "Investigation of blunt abdominal trauma". BMJ. 336 (7650): 938–42. PMC 2335258
 . PMID 18436949. doi:10.1136/bmj.39534.686192.80.
. PMID 18436949. doi:10.1136/bmj.39534.686192.80.
- ↑ Wyatt, Jonathon; Illingworth, RN; Graham, CA; Clancy, MJ; Robertson, CE (2006). Oxford Handbook of Emergency Medicine. Oxford University Press. p. 346. ISBN 978-0-19-920607-0.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Hemmila MR, Wahl WL (2005). "Management of the Injured Patient". In Doherty GM. Current Surgical Diagnosis and Treatment. McGraw-Hill Medical. pp. 227–8. ISBN 0-07-142315-X. Retrieved 2008-06-21.
- 1 2 3 4 5 6 7 8 9 Yeo A (2004). "Abdominal trauma". In Chih HN, Ooi LL. Acute Surgical Management. World Scientific Publishing Company. pp. 327–33. ISBN 981-238-681-5. Retrieved 2008-06-21.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Bixby SD, Callahan MJ, Taylor GA (January 2008). "Imaging in pediatric blunt abdominal trauma". Semin Roentgenol. 43 (1): 72–82. PMID 18053830. doi:10.1053/j.ro.2007.08.009.
- 1 2 3 Lichtenstein R, Suggs AH (2006). "Child abuse/assault". In Olshaker JS, Jackson MC, Smock WS. Forensic Emergency Medicine: Mechanisms and Clinical Management (Board Review Series). Hagerstown, MD: Lippincott Williams & Wilkins. pp. 157–9. ISBN 0-7817-9274-6. Retrieved 2008-06-21.
- ↑ Chih, p.343
- 1 2 3 Hemmila, p. 231
- 1 2 Chih, pp. 346–348
- 1 2 3 4 Blank-Reid C (September 2006). "A historical review of penetrating abdominal trauma". Crit Care Nurs Clin North Am. 18 (3): 387–401. PMID 16962459. doi:10.1016/j.ccell.2006.05.007.
- ↑ Fabian TC, Bee TK (2004). "Liver and biliary trauma". In Moore EJ, Feliciano DV, Mattox KL. Trauma. New York: McGraw-Hill, Medical Pub. Division. p. 637. ISBN 0-07-137069-2. Retrieved 2008-06-21.
- 1 2 3 4 5 6 7 8 Visrutaratna P, Na-Chiangmai W (April 2008). "Computed tomography of blunt abdominal trauma in children" (PDF). Singapore Med J. 49 (4): 352–8; quiz 359. PMID 18418531.
- ↑ Amal Mattu; Deepi Goyal; Barrett, Jeffrey W.; Joshua Broder; DeAngelis, Michael; Peter Deblieux; Gus M. Garmel; Richard Harrigan; David Karras; Anita L'Italien; David Manthey (2007). Emergency medicine: avoiding the pitfalls and improving the outcomes. Malden, Mass: Blackwell Pub./BMJ Books. p. 61. ISBN 1-4051-4166-2.
- ↑ Demetriades D, Velmahos G, Cornell E 3rd, et al. Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg 1997; 132:178–183
- ↑ Goodman CS, Hur JY, Adajar MA, Coulam CH., How well does CT predict the need for laparotomy in hemodynamically stable patients with penetrating abdominal injury? A review and meta-analysis., AJR Am J Roentgenol. 2009 Aug;193(2):432-7.
- ↑ Moore. 2012. p. 517.
- ↑ Moore. 2012. p. 516.
- ↑ Oyo-Ita, Angela; Chinnock, Paul; Ikpeme, Ikpeme A. (2015-11-13). "Surgical versus non-surgical management of abdominal injury". The Cochrane Database of Systematic Reviews (11): CD007383. ISSN 1469-493X. PMID 26568111. doi:10.1002/14651858.CD007383.pub3.
Bibliography
- Feliciano, David V.; Mattox, Kenneth L.; Moore, Ernest J (2012). Trauma, Seventh Edition (Trauma (Moore)). McGraw-Hill Professional. ISBN 978-0-07-166351-9.
- Fitzgerald, J.E.F.; Larvin, Mike (2009). "Chapter 15: Management of Abdominal Trauma". In Baker, Qassim; Aldoori, Munther. Clinical Surgery: A Practical Guide. CRC Press. pp. 192–204. ISBN 9781444109627.